Transcutaneous pacing
| Transcutaneous pacing | |
|---|---|
| Other names: External pacing | |
 | |
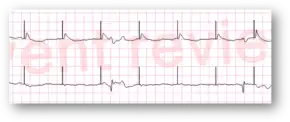
| True electrical and mechanical capture | |
| Specialty | Emergency medicine |
Transcutaneous pacing, also called external pacing, is a temporary means of pacing the heart which is most commonly used when the heart rate is less than 40 and the systolic blood pressure is less than 90.[1] This may occur in conditions such as third degree heart block.[1] Less commonly it may be used in atrial flutter after surgery or torsades de pointes when other measures are not effected.[1]
If time permits, hair at the pad location should be removed and the skin cleaned.[1] If the person is conscious, some sedation may be given to reduce discomfort.[1] The pacing pads are than placed on the chest, either in the anterior/lateral or anterior/posterior positions.[1] The rate on the machine is set at between 60 and 90 beats per minute and the current at its lowest level.[1] The current is than increased until pacer spikes are seen and than further until a QRS complex follows each spike.[1] The pulse is than checked to verify mechanical capture.[1]
Transcutaneous pacing is no longer indicated for the treatment of asystole (cardiac arrest associated with a "flat line" on the ECG).[2]
Medical uses
Transcutaneous pacing is most commonly used when the heart rate is less than 40 and the systolic blood pressure is less than 90.[1] This may occur due to a recent heart attack, trauma to the heart, infections such as Lyme disease or bacterial endocarditis, electrolyte problems, medications, and sepsis.[1] Less commonly it may be used in atrial flutter after surgery or torsades de pointes when other measures are not effected.[1]
Use is only recommended short term, with transvenous pacing being a more permanent solution.[1]
Contraindications
It is generally not used in people with only a slow heart rate but without symptoms or a low blood pressure.[1] Otherwise there are no contraindications.[1]
Technique
If time permits, hair at the location the pads will be placed should be removed and the skin cleaned with an alcohol wipe.[1] If the person is conscious, some sedation may be given to reduce discomfort.[1]
The pacing pads are than placed on the chest, either in the anterior/lateral or anterior/posterior positions.[1]
The rate on the machine should be set at between 60 and 90 beats per minute and the current at the lowest level.[1]
The current is than increased until pacer spikes are seen on the monitor and than further until a QRS complex follows each pacer spike.[1] The pulse is than checked to verify mechanical capture.[1] An ultrasound may be used to help verify mechanical capture.[1]
The pads are then attached to a monitor/defibrillator. Pacing artifact on the ECG and muscle twitching may make this determination difficult.
Trouble shooting
If pacer spike are not followed by a QRS complex the current should be increased.
Alternatives
Other forms of cardiac pacing are transvenous pacing, epicardial pacing,[4] and permanent pacing with an implantable pacemaker.
In addition to synchronized transcutaneous pacing, some machines have the option of asynchronous pacing. If ECG electrodes are not available or something interferes with adhesion to the skin and a person must be paced, asynchronous pacing may be used. This setting should only be used as a last resort due to possible adverse effects.
It differs from defibrillation (used in ventricular fibrillation or pulseless ventricular tachycardia) and cardioversion (used for atrial fibrillation or atrial fluuter; though all three generally use the same machine and pads.
Complications
Pacing results in a lower stroke volume and therefore a slightly higher heart rate is required.[1]
Other side effects may include skin burns and muscle spasms.[1] Skin burns occur more commonly in the very young and old.[1] It is theoretically possible that transcutaneous pacing may harm a previously implanted pacemaker.[1]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 Crofoot, Meagan; Sarwar, Ayesha; Weir, Alec J. "External pacemaker". StatPearls Publishing. PMID 30137851. Archived from the original on 10 March 2021. Retrieved 6 June 2022.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ GREGORATOS, GABRIEL. "ACC/AHA Guidelines for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices" (PDF). Archived from the original (PDF) on 2018-05-16. Retrieved 2019-10-14.
- ↑ "Transcutaneous Pacing (TCP): The Problem of False Capture". EMS 12 Lead. Archived from the original on 2019-02-01. Retrieved 2019-01-31.
- ↑ Batra AS, Balaji S (2008). "Post operative temporary epicardial pacing: When, how and why?". Ann Pediatr Cardiol. 1 (2): 120–05. doi:10.4103/0974-2069.43877. PMC 2840753. PMID 20300253.