Pericardiocentesis
| Pericardiocentesis | |
|---|---|
 | |
| Drawing of a pericardial effusion, needle pictured is not generally long enough. | |
| Specialty | Emergency medicine, cardiology |
| Indications | Pericardial tamponade[1] |
| Contraindications | None absolute[1] |
| Steps | 1) Verify tamponade on ultrasound 2) Sterilize and freeze the area around the xiphoid process 3) Just below and left of the xiphoid joining the ribs introduce the needle pointing towards the left shoulder 4) Pull back the plunger as you advance the needle 5) Once fluid comes back, take off the syringe and feed in a guidewire 6) Remove the needle and feed a dilator over the wire 7) Remove the dilator and place a pigtail drain 8) Remove the wire[2] |
| Success | Improved blood pressure[1] |
| Complications | Injury to the heart, arrhythmia, pneumothorax, injury to the liver[1] |
| Outcome | Depends on underlying cause[3] |
Pericardiocentesis (PCC), also called pericardial tap, is a procedure where fluid is removed from the envelope around the heart (pericardial sac).[1] Emergently it is most commonly carried out for pericardial tamponade resulting in low blood pressure.[1] Tamponade typically results from a stab wound to the chest rather than blunt trauma.[4] The procedure may also be done less urgently when a moderate effusion results in symptoms.[3]
To preform the procedure sterilize and freeze the area.[1][5] The needle is often inserted below the lower part of the sternum, through may be inserted through the front of the chest.[1] A 20g spinal needle with a 10 ml syringe or the needle from a central line kit may be used.[5] The path can be guided with an ultrasound.[1] The Seldinger technique can be used to leave a pigtail drain in place.[1][5]
Complications can include injury to the heart, arrhythmia, pneumothorax, and injury to the liver.[1] Placing a nasogastric tube to decompress the stomach before the procedure may lower the risk of stomach injury.[1] Signs of success include improved blood pressure and this generally occurs rapidly.[1][3] After the procedure the person may be brought to the operating room for further procedures such as a pericardial window or thoracotomy.[1] The procedure was first described in 1911 by Marfan.[3]
Medical uses
Cardiac tamponade
Pericardiocentesis can be used to diagnose and treat cardiac tamponade.[6][7] Cardiac tamponade is a medical emergency in which excessive accumulation of fluid within the pericardium (pericardial effusion) creates increased pressure.[8] This prevents the heart from filling normally with blood. This can critically decrease the amount of blood that is pumped from the heart. The removal of the excess fluid reverses this, and is often the first treatment for cardiac tamponade due to the short time in which it can be performed.[8]
Other uses
In those with a moderate or large amount of fluid that is resulting in symptoms and does not improve after medical treatment pericardiocentesis may be carried out.[3] It may also be done for smaller effusions due to a bacterial infection.[3]
Analysis of fluid
Pericardiocentesis is not generally recommended for diagnostic purposes alone.[3] If the effusion dose not result in symptoms and is less than 20 mm in thickness during diastole, the risks of the procedure do not generally out way the usefulness of the information acquired by testing.[3]
Contraindications
Long-term drainage
Pericardiocentesis is a one-off procedure, which is not appropriate for long-term drainage. In cases where longer term drainage is needed, a surgeon can create a pericardial window. This involves the removal of a section of the pericardium, and the placement of a chest tube.
Aortic dissection
Pericardiocentesis may be carried out in cardiac tamponade due to aortic dissection but only a small amount of fluid to bring the systolic blood pressure up to about 90 mmHg is recommended.[3] The person needs definitive surgery to manage this complications.[3]
Technique
Preparation
The person undergoing pericardiocentesis is generally positioned on their back with the head of the bed raised to about 30 degrees.[1][3] If time permits, a nasogastric tube to decompress the stomach is recommended to lower the risk of stomach injury.[1] It is preferable to avoid intubating and ventilating a person before the procedure as doing so may decrease their blood pressure further.[3]
There are three main locations pericardiocentesis can be performed:[3]
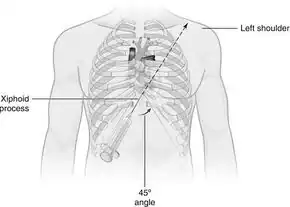
- The most standard location is through the infrasternal angle, also called subxiphoid approach.[8][9] The needle is inserted at an angle between 30 and 45 degrees to the chest.[10] Once under the ribs the angle is decreased to 15 to 30 degrees.[3]
- Another location is through the 5th or 6th intercostal space at the left sternal border at the cardiac notch of the left lung, and is also called as parasternal approach.[10] The needle is inserted at an angle of 90 degrees to the chest.[10] Some evidence suggests that this poses lower risk of vascular damage in adults.[10]
- The needle is placed about one finger width lateral to the apex of the heart. Generally this in the 5th to 7th intercostal space.[3]
Steps
Pericardiocentesis is often performed using local anaesthetic.[12] A wide-bore catheter is inserted.[12]
Steps for below the xiphoid process:[2] 1) Verify tamponade on ultrasound 2) Sterilize and freeze the area around the xiphoid process 3) Just below and left of the were the xiphoid joins the ribs introduce the needle pointing towards the left shoulder 4) Pull back the plunger as you advance the needle 5) Once fluid comes back, take off the syringe and feed in a guidewire 6) Remove the needle and feed a dilator over the wire 7) Remove the dilator and place a pigtail 8) Remove the wire
Pericardiocentesis is generally done under ultrasound guidance to minimize complications.[12] An electrocardiogram (ECG) is also continuously recorded to assess for complications.[8]
Equipment
Besides having an ECHO machine one needs sterile drapes, local anesthetic, syringes, needles, scalpel and a pericardiocentesis kit.[1] An alligator clip connector may be used to connect the V1 lead to the ECG machine.[1]
Post-procedure
If the blood aspirated does not clot it is likely to be from the pericardial sac, while if it does lot it is likely to be from the ventricle of the heart.[11]
Following the removal of a small amount of fluid the persons hemodynamics generally improves rapidly.[3] A chest X-ray should be take to verify that no pneumothorax has occurred.[3] Antibiotics are not needed routinely.[3] Longer term outcomes often depend on the underlying cause.[3]
Complications
Fewer than 1.5% of people experience complications from pericardiocentesis.[13] The most common complications are lacerations of coronary arteries, and puncture of the left ventricle (with associated bleeding from both).[13][14] Echocardiograms can help to identify complications.[14] Blind approaches are typically only advised in emergencies, and a guided approach is typically preferred (using echocardiography).[14][12]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Willner, DA; Grossman, SA (January 2021). "Pericardiocentesis". PMID 29261871.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Roberts and Hedges' clinical procedures in emergency medicine and acute care (Seventh ed.). Philadelphia, PA: Elsevier Health Sciences. 2019. pp. 309–331. ISBN 9780323547949.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Carlini, Caterina Chiara De; Maggiolini, Stefano (11 October 2017). "Pericardiocentesis in cardiac tamponade: indications and practical aspects". www.escardio.org. 15 (19). Archived from the original on 10 March 2021. Retrieved 17 March 2021.
- ↑ Surgical care at the district hospital (PDF). Geneva: World Health Organization. 2003. p. PTCM-18. ISBN 9241545755. Archived (PDF) from the original on 27 January 2018. Retrieved 16 March 2021.
- 1 2 3 Nagdev, Arun (22 August 2013). "Ultrasound-Guided Pericardiocentesis". ALiEM. Archived from the original on 25 October 2020. Retrieved 16 March 2021.
- ↑ Gupta, Pooja; Ibrahim, Amar; Butany, Jagdish (2014-01-01), Willis, Monte S.; Homeister, Jonathon W.; Stone, James R. (eds.), "Chapter 16 - The Pericardium and its Diseases", Cellular and Molecular Pathobiology of Cardiovascular Disease, San Diego: Academic Press, pp. 297–314, doi:10.1016/b978-0-12-405206-2.00016-8, ISBN 978-0-12-405206-2, archived from the original on 2021-08-28, retrieved 2020-12-03
- ↑ Jneid, Hani; Maree, Andrew O.; Palacios, Igor F. (2008-01-01), Parrillo, Joseph E.; Dellinger, R. Phillip (eds.), "Chapter 6 - Pericardial Tamponade: Clinical Presentation, Diagnosis, and Catheter-Based Therapies", Critical Care Medicine (Third Edition), Philadelphia: Mosby, pp. 85–92, doi:10.1016/b978-032304841-5.50008-x, ISBN 978-0-323-04841-5, archived from the original on 2021-02-10, retrieved 2020-12-03
- 1 2 3 4 Fashoyin-Aje, Lola A.; Brahmer, Julie R. (2020-01-01), Niederhuber, John E.; Armitage, James O.; Kastan, Michael B.; Doroshow, James H. (eds.), "59 - Malignancy-Related Effusions", Abeloff's Clinical Oncology (Sixth Edition), Philadelphia: Elsevier, pp. 863–873.e4, doi:10.1016/b978-0-323-47674-4.00059-1, ISBN 978-0-323-47674-4, archived from the original on 2020-12-11, retrieved 2020-12-03
- ↑ "Pericardiocentesis". Archived from the original on 7 March 2016.
- 1 2 3 4 Steele, Robert; Thorp, Andrea (2008-01-01), Baren, Jill M.; Rothrock, Steven G.; Brennan, John A.; Brown, Lance (eds.), "Chapter 180 - Pericardiocentesis", Pediatric Emergency Medicine, Philadelphia: W.B. Saunders, pp. 1259–1262, ISBN 978-1-4160-0087-7, archived from the original on 2021-08-28, retrieved 2020-11-16
- 1 2 "Pericardiocentesis • LITFL • CCC Procedure". Life in the Fast Lane • LITFL. 30 January 2019. Archived from the original on 23 January 2021. Retrieved 17 March 2021.
- 1 2 3 4 Balmanoukian, Ani; Brahmer, Julie R. (2011-01-01), Davis, Mellar P.; Feyer, Petra Ch.; Ortner, Petra; Zimmermann, Camilla (eds.), "32 - Pleural and pericardial effusions", Supportive Oncology, Saint Louis: W.B. Saunders, pp. 354–361, doi:10.1016/b978-1-4377-1015-1.00032-1, ISBN 978-1-4377-1015-1, archived from the original on 2021-08-28, retrieved 2020-12-03
- 1 2 Sorajja, Paul (2018-01-01), Kern, Morton J.; Sorajja, Paul; Lim, Michael J. (eds.), "17 - Pericardiocentesis", The Interventional Cardiac Catheterization Handbook (Fourth Edition), Elsevier, pp. 438–447, doi:10.1016/b978-0-323-47671-3.00017-x, ISBN 978-0-323-47671-3, archived from the original on 2021-08-28, retrieved 2020-11-16
- 1 2 3 Sovari, Ali S. (2019-01-01), Brown, David L. (ed.), "44 - Pericardiocentesis", Cardiac Intensive Care (Third Edition), Philadelphia: Elsevier, pp. 461–464.e1, doi:10.1016/b978-0-323-52993-8.00044-8, ISBN 978-0-323-52993-8, archived from the original on 2020-11-08, retrieved 2020-11-16
External links
| Classification | |
|---|---|
| External resources |