Pericardial effusion
| Pericardial effusion | |
|---|---|
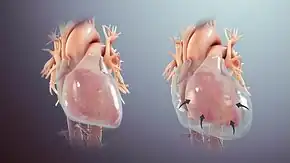
.gif) | |
| A 2D transthoracic echocardiogram of a massive pericardial effusion. The "swinging" heart | |
| Specialty | Cardiac surgery |
| Symptoms | Chest pain, shortness of breath, tiredness[1] |
| Complications | Cardiac tamponade[1] |
| Usual onset | Sudden, gradual[1] |
| Types | Transudate, exudate, bloody[1] |
| Diagnostic method | Ultrasound of the heart[1] |
| Differential diagnosis | Pericarditis, pulmonary edema, dilated cardiomyopathy, constrictive pericarditis, pulmonary embolism[1] |
| Treatment | Conservative management, pericardiocentesis[1] |
| Frequency | Relatively common[1] |
Pericardial effusion is an abnormal accumulation of fluid in the pericardial space around the heart.[1] Symptoms may include chest pain, shortness of breath, and tiredness.[1] Onset may be sudden or gradual.[1] Complications may include cardiac tamponade with low blood pressure, fast heart rate, jugular venous distension, and distant heart sounds.[1]
In the developed world the most common cause is viral pericarditis.[1] Other causes include infections, autoimmune disorders, cancer, trauma, following a heart attack, thoracic aortic dissection, kidney failure, low thyroid, and cirrhosis.[1] Diagnosis is confirmed by ultrasound of the heart.[1] Normal levels of pericardial fluid are from 15 to 50 ml.[1]
Treatment depends on the underlying cause, size of the effusion, and a person's symptoms.[1] Small effusions may be managed conservatively while large effusions may be treated with pericardiocentesis.[1] Pericardial effusions are relatively common.[1] They were first described around 200 AD by Galen.[2]
Signs and symptoms
Chest pain or pressure are common symptoms. A small effusion may be asymptomatic. Larger effusions may cause cardiac tamponade, a life-threatening complication; signs of impending tamponade include dyspnea, low blood pressure, and distant heart sounds.
It can be associated with dullness to percussion over the left subscapular area due to compression of the left lung base. This phenomenon is known as Ewart's sign.[3]
Causes
- Pericarditis
- Viral infection (coxsackie virus)
- Infection including tuberculosis
- Drug eluting stents
- Inflammatory disorders, such as lupus, rheumatoid arthritis[4] and post myocardial infarction pericarditis (Dressler's syndrome)
- Cancer that has spread to the pericardium such as breast and lung cancer. Pericardial irregular thickening and/or nodularity, focal, or diffuse FDG uptake on PET scan and lack of preserved fat plane with an adjacent tumor are strongly suggestive of cancer spread from other parts of the body.[5]
- Trichinosis
- Kidney failure with excessive blood levels of urea nitrogen
- Minoxidil
- Hypothyroidism
- Heart surgery[6] (Postpericardiotomy syndrome)
- Primary tumor - The most common primary pericardial tumour is mesothelioma. Various imaging appearances such as solid and cystic components could be encountered on CT scan on those with mesothelioma. Other less common primary tumours are sarcoma, ly,phoma, and primitive neuroectodermal tumour.[5]
Pathophysiology
How much fluid is stored in the pericardial sac at one particular time is based on the balance between production and reabsorption. Studies have shown that much of the fluid that accumulates in the pericardial sac is from plasma filtration of the epicardial capillaries and a small amount from the myocardium, while the fluid that is drained is mostly via the parietal lymphatic capillaries. [7] Pericardial effusion usually results from a disturbed equilibrium between these two processes or from a structural abnormality that allows excess fluid to enter the pericardial cavity.[7] Because of the limited amount of anatomic space in the pericardial cavity and the limited elasticity of the pericardium, fluid accumulation beyond the normal amount leads to an increased intrapericardial pressure which can negatively affect heart function.
A pericardial effusion with enough pressure to adversely affect heart function is called cardiac tamponade.[3] Pericardial effusions can cause cardiac tamponade in acute settings with fluid as little as 150mL. In chronic settings, however, fluid can accumulate anywhere up to 2L before an effusion causes cardiac tamponade. The reason behind this is the elasticity of the pericardium. When fluid fills the cavity rapidly, the pericardium cannot stretch rapidly, but in chronic effusions, the gradual fluid collection provides the pericardium enough time to accommodate and stretch with the increasing fluid levels.[8]
Diagnosis
It may be:
- transudative (congestive heart failure, myxoedema, nephrotic syndrome),
- exudative (tuberculosis, spread from empyema)
- bloody (trauma, rupture of aneurysms, malignant effusion).
- malignant (due to fluid accumulation caused by metastasis)
The most common causes of pericardial effusion have changed over time and vary depending on geography and the population in question. When pericardial effusion is suspected, echocardiography usually confirms the diagnosis and allows assessment for signs of hemodynamic instability. Cross-sectional imaging with computed tomography (CT) can help to localize and quantify (as in a loculated effusion) or assess for pericardial pathology (pericardial thickening, constrictive pericarditis).[9]
The so-called "water-bottle heart" is a radiographic sign of pericardial effusion, in which the cardiopericardial silhouette is enlarged and assumes the shape of a flask or water bottle.
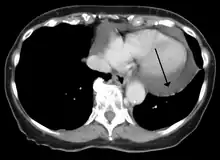 A CT scan image showing a pericardial effusion
A CT scan image showing a pericardial effusion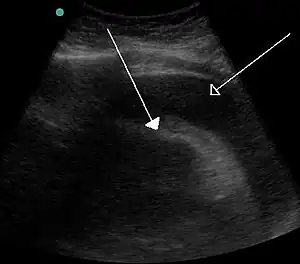 A very large hemorrhagic pericardial effusion due to malignancy as seen on ultrasound. closed arrow: the heart, open arrow: the effusion
A very large hemorrhagic pericardial effusion due to malignancy as seen on ultrasound. closed arrow: the heart, open arrow: the effusion Pericardial effusion due to malignancy. Note bulbous heart and primary lung cancer in right upper lobe.
Pericardial effusion due to malignancy. Note bulbous heart and primary lung cancer in right upper lobe.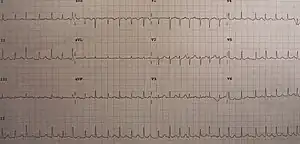 An ECG showing sinus tachycardia and electrical alternans in a person with a pericardial effusion.
An ECG showing sinus tachycardia and electrical alternans in a person with a pericardial effusion. A pericardial effusion due to pericarditis
A pericardial effusion due to pericarditis- Loculated pericardial effusion[10]
Treatment

Treatment depends on the underlying cause and the severity of the heart impairment. Pericardial effusion due to a viral infection usually goes away within a few weeks without the treatment. Some pericardial effusions remain small and never need treatment. If the pericardial effusion is due to a condition such as lupus, treatment with anti-inflammatory medications may help. If the effusion is compromising heart function and causing cardiac tamponade, it will need to be drained, most commonly by a needle inserted through the chest wall and into the pericardial space called pericardiocentesis. A drainage tube is often left in place for several days. In some cases, surgical drainage may be required by cutting through the pericardium creating a pericardial window.
Other animals

Serous exsudates are seen at necropsy in various diseases of domestic animals, like enterotoxemia in sheep or fowl cholera.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Willner, DA; Goyal, A; Grigorova, Y; Kiel, J (January 2020). "Pericardial Effusion". PMID 28613741.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Marx, John; Hockberger, Robert; Walls, Ron (2013). Rosen's Emergency Medicine - Concepts and Clinical Practice E-Book: 2-Volume Set. Elsevier Health Sciences. p. 1091. ISBN 978-1-4557-4987-4. Archived from the original on 2021-08-28. Retrieved 2021-02-16.
- 1 2 "Pericardial Disease". Archived from the original on 2008-12-02.
- ↑ Hallewell RA, Sherratt DJ (1976). "Isolation and characterization of Co1E2 plasmid mutants unable to kill colicin-sensitive cells". Mol Gen Genet. 146 (3): 239–45. doi:10.1007/bf00701246. PMID 794689.
- 1 2 Ünal, Emre; Karcaaltincaba, Musturay; Akpinar, Erhan; Ariyurek, Orhan Macit (December 2019). "The imaging appearances of various pericardial disorders". Insights into Imaging. 10 (1): 42. doi:10.1186/s13244-019-0728-4. ISSN 1869-4101. PMC 6441059. PMID 30927107. Archived from the original on 2020-07-24. Retrieved 2020-07-24.
- ↑ Pericardial effusion:What are the symptoms? Archived 2007-07-06 at the Wayback Machine, Dr. Martha Grogan M.D.
- 1 2 Vogiatzidis, Konstantinos et al. “Physiology of pericardial fluid production and drainage Archived 2020-11-12 at the Wayback Machine.” Frontiers in physiology vol. 6 62. 18 Mar. 2015, doi:10.3389/fphys.2015.00062
- ↑ Willner, Daniel A.; Goyal, Amandeep; Grigorova, Yulia; Kiel, John (2020), "Pericardial Effusion", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 28613741, archived from the original on 2022-04-05, retrieved 2020-11-12
- ↑ Chang, S (Jul–Sep 2014). "Brief Images: Massive pericardial effusion". Images in Paediatric Cardiology. 16 (3): 1–3. PMC 4521324. PMID 26236369.
- ↑ "UOTW #25 - Ultrasound of the Week". Ultrasound of the Week. 11 November 2014. Archived from the original on 9 May 2017. Retrieved 27 May 2017.
External links
- Pericardial Disease Archived 2019-03-16 at the Wayback Machine Cleveland Clinic Online Medical Reference
| Classification | |
|---|---|
| External resources |