Sinus bradycardia
| Sinus bradycardia | |
|---|---|
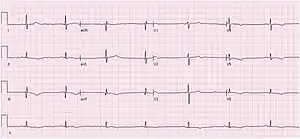 | |
| ECG of Sinus bradycardia with a heart rate of 43 bpm. | |
| Specialty | Cardiology |
| Symptoms |
|
| Diagnostic method | electrocardiogram |
Sinus bradycardia is a sinus node dysfunction with a rate that is lower than normal. In humans, bradycardia is generally defined to be a rate of under 60 beats per minute.[1] A normal heartbeat in human is usually at a rate of 60 to 100 beats per minute.[2]
Signs and symptoms
The decreased heart rate can cause a decreased cardiac output resulting in symptoms such as lightheadedness, dizziness, hypotension, vertigo, and syncope.[3] The slow heart rate may also lead to atrial, junctional, or ventricular ectopic rhythms.
Bradycardia is not necessarily problematic. People who practice sports may have sinus bradycardia, because their trained hearts can pump enough blood in each contraction to allow a low resting heart rate.[4] Sinus bradycardia can also be an adaptive advantage; for example, diving seals may have a heart rate as low as 12 beats per minute, helping them to conserve oxygen during long dives.[5]
Sinus bradycardia is a common condition found in both healthy individuals and those who are considered well-conditioned athletes.[6]
Heart rates considered bradycardic vary by species; for example, in the house cat, a rate of under 120 beats per minute is abnormal. Generally, smaller species have higher and larger species lower rates.[7]
Cause
Sinus bradycardia is commonly seen in normal healthy persons and athletes in the absence of pathophysiological diseases or conditions.[1]Different factors or etiologies could lead to the dysfunction of the sinus node, causing a malformation or prolongation of the impulse.
In terms of pathophysiological diseases, sinus rhythm may be caused by:
- Diseases/Conditions:
- Acute myocardial infarction, carotid sinus syndrome, eating disorders (such as anorexia nervosa), rhodotoxin poisoning, hypothermia, hypothyroidism, infections (such as diphtheria, acute rheumatic fever, or viral myocarditis), intrinsic disease of the SA node (such as sick sinus syndrome), Roemheld syndrome, sleep apnea
- Physiological causes:
- Increased vagal tone, increased intracranial pressure
- Medications, most commonly: digitalis glycosides, beta-blockers, quinidine, adenosine, calcium channel blockers, class I antiarrhythmic agents, ivabradine, clonidine, reserpine, cimetidine, lithium, amitriptyline
Diagnosis
 Rhythm strip of sinus bradycardia at 50 bpm
Rhythm strip of sinus bradycardia at 50 bpm.png.webp) EKG shows a sinus bradycardia at 40 bpm with a first-degree atrio-ventricular block
EKG shows a sinus bradycardia at 40 bpm with a first-degree atrio-ventricular block
Diagnosis of sinus bradycardia can be confirmed by an electrocardiogram that shows the following characteristics:[1]
- Rate: Less than 60 beats per minute.
- Rhythm: Regular.
- P waves: Upright, consistent, and normal in morphology and duration.
- PR interval: Between 0.12 and 0.20 seconds in duration.
- QRS complex: Less than 0.12 seconds in width, and consistent in morphology.[8]
Taking a thorough medical history and physical exam by healthcare providers can also help with narrowing differential diagnosis. Any recent changes to patient's medication history, new symptoms such as chest pain, shortness of breath and palpitations, family history of sinus bradycardia, physical exam that reveals cyanosis, peripheral edema, altered mental status, dyspnea, rales and crackles are all relevant information to consider for differential diagnosis.[1]
Treatment
In terms of management the affected individual may be treated with intravenous atropine 0.5 mg every 3-5 minutes (3 mg total)[1]
See also
References
- 1 2 3 4 5 Hafeez Y, Grossman SA (2020). "Sinus Bradycardia". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 29630253. Archived from the original on 2021-08-27. Retrieved 2020-07-27.
- ↑ "Sinus Bradycardia". Cedars-Sinai. Archived from the original on 2020-05-08. Retrieved 2020-07-28.
- ↑ "Bradycardia - Signs and Symptoms | CardioSmart – American College of Cardiology". CardioSmart. Archived from the original on 2021-07-25. Retrieved 2022-05-17.
- ↑ "Why Do Athletes Have a Lower Resting Heart Rate?". Healthline. 2020-04-21. Archived from the original on 2022-05-17. Retrieved 2022-05-17.
- ↑ Thornton SJ, Hochachka PW (2004). "Oxygen and the diving seal" (PDF). Undersea & Hyperbaric Medicine : Journal of the Undersea and Hyperbaric Medical Society, Inc. 31 (1): 81–95. PMID 15233163. Archived (PDF) from the original on 2019-07-14. Retrieved 2022-05-17.
- ↑ Salyer SW (2007). "Chapter 2 - Cardiology". In Salyer SW (ed.). Essential emergency medicine: for the healthcare practitioner. Saunders/Elsevier. pp. 37–96. ISBN 978-1-4160-2971-7.
- ↑ Milani-Nejad N, Janssen PM (March 2014). "Small and large animal models in cardiac contraction research: advantages and disadvantages". Pharmacology & Therapeutics. 141 (3): 235–49. doi:10.1016/j.pharmthera.2013.10.007. PMC 3947198. PMID 24140081.
- ↑ "Electrocardiogram Waves". en.my-ekg.com. Archived from the original on 2022-02-02. Retrieved 2022-05-17.
External links
| Classification |
|---|