Left bundle branch block
| Left bundle branch block | |
|---|---|
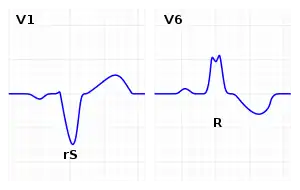 | |
| ECG characteristics of a typical LBBB showing wide QRS complexes with abnormal morphology in leads V1 and V6. | |
| Specialty | Cardiology, emergency medicine |
| Symptoms | None[1] |
| Duration | Long-term[1] |
| Causes | Unknown, dilated cardiomyopathy, amyloidosis[1] |
| Diagnostic method | Electrocardiogram (ECG)[1] |
| Differential diagnosis | Intraventricular conduction delay, artificial pacemaker, run of PVCs[1] |
| Treatment | Based on underlying disorder[1] |
| Frequency | Common[1] |
Left bundle branch block (LBBB) is a type of electrical conduction abnormality of the heart seen on the electrocardiogram (ECG).[1] In and of itself, it results in no symptoms.[1] The condition is generally permanent.[1]
Causes include dilated cardiomyopathy, such as may occur following a heart attack, valvular heart disease, or heart failure and amyloidosis.[1] Though some cases occurs without any specific cause.[1] The underlying mechanism involves abnormal conduction down both anterior and posterior left fascicles of the His-Purkinje system.[1]
Diagnosis requires four conditions: the rhythm is supraventricular, the QRS is greater than 120 ms, lead V1 has a QS or a small r with a large S wave, and lead V6 has a notched R and no Q wave.[1] When the QRS duration is less than 120 ms, but the other criteria are present, it is called an incomplete LBBB.[1] New onset LBBB together with chest pain was previously, but is no longer considered, a STEMI equivalent.[2] Rather it is recommended the Sgarbossa criteria be applied.[1]
No specific treatment is generally required.[1] Management is directed at the underlying cause, which determines the outcomes.[1] LBBB is common, affected about 1 in 1,000 people.[1] About 33% of those with heart failure are affected.[1] Those affected are not permitted to fly an aircraft in the United States or United Kingdom.[1]
Signs and symptoms
In and of itself, it results in no symptoms.[1]
Causes
Among the causes of LBBB are:
- Aortic stenosis
- Dilated cardiomyopathy
- Acute myocardial infarction
- Extensive coronary artery disease
- Primary disease of the cardiac electrical conduction system
- Long standing hypertension leading to aortic root dilatation and subsequent aortic regurgitation
- Lyme disease
- Side effect of some cardiac surgeries (e.g., aortic root reconstruction)
Diagnosis
The criteria to diagnose a left bundle branch block on the electrocardiogram:
- The heart rhythm must be supraventricular in origin
- The QRS duration must be ≥ 120 ms[3]
- There should be a QS or rS complex in lead V1
- There should be a notched ('M'-shaped) R wave in lead V6.
The T wave should be deflected opposite the terminal deflection of the QRS complex. This is known as appropriate T wave discordance with bundle branch block. A concordant T wave may suggest ischemia or myocardial infarction.
There are also partial blocks of the left bundle branch: "left anterior fascicular block" (LAFB)[4] and a "left posterior fascicular block" (LPFB).[5] This refers to the block after the bifurcation of the left bundle branch.
The presence of LBBB results in an ECG that cannot be used to diagnose left ventricular hypertrophy or Q wave infarction, because LBBB in itself results in widened QRS complex, and changes in the ST segment consistent with ischemia or injury.[6]
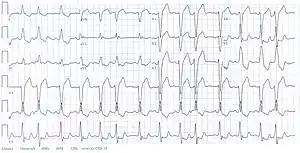 Electrocardiogram showing left bundle branch block and irregular rhythm due to supraventricular extrasystoles.
Electrocardiogram showing left bundle branch block and irregular rhythm due to supraventricular extrasystoles.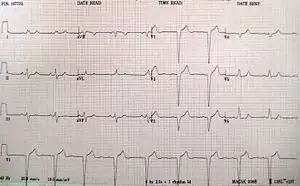 A left bundle branch block
A left bundle branch block
Treatment
No specific treatment is generally required.[1] Management is directed at the underlying cause.[1]
- People with LBBB require complete cardiac evaluation, and those with LBBB and syncope or near-syncope may require a pacemaker.
- Some people with LBBB, a markedly prolonged QRS (usually > 150 ms), and systolic heart failure may benefit from a biventricular pacemaker, which allows for better synchrony of heart contractions.[7]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Scherbak, D; Hicks, GJ (January 2020). "Left Bundle Branch Block". PMID 29489192.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Roberts, David. Mastering the 12-Lead EKG. Springer Publishing Company. p. 434. ISBN 978-0-8261-8194-7. Archived from the original on 2021-08-28. Retrieved 2020-12-30.
- ↑ "Lesson VI - EKG Conduction Abnormalities". Archived from the original on 2019-12-16. Retrieved 2009-01-07.
- ↑ "more detailed information about left anterior fascicular block". GPnotebook.
- ↑ "more detailed information about left posterior fascicular block". GPnotebook.
- ↑ Emily Groepper; Nasar Nallamothu; Wilfred Lam; Frank Aguirre; Kristi Bergman; Patricia Good; Patricia Wright (May 13, 2014). "Electrocardiography > Left Bundle Branch Block (LBBB)". Southern Illinois University School of Medicine. Archived from the original on 2019-04-11. Retrieved 2015-07-02.
- ↑ Stevenson WG, Hernaddez AF, Carson PE, et al. Indications for cardiac resynchronization therapy: 2011 update from the Heart Failure Society of America guideline committee. J Card Fail 2012; 18:94-106.
External links
| Classification | |
|---|---|
| External resources |