Constrictive pericarditis
| Constrictive pericarditis | |
|---|---|
| Other names: Pericarditis - constrictive[1] | |
 | |
| Constrictive pericarditis is defined by a fibrotic (thickened) pericardium. | |
| Symptoms | Fatigue[1] |
| Causes | Tuberculosis, Heart surgery[1] |
| Diagnostic method | CT scan, MRI[1] |
| Treatment | Diuretic, Antibiotics[1] |
Constrictive pericarditis is a medical condition characterized by a thickened, fibrotic pericardium, limiting the heart's ability to function normally.[1] In many cases, the condition continues to be difficult to diagnose and therefore benefits from a good understanding of the underlying cause.[2]
Signs and symptoms
Signs and symptoms of constrictive pericarditis are consistent with the following: fatigue, swollen abdomen, difficulty breathing (dyspnea), swelling of legs and general weakness. Related conditions are bacterial pericarditis, pericarditis and pericarditis after a heart attack.[1]
Causes
The cause of constrictive pericarditis in the developing world are idiopathic in origin, though likely infectious in nature. In regions where tuberculosis is common, it is the cause in a large portion of cases.[3] Causes of constrictive pericarditis include:
- Tuberculosis[4]
- Incomplete drainage of purulent pericarditis[4]
- Fungal and parasitic infections[4]
- Chronic pericarditis[4]
- Postviral pericarditis[4]
- Postsurgical[4]
- Following MI, post-myocardial infarction[4]
- In association with pulmonary asbestos[5]
Pathophysiology

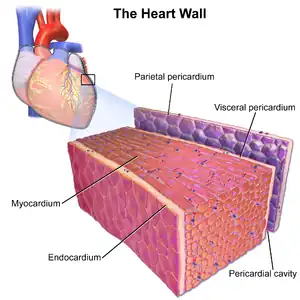
The pathophysiological characteristics of constrictive pericarditis are due to a thickened, fibrotic pericardium that forms a non-compliant shell around the heart. This shell prevents the heart from expanding when blood enters it. This results in significant respiratory variation in blood flow in the chambers of the heart.[6]
During inspiration, pressure in the thoracic cavity decreases but is not relayed to the left atrium, subsequently a reduction in flow to the left atrium and ventricle happens. During diastole, less blood flow in left ventricle allows for more room for filling in right ventricle and therefore a septal shift occurs.[7]
During expiration, the amount of blood entering the left ventricle will increase, allowing the interventricular septum to bulge towards the right ventricle, decreasing the right heart ventricular filing.[8]
Diagnosis
The diagnosis of constrictive pericarditis is often difficult to make. In particular, restrictive cardiomyopathy has many similar clinical features to constrictive pericarditis, and differentiating them in a particular individual is often a diagnostic dilemma.[9]
- Chest X-Ray - pericardial calcification (common but not specific), pleural effusions are common findings.[10]
- Echocardiography - the principal echographic finding is changes in cardiac chamber volume.[10]
- CT and MRI - CT scan is useful in assessing the thickness of pericardium, calcification, and ventricular contour. Cardiac MRI may find pericardial thickening and pericardial-myocardial adherence. Ventricular septum shift during breathing can also be found using cardiac MRI. Late gadolinium enhancement can show enhancement of the pericardium due to fibroblast proliferation and neovascularization.[8]
- BNP blood test - tests for the existence of the cardiac hormone brain natriuretic peptide, which is only present in restrictive cardiomyopathy but not in constrictive pericarditis[11]
- Conventional cardiac catheterization[12]
- Physical examination - can reveal clinical features including Kussmaul's sign and a pericardial knock.[12]
.png.webp) Hepatic vein flows; expiratory diastolic flow reversal characteristic feature in constrictive pericarditis is suspected
Hepatic vein flows; expiratory diastolic flow reversal characteristic feature in constrictive pericarditis is suspected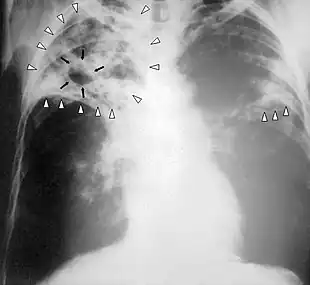 Tuberculosis-x-ray
Tuberculosis-x-ray
Treatment
The definitive treatment for constrictive pericarditis is pericardial stripping, which is a surgical procedure where the entire pericardium is peeled away from the heart. This procedure has significant risk involved,[13] with mortality rates of 6% or higher in major referral centers.[14]
A poor outcome is almost always the result after a pericardiectomy is performed for constrictive pericarditis whose origin was radiation-induced, further some patients may develop heart failure post-operatively.[15]
References
- 1 2 3 4 5 6 7 "Contrictive pericarditis". Medline Plus. NIH. Archived from the original on 6 September 2015. Retrieved 21 September 2015.
- ↑ Schwefer, Markus; Aschenbach, Rene; Heidemann, Jan; Mey, Celia; Lapp, Harald (September 2009). "Constrictive pericarditis, still a diagnostic challenge: comprehensive review of clinical management". European Journal of Cardio-Thoracic Surgery. 36 (3): 502–510. doi:10.1016/j.ejcts.2009.03.004. PMID 19394850.
- ↑ Dunn, Brian (2013). Manual of cardiovascular medicine (4th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 653. ISBN 978-1-4511-3160-4. Archived from the original on 12 October 2022. Retrieved 21 September 2015.
- 1 2 3 4 5 6 7 "Constritive pericarditis". eMedicine. MedScape. Archived from the original on 5 September 2015. Retrieved 21 September 2015.
- ↑ Lloyd, Joseph (2013). Mayo Clinic cardiology : concise textbook (4th ed.). Oxford: Mayo Clinic Scientific Press/Oxford University Press. p. 718. ISBN 978-0-199915712. Archived from the original on 12 October 2022. Retrieved 21 September 2015.
- ↑ Crouch, Michael A. (2010). Cardiovascular pharmacotherapy : a point-of-care guide. Bethesda, Md.: American Society of Health-System Pharmacists. p. 376. ISBN 978-1-58528-215-9. Archived from the original on 12 October 2022. Retrieved 21 September 2015.
- ↑ Camm, Demosthenes G. Katritsis, Bernard J. Gersh, A. John (2013). Clinical cardiology : current practice guidelines (1st ed.). Oxford: Oxford University Press. p. 388. ISBN 978-0-19-968528-8. Archived from the original on 12 October 2022. Retrieved 21 September 2015.
- 1 2 Welch, Terrence D.; Oh, Jae K. (November 2017). "Constrictive Pericarditis". Cardiology Clinics. 35 (4): 539–549. doi:10.1016/j.ccl.2017.07.007. PMID 29025545.
- ↑ "Restrictive pericarditis". eMedicine. MedScape. Archived from the original on 30 September 2015. Retrieved 21 September 2015.
- 1 2 "Imaging in Constrictive pericarditis". eMedicine. MedScape. Archived from the original on 5 September 2015. Retrieved 21 September 2015.
- ↑ Semrad, Michal (2014). Cardiovascular Surgery. Charles University. p. 114. ISBN 978-80-246-2465-5. Archived from the original on 12 October 2022. Retrieved 21 September 2015.
- 1 2 Khandaker, Masud H.; Espinosa, Raul E.; Nishimura, Rick A.; Sinak, Lawrence J.; Hayes, Sharonne N.; Melduni, Rowlens M.; Oh, Jae K. (June 2010). "Pericardial Disease: Diagnosis and Management". Mayo Clinic Proceedings. 85 (6): 572–593. doi:10.4065/mcp.2010.0046. PMC 2878263. PMID 20511488.
- ↑ Cinar B, Enc Y, Goksel O, Cimen S, Ketenci B, Teskin O, Kutlu H, Eren E (2006). "Chronic constrictive tuberculous pericarditis: risk factors and outcome of pericardiectomy". Int J Tuberc Lung Dis. 10 (6): 701–6. PMID 16776460.
- ↑ Chowdhury UK, Subramaniam GK, Kumar AS, Airan B, Singh R, Talwar S, Seth S, Mishra PK, Pradeep KK, Sathia S, Venugopal P (2006). "Pericardiectomy for constrictive pericarditis: a clinical, echocardiographic, and hemodynamic evaluation of two surgical techniques". Ann Thorac Surg. 81 (2): 522–9. doi:10.1016/j.athoracsur.2005.08.009. PMID 16427843.
- ↑ Greenberg, Barry H. (2007). Congestive heart failure (3rd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 410. ISBN 978-0-7817-6285-4. Archived from the original on 12 October 2022. Retrieved 21 September 2015.
Further reading
- Hoit, B. D. (25 June 2002). "Management of Effusive and Constrictive Pericardial Heart Disease". Circulation. 105 (25): 2939–2942. doi:10.1161/01.CIR.0000019421.07529.C5. PMID 12081983. Archived from the original on 23 July 2017. Retrieved 21 September 2015.
External links
| Classification | |
|---|---|
| External resources |