Trichosporon asteroides
| Trichosporon asteroides | |
|---|---|
 | |
| Scientific classification | |
| Kingdom: | |
| Division: | Basidiomycota |
| Class: | Tremellomycetes |
| Order: | Tremellales |
| Genus: | |
| Species: | T. asteroides |
| Binomial name | |
| Trichosporon asteroides M. Ota (1926) | |
| Synonyms | |
| |
Trichosporon asteroides is an asexual Basidiomycetous fungus first described from human skin but is now mainly isolated from blood and urine.[1][2][3][4][5] T. asteroides is a hyphal fungus with a characteristically yeast-like appearance due to the presence of slimy arthroconidia.[3][6] Infections by this species usually respond to treatment with azoles and amphotericin B.[2][7][8]
History and taxonomy
Trichosporon asteroides was isolated from lesion of male chin skin by Rinchin in Berne in 1926 and named in the genus, Parendomyces. T. asteroides was later reevaluated by Masao Ota and transferred to the genus Trichosporon as T. asteroides.[1] Ota noted that its hyphae were more sparsely branched than other species in Trichosporon, and it lacked the ability to ferment glucose, maltose, sucrose and fructose.[1] Molecular phylogenetic study has since supported the placement of T. asteroides in the genus Trichsporon.[9] T. asteroides was determined to be conspecific with Fissuricella filamenta on the basis of DNA/DNA reassociation.[3][6] Modern classifications support the affiliation of this species with the order Tremellales in the phylum Basidiomycota.[10]
Growth and morphology
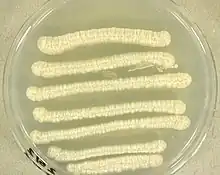
T. asteroides grows in a range of media including in the presence of the antifungal agent, cycloheximide.[4] Colonies of T. asteroides grown on Sabouraud agar appear white in colour with a brain-like texture, reaching a diameter of 10 mm after 10 days growth at 25 °C (77 °F).[3][6] Colonies have radially furrowed outer zone and matt appearance that is not powdery like the related species, T. asahii.[3] Antibodies produced by infected patients can also be used to differentiate T. asahii and T. asteroides in disease.[11] Weak growth is seen at 37 °C (99 °F) but is absent at higher temperatures.[6][10] T. asteroides can be distinguish with other relative species in the genus Trichosporon by its ability to utilize D-galactose, L-rhamnose, erythritol and L-arabinitol.[3]
Physiology and pathogenesis
T. asteroides does not ferment glucose, maltose, sucrose or fructose, this is the common feature to all the species in Trichosporon.[1] T. asteroides causes trichosporonosis, which mainly responsible for deep-seated, mucosa-associated, superficial, and systematic infections including blood.[2][4][6][12][13] This species is one of the three most common Trichosporon species isolated in clinical settings.[12] The fungus is sometimes recovered from specimens of blood, urine, and aspiration fluid, vaginal mucosa, male perigenital skin area, and catheters.[4][14][5] The first record of this agent in a systemic infection involved a bloodstream infection.[4] Some main types of latent infection can be raised are fungemia, urinary tract infections, peritonitis, endocarditis, arthritis, esophagitis, meningitis, brain abscess, splenic abscess, and uterine infections.[2] Allergies and systemic infections can also be caused by this fungus particularly in immunosuppressed people.[15] Recently, T. asteroides was implicated in a case of kerion celsi, a rare, highly inflammatory scalp infection seen mainly in children.[16]
This fungus is rarely encountered in zoonotic infections[15] and has never been shown to cause disease un insects.[12] However, T. asteroides was isolated from the multifocal, irregularly raised skin lesions on a female Bottle-Nosed Dolphin, Tursiops truncatus, in Japan.[15] In the absence of cultures and molecular biological analysis, the agent was initially suspected to be Paracoccidioides ceti, a worldwide causative agent of Paracoccidioidomycosis in dolphins.[15]
Treatment
Azole antifungals are often used as a front-line therapy in trichosporonosis.[7] Resistance to amphotericin, flucytosine, fluconazole, and itraconazole have been described.[8][2] Echinocandins, as a group, are ineffective against Trichosporon species.[6] Triazoles show better in vitro and in vivo antifungal activity than amphotericin B, while voriconazole also has excellent in vitro activity against Trichosporon asteroides.[2][8][17] Combination therapy regimens such as voriconazole and amphotericin B are also effective in serious infections.[17] Fluconazole has been used successfully in subcutaneous and deep infections.[16]
References
- 1 2 3 4 Masao, Ota (1926). "Sur quelques champignons pathogènes du type Trichosporum beigeli Vuillemin". Annales de Parasitologie Humaine et Comparée. 4 (1): 1–13. doi:10.1051/parasite/1926041001.
- 1 2 3 4 5 6 Colombo, A. L.; Padovan, A. C. B.; Chaves, G. M. (2011). "Current Knowledge of Trichosporon spp. and Trichosporonosis". Clinical Microbiology Reviews. 24 (4): 682–700. doi:10.1128/CMR.00003-11. PMC 3194827. PMID 21976604.
- 1 2 3 4 5 6 Guého, E.; Smith, M. T.; De Hoog, G. S.; Billon-Grand, G.; Christen, R.; van der Vegte, W. B. (1992). "Contributions to a revision of the genus Trichosporon". Antonie van Leeuwenhoek. 61 (4): 289–316. doi:10.1007/BF00713938. PMID 1497334. S2CID 24841877.
- 1 2 3 4 5 Kustimur, Semra; Kalkanci, Ayse; Caglar, Kayhan; Dizbay, Murat; Aktas, Firdevs; Sugita, Takashi (2002). "Nosocomial fungemia due to Trichosporon asteroides: firstly described bloodstream infection". Diagnostic Microbiology and Infectious Disease. 43 (3): 167–170. doi:10.1016/S0732-8893(02)00385-1. PMID 12088626.
- 1 2 Silvestre Junior, Agenor Messias; Miranda, Mauricio Alexandre Bandeira Rampazzo; Camargo, Zoilo Pires de (2010). "Trichosporon species isolated from the perigenital region, urine and catheters of a Brazilian population". Brazilian Journal of Microbiology. 41 (3): 628–34. doi:10.1590/S1517-83822010000300013. PMC 3768649. PMID 24031538.
- 1 2 3 4 5 6 Guého, Eveline; Improvisi, Luce; Dupont, B.; De Hoog, G. S. (1994). "Trichosporon on humans: a practical account: Trichosporon am Menschen: Eine Darstellung für die Praxis". Mycoses. 37 (1–2): 3–10. doi:10.1111/j.1439-0507.1994.tb00277.x. PMID 7935589. S2CID 24703812.
- 1 2 Anaissie, E.; Gokaslan, A.; Hachem, R.; Rubin, R.; Griffin, G.; Robinson, R.; Sobel, J.; Bodey, G. (1992). "Azole Therapy for Trichosporonosis: Clinical Evaluation of Eight Patients, Experimental Therapy for Murine Infection, and Review". Clinical Infectious Diseases. 15 (5): 781–787. doi:10.1093/clind/15.5.781. ISSN 1058-4838. PMID 1445976.
- 1 2 3 Garg, Vaibhav; Jones, Elizabeth K.; Friedman, Ben J.; Lee, Jason B.; Yang, Sherry (2018). "Invasive trichosporonosis treated with voriconazole". JAAD Case Reports. 4 (4): 362–364. doi:10.1016/j.jdcr.2017.11.003. ISSN 2352-5126. PMC 5911819. PMID 29693071.
- ↑ Sugita, Takashi; Nakase, Takashi (1998). "Molecular phylogenetic study of the basidiomycetous anamorphic yeast genus Trichosporon and related taxa based on small subunit ribosomal DNA sequences". Mycoscience. 39 (1): 7–13. doi:10.1007/BF02461572. S2CID 83647795.
- 1 2 Howard, Dexter H. (2007). Pathogenic fungi in humans and animals (2nd ed.). New York: Marcel Dekker. ISBN 9780203909102.
- ↑ Davies, Genna E.; Thornton, Christopher R. (2014). "Differentiation of the emerging human pathogens Trichosporon asahii and Trichosporon asteroides from other pathogenic yeasts and moulds by using species-specific monoclonal antibodies". PLOS ONE. 9 (1): e84789. doi:10.1371/journal.pone.0084789. PMC 3879316. PMID 24392156.
- 1 2 3 Mariné, Marçal; Bom, Vinicius Leite Pedro; Castro, Patricia Alves de; Winkelstrote, Lizziane Kretli; Ramalh, Leandra Naira; Brown, Neil Andrew; Goldman, Gustavo Henrique (2015). "The development of animal infection models and antifungal efficacy assays against clinical isolates of Trichosporon asahii, T. asteroides and T. inkin". Virulence. 6 (5): 476–86. doi:10.1080/21505594.2015.1020273. PMC 4601256. PMID 25751127.
- ↑ Sugita, T; Nishikawa, A; Shinoda, T (1998). "Rapid detection of species of the opportunistic yeast Trichosporon by PCR". Journal of Clinical Microbiology. 36 (5): 1458–60. doi:10.1128/JCM.36.5.1458-1460.1998. PMC 104855. PMID 9574732.
- ↑ Paula, Claudete R.; Krebs, Vera L. J.; Auler, Marcos E.; Ruiz, Luciana S.; Matsumoto, Flavia E.; Silva, Elza H.; Diniz, Edna M. A.; Vaz, Flavio A. C. (2006). "Nosocomial infection in newborns by in a Brazilian intensive care unit". Medical Mycology. 44 (5): 479–484. doi:10.1080/13693780600561809. PMID 16882616.
- 1 2 3 4 Ueda, Keiichi; Nakamura, Ichiro; Itano, Eiko Nakagawa; Takemura, Kazunori; Nakazato, Yasutomo; Sano, Ayako (2017). "Trichosporon asteroides Isolated from Cutaneous Lesions of a Suspected Case of "paracoccidioidomycosis ceti" in a Bottlenose Dolphin (Tursiops truncatus)". Mycopathologia. 182 (9–10): 937–946. doi:10.1007/s11046-017-0147-3. PMID 28547342. S2CID 11893217.
- 1 2 Kocabaş, Bilge Aldemİr; Karbuz, Adem; Çİftçİ, Ergin; Beğde, Fırat; Ametoglou, Selver; Fouad, Ali Adil; Kalkancı, Ayşe; Karahan, Zeynep Ceren; Aysev, Derya; İnce, Erdal (2016). "Trichosporon asteroides: A novel etiologic agent of Kerion celsi in a child" (PDF). İzmir Dr. Behçet Uz Çocuk Hastanesi Dergisi. 6 (2): 151–154.
- 1 2 Maxfield, Luke; Matthews, Juliana J.; Ambrosetti, David Ryan; Ephtimios, Issa E. (2015). "Trichosporon fungemia in a pediatric patient with acute lymphoblastic leukemia". IDCases. 2 (4): 106–108. doi:10.1016/j.idcr.2015.09.007. ISSN 2214-2509. PMC 4712209. PMID 26793473.