Urethral cancer
| Urethral cancer[1] | |
|---|---|
| Other names: Primary urethral cancer | |
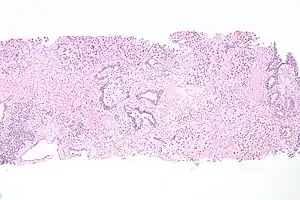 | |
| Micrograph of urethral cancer, urothelial cell carcinoma, found on a prostate core biopsy. H&E stain. | |
| Specialty | Oncology urology |
| Symptoms | Blood in the urine, lump at end of penis, bloody urethral discharge[1][2] |
| Complications | Urinary retention, priapism[1][3] |
| Usual onset | 73 years[4] |
| Types | Urothelial carcinoma, squamous cell cancer, adenocarcinoma[1] |
| Risk factors | Prolonged urinary catheterization, chronic infection, radiation, diverticula of the urethra, urethral strictures[1] |
| Diagnostic method | Transurethral biopsy[1] |
| Treatment | Surgery, radiation therapy, chemotherapy[1] |
| Prognosis | Often poor[4] |
| Frequency | Rare[1] |
Urethral cancer is cancer originating from the urethra.[1] Symptoms may include blood in the urine, lump at end of penis, pain with sex, or bloody discharge.[1][2] Complications may include urinary retention and priapism.[3]
Risk factors may include prolonged irritations from urinary catheterization, chronic inflammation due to infection, radiation, diverticula of the urethra, or urethral strictures.[1] The most common types are urothelial carcinoma, squamous cell cancer, and adenocarcinoma.[1] Diagnosis is established by transurethral biopsy.[1] The disease is classified by the TNM staging system and the World Health Organization.[1][5]
Treatment may include a combination of surgery, radiation therapy, and chemotherapy.[1] Outcomes are often poor with a five-year survival rate of 46%.[4] Urethral cancer is rare, representing less than 1% of cancers.[1] About 4.3 cases occur per million males and 1.5 cases per million females in the United States.[4] The typical age at diagnosis is 73.[4]
Signs and symptoms
Symptoms that may be caused by urethral cancer include:
- Blood visible in urine.[1]
- Bloody urethral discharge.[2]
- Weak or interrupted flow of urine.
- Urination occurs often, painful urination, inability to pass urine.
- A lump or thickness in the perineum or penis.[1]
- Enlarged lymph nodes or pain in the groin or vaginal area.
Diagnosis
Diagnosis is established by transurethral biopsy and histological findings.[1] Bladder cystoscopy is performed to detect if there is simultaneous bladder cancer.[1]
Histology
Types of urethral cancer include the most common type urothelial carcinoma, and others including squamous cell carcinoma, and adenocarcinoma. Melanoma and sarcoma are rare.[1]
Staging
The World Health Organization classification of tumours of the urinary system and male genital organs (4th edn) was published in January 2016.[5] Urethral cancer has also been classified by the TNM staging system.[6]
| T-category | Description |
|---|---|
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| Urethra (male and female) | |
| Ta | Noninvasive papillary, polypoid, or verrucous carcinoma |
| Tis | Carcinoma in situ |
| T1 | Tumor invades subepithelial connective tissue |
| T2 | Tumor invades any of the following: corpus spongiosum, prostate, periurethral muscle |
| T3 | Tumor invades any of the following: corpus cavernosum, beyond prostatic capsule, anterior vagina, bladder neck (extraprostatic extension) |
| T4 | Tumor invades other adjacent organs (invasion of the bladder) |
| Urothelial (transitional cell) carcinoma of the prostate | |
| Tis pu | Carcinoma in situ, involvement of prostatic urethra |
| Tis pd | Carcinoma in situ, involvement of prostatic ducts |
| T1 | Tumor invades subepithelial connective tissue (for tumors involving prostatic urethra only) |
| T2 | Tumor invades any of the following: prostatic stroma, corpus spongiosum, periurethral muscle |
| Ta | Noninvasive papillary, polypoid, or verrucous carcinoma |
| T3 | Tumor invades any of the following: corpus cavernosum, beyond prostatic capsule, bladder neck (extraprostatic extension) |
| T4 | Tumor invades other adjacent organs (invasion of the bladder or rectum) |
| N—regional lymph nodes | |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in a single lymph node |
| N2 | Metastasis in multiple lymph nodes |
| M—Distant Metastasis | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
Treatment
Surgery is the most common treatment for cancer of the urethra.[7] One of the following types of surgery may be done: open excision, electro-resection with flash, laser surgery, cystourethrectomy, cystoprostatectomy, anterior body cavity, or incomplete or basic penectomy surgery.
Radiation therapy has also been used in some cases.[1]
Chemotherapy is sometimes used to destroy urethral cancer cells. It is a systemic urethral cancer treatment (i.e., destroys urethral cancer cells throughout the body) that is administered orally or intravenously. Medications are often used in combination to destroy urethral cancer that has metastasized. Commonly used drugs include cisplatin, vincristine, and methotrexate.
Side effects include anemia (causing fatigue, weakness), nausea and vomiting, loss of appetite, hair loss, mouth sores, increased risk for infection, shortness of breath, or excessive bleeding and bruising.[8]
Epidemiology
Primary urethral cancer is rare and contributes to less than 1% of all cancers. It is three times more common in men than women and its incidence rises after the age of 75.[1]
Around half of affected people have locally advanced disease when they first present.[1] 54–65% of cases are of the urothelial carcinoma type.[1]
Prolonged irritations of the urethra due to urinary catheterization, chronic inflammation due to infection, radiation, diverticula of the urethra, and urethral strictures, may increase the risk of primary urethral cancer.[1] Other risk factors include squamous cell carcinoma (SCC) and genital lichen sclerosus.[1]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 Janisch, Florian; Abufaraj, Mohammad; Fajkovic, Harun; Kimura, Shoji; Iwata, Takehiro; Nyirady, Peter; Rink, Michael; Shariat, Shahrokh F. (1 September 2019). "Current Disease Management of Primary Urethral Carcinoma". European Urology Focus. 5 (5): 722–734. doi:10.1016/j.euf.2019.07.001. ISSN 2405-4569. Archived from the original on 27 August 2021. Retrieved 27 December 2020.
- 1 2 3 Kahan, Scott; Miller, Redonda; Smith, Ellen G. (2008). "126. Penile Discharge". Signs and Symptoms. Lippincott Williams & Wilkins. ISBN 978-0-7817-7043-9. Archived from the original on 29 April 2021. Retrieved 27 December 2020.
- 1 2 Nargund, Vinod H.; Raghavan, Derek; Sandler, Howard M. (2015). Urological Oncology. Springer. p. 174. ISBN 978-0-85729-482-1. Archived from the original on 27 August 2021. Retrieved 28 December 2020.
- 1 2 3 4 5 Grivas, PD; Davenport, M; Montie, JE; Kunju, LP; Feng, F; Weizer, AZ (December 2012). "Urethral cancer". Hematology/oncology clinics of North America. 26 (6): 1291–314. doi:10.1016/j.hoc.2012.08.006. PMID 23116581.
- 1 2 3 Compérat, Eva; Varinot, Justine (2016). "Immunochemical and molecular assessment of urothelial neoplasms and aspects of the 2016 World Health Organization classification". Histopathology. 69 (5): 717–726. doi:10.1111/his.13025. ISSN 1365-2559.
- 1 2 Brierley, James D.; Gospodarowicz, Mary K.; Wittekind, Christian (2017). "Urological Tumours". TNM Classification of Malignant Tumours (8th ed.). John Wiley & Sons. p. 208. ISBN 978-1-119-26354-8. Archived from the original on 27 August 2021. Retrieved 27 December 2020.
- ↑ Pagliaro, Lance. Rare Genitourinary Tumors. Springer. p. 157. ISBN 978-3-319-30046-7. Archived from the original on 27 August 2021. Retrieved 27 December 2020.
- ↑ "Urethral Cancer Treatment". Archived from the original on 19 January 2021. Retrieved 14 March 2022.
External links
| Classification |
|
|---|---|
| External resources |