Vancomycin-resistant Enterococcus
| Vancomycin-resistant Enterococcus | |
|---|---|
| Other names: Vancomycin-resistant enterococci | |
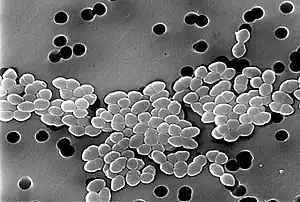 | |
| SEM micrograph of vancomycin-resistant enterococci | |
| Specialty | Microbiology |
| Prevention | Screen with peri-rectal swab[1] |
| Treatment | Linezolid [2] |
Vancomycin-resistant Enterococcus, or vancomycin-resistant enterococci (VRE), are bacterial strains of the genus Enterococcus that are resistant to the antibiotic vancomycin.[3]
Mechanism of acquired resistance
Six different types of vancomycin resistance are shown by enterococcus: Van-A, Van-B, Van-C, Van-D, Van-E and Van-G.[4] The significance is that Van-A VRE is resistant to both vancomycin and teicoplanin,[5] Van-B VRE is resistant to vancomycin but susceptible to teicoplanin,[6][7] and Van-C is only partly resistant to vancomycin.
The mechanism of resistance to vancomycin found in enterococcus involves the alteration of the peptidoglycan synthesis pathway.[8] The D-alanyl-D-lactate variation results in the loss of one hydrogen-bonding interaction (four, as opposed to five for D-alanyl-D-alanine) being possible between vancomycin and the peptide. The D-alanyl-D-serine variation causes a six-fold loss of affinity between vancomycin and the peptide, likely due to steric hindrance.[9][10]
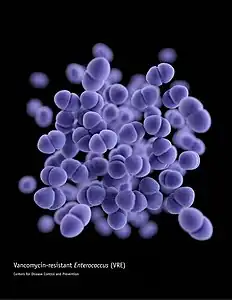 This illustration depicts a three-dimensional (3D) computer-generated image of a cluster of paired, or diplococcal, vancomycin-resistant Enterococcus (VRE) bacteria. The artistic recreation was based upon scanning electron microscopic (SEM) imagery.
This illustration depicts a three-dimensional (3D) computer-generated image of a cluster of paired, or diplococcal, vancomycin-resistant Enterococcus (VRE) bacteria. The artistic recreation was based upon scanning electron microscopic (SEM) imagery. Vancomycin
Vancomycin
Diagnosis
Once the individual has VRE, it is important to ascertain which strain.[11]
Screening
Screening for VRE can be accomplished in a number of ways. For inoculating peri-rectal/anal swabs or stool specimens directly, one method uses bile esculin azide agar plates containing 6 μg/ml of vancomycin. Black colonies should be identified as an enterococcus to species level and further confirmed as vancomycin resistant by an MIC method before reporting as VRE.[1]
Vancomycin resistance can be determined for enterococcal colonies available in pure culture by inoculating a suspension of the organism onto a commercially available brain heart infusion agar (BHIA) plate containing 6 μg/ml vancomycin. The National Committee for Clinical Laboratory Standards (NCCLS) recommends performing a vancomycin MIC test and also motility and pigment production tests to distinguish species with acquired resistance (vanA and vanB) from those with vanC intrinsic resistance.[1] Detection of vancomycin resistance by the use of PCR targeting vanA and vanB can also be performed.
Treatment of infection
Ceftriaxone (a third generation cephalosporin) use is a risk factor for colonization and infection by VRE, and restriction of cephalosporin usage has been associated with decreased VRE infection and transmission in hospitals.[12] Lactobacillus rhamnosus GG (LGG), a strain of L. rhamnosus, was used successfully for the first time to treat gastrointestinal carriage of VRE.[13] In the US, linezolid is commonly used to treat VRE.[2]
History
To become vancomycin-resistant, vancomycin-sensitive enterococci typically obtain new DNA in the form of plasmids or transposons which encode genes that confer vancomycin resistance.[14] This acquired vancomycin resistance is distinguished from the natural vancomycin resistance of certain enterococcal species including E. gallinarum and E. casseliflavus/flavescens.[15][16]
High-level vancomycin-resistant E. faecalis and E. faecium are clinical isolates first documented in the 1980s.[17] In the United States, vancomycin-resistant E. faecium was associated with 4% of healthcare-associated infections reported to the Centers for Disease Control and Prevention National Healthcare Safety Network from January 2006 to October 2007.[18] VRE can be carried by healthy people who have come into contact with the bacteria, usually in a hospital[19] (nosocomial infection),[20] although it is thought that a significant percentage of intensively farmed chickens also carry VRE.[21] Other regions have noted a similar distribution, but with increased incidence of VRE. For example, a 2006 study of nosocomial VRE revealed a rapid spread of resistance among enterococci along with an emerging shift in VRE distribution in the Middle East region, such as Iran. Treatment failures in enterococcal infections result from inadequate information regarding glycopeptide resistance of endemic enterococci due to factors such as the presence of VanA and VanB. The study from Iran reported the first case of VRE isolates that carried VanB gene in enterococcal strains from Iran. This study also noted the first documented isolation of nosocomial E. raffinosus and E. mundtii in the Middle East region.[22]
See also
- Methicillin-resistant Staphylococcus aureus (MRSA)(Vancomycin intermediate-resistant Staphylococcus aureus redirect)
- Antibiotic resistance
- Drug resistance
- MDR-TB
References
- 1 2 3 "Vancomycin-resistant Enterococci (VRE) and the Clinical Laboratory". Centers for Disease Control and Prevention. Archived from the original on 14 April 2019. Retrieved 21 May 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 Balli, Eleni P.; Venetis, Chris A.; Miyakis, Spiros (2014). "Systematic Review and Meta-Analysis of Linezolid versus Daptomycin for Treatment of Vancomycin-Resistant Enterococcal Bacteremia". Antimicrobial Agents and Chemotherapy. 58 (2): 734–739. doi:10.1128/AAC.01289-13. ISSN 0066-4804. PMC 3910884. PMID 24247127.
- ↑ "Vancomycin-resistant Enterococci (VRE) in Healthcare Settings". VRE in Healthcare Settings - HAI. CDC. Archived from the original on 2019-05-18. Retrieved 2015-06-09.
- ↑ Fong, I. W.; Drlica, Karl (2007-11-15). Antimicrobial Resistance and Implications for the 21st Century. Springer Science & Business Media. ISBN 9780387724188. Archived from the original on 2021-12-11. Retrieved 2021-11-25.
- ↑ Mendez-Vilas, A. (2011). Science and Technology Against Microbial Pathogens: Research, Development and Evaluation, Proceedings of the International Conference on Antimicrobial Research (ICAR2010), Valladolid, Spain 3 - 5 November 2010. World Scientific. ISBN 9789814354868.
- ↑ Ahmad, Iqbal; Aqil, Farrukh (2008-11-21). New Strategies Combating Bacterial Infection. John Wiley & Sons. ISBN 9783527622948.
- ↑ Grayson, M. Lindsay; Crowe, Suzanne M.; McCarthy, James S.; Mills, John; Mouton, Johan W.; Norrby, S. Ragnar; Paterson, David L.; Pfaller, Michael A. (2010-10-29). Kucers' The Use of Antibiotics Sixth Edition: A Clinical Review of Antibacterial, Antifungal and Antiviral Drugs. CRC Press. ISBN 9781444147520. Archived from the original on 2021-12-11. Retrieved 2021-11-25.
- ↑ Arias, Cesar A.; Murray, Barbara E. (2012). "Figure 4 : The rise of the Enterococcus: beyond vancomycin resistance : Nature Reviews Microbiology". Nature Reviews Microbiology. 10 (4): 266–278. doi:10.1038/nrmicro2761. PMC 3621121. PMID 22421879.
- ↑ Meziane-Cherif, Djalal; Saul, Frederick A.; Haouz, Ahmed; Courvalin, Patrice (2012). "Structural and Functional Characterization of VanG d-Ala:d-Ser Ligase Associated with Vancomycin Resistance in Enterococcus faecalis♦". The Journal of Biological Chemistry. 287 (45): 37583–37592. doi:10.1074/jbc.M112.405522. ISSN 0021-9258. PMC 3488035. PMID 22969085.
- ↑ Coates, Anthony R. M. (2012-08-31). Antibiotic Resistance. Springer Science & Business Media. ISBN 9783642289507. Archived from the original on 2021-12-11. Retrieved 2021-11-25.
- ↑ "Vancomycin-Resistant Enterococci (VRE) Diagnosis | NIH: National Institute of Allergy and Infectious Diseases". www.niaid.nih.gov. Archived from the original on 2017-03-25. Retrieved 2017-03-24.
- ↑ McKinnell, James A.; Kunz, Danielle F.; Chamot, Eric; Patel, Mukesh; Shirley, Rhett M.; Moser, Stephen A.; Baddley, John W.; Pappas, Peter G.; Miller, Loren G. (2012). "Association of Vancomycin-Resistant Enterococcus Bacteremia and Ceftriaxone Usage". Infection Control and Hospital Epidemiology. 33 (7): 718–724. doi:10.1086/666331. ISSN 0899-823X. PMC 3879097. PMID 22669234.
- ↑ Phoenix, David A.; Harris, Frederick; Dennison, Sarah R. (2014-08-25). Novel Antimicrobial Agents and Strategies. John Wiley & Sons. ISBN 9783527676156.
- ↑ Gould, Dinah; Brooker, Christine (2008-08-20). Infection Prevention and Control: Applied Microbiology for Healthcare. Palgrave Macmillan. ISBN 9781137045928.
{{cite book}}: CS1 maint: url-status (link) - ↑ Monticelli J, et al. (2018). "Clinical management of non-faecium non-faecalis vancomycin-resistant enterococci infection. Focus on Enterococcus gallinarum and Enterococcus casseliflavus/flavescens". J Infect Chemother. 24 (4): 237–246. doi:10.1016/j.jiac.2018.01.001. PMID 29396199.
- ↑ "VRE and the Clinical Laboratory - HAI". Healthcare-associated Infections. CDC. Archived from the original on 2019-04-14. Retrieved 2015-06-09.
- ↑ Robinson, D. Ashley; Feil, Edward J.; Falush, Daniel (2010-03-16). Bacterial Population Genetics in Infectious Disease. John Wiley & Sons. ISBN 9780470600115.
- ↑ Hidron AI, Edwards JR, Patel J, et al. (November 2008). "NHSN annual update: antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006-2007". Infect Control Hosp Epidemiol. 29 (11): 996–1011. doi:10.1086/591861. PMID 18947320.
- ↑ "Diseases and Organisms in Healthcare Settings". Healthcare-associated Infections (HAIs). CDC. Archived from the original on 2015-07-08. Retrieved 2015-06-09.
- ↑ Kouchak, Farideh; Askarian, Mehrdad (2012). "Nosocomial Infections: The Definition Criteria". Iranian Journal of Medical Sciences. 37 (2): 72–73. PMC 3470069. PMID 23115435.
- ↑ Nilsson, Oskar (2012). "Vancomycin resistant enterococci in farm animals – occurrence and importance". Infection Ecology & Epidemiology. 2: 16959. doi:10.3402/iee.v2i0.16959. PMC 3426332. PMID 22957131.
- ↑ Fathollahzadeh, Bahram; Hashemi, Farhad B.; Emaneini, Mohammad; Aligholi, Marzieh; Nakhjavani, Farrokh A. (2006). "Frequency of Vancomycin-Resistant Enterococci from Three Hospitals in Iran" (PDF). Daru. 14 (3): 141–146. Archived from the original on 2016-03-04. Retrieved 2015-12-30.
Further reading
- Rastall, Bob; Gibson, Glenn (2006-05-01). Prebiotics: Development and Application. John Wiley & Sons. ISBN 9780470023143. Archived from the original on 2021-12-11. Retrieved 2021-11-25.
External links
| Classification | |
|---|---|
| External resources |