This article was co-authored by Eric Baron, DO. Dr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
There are 15 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 83% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 100,683 times.
The spine has a long hollow space inside it that contains your spinal cord. Spinal headaches occur in up to 40 percent of people who undergo a spinal tap or spinal anesthesia. During both procedures, the membrane surrounding the spinal cord is punctured, and if spinal fluid leaks through the tiny puncture site, you may develop a spinal headache. Most spinal headaches go away on their own with no treatment. If your spinal headache lasts longer than 24 hours, you can take steps to address it at home, or visit the doctor to treat severe, chronic headache.
Steps
Coping At Home
-
1Consume caffeine to constrict the blood vessels in your head. Caffeine is a central nervous system stimulant and causes constriction of the blood vessels within your head.[1]
- Since headache is often caused by the dilatation of blood vessels, caffeine helps constrict them and counteract this effect.
- Caffeine can be taken both orally and intravenously.
- A recommended dose of caffeine is 500mg once or twice daily.
- A simple way to get caffeine is to drink coffee; one cup of coffee contains 50-100mg of caffeine. So, you should drink 5-8 cups of coffee daily to get an optimum result.
-
2Take simple painkillers. Using simple painkillers, like acetaminophen and other NSAIDs is a simple, but effective way to knock back headaches.[2]
- Acetaminophen and other NSAIDs provide temporary relief from headache by blocking the production of chemicals that are responsible for producing the pain sensation in the brain.
- Take 500mg of acetaminophen or acetaminophen+caffeine three times per day, after eating a meal.
- Use other non‐steroidal anti‐inflammatory drugs (NSAIDs) like ibuprofen (400mg 2-3 times daily after meal).
- Consult your doctor before any longterm usage of pain medications.
- Nowadays, you can buy NSAIDs that also contain caffeine for a more pronounced headache relief effect. Caffeine constricts blood vessels within your head, so you get the cumulative effect of both the painkiller and the caffeine.
- Do not forget to take an anti-peptic drug with these pain relievers to protect your stomach lining. Take omeprazole, pantoprazole, or esomeprazole at a dosage of 20 mg twice daily, 30 minutes before your meal.
Advertisement -
3Drink plenty of fluid to increase your blood volume. Drinking lots of fluids, especially water, will increase your blood volume and the fluid content of other parts of your body.[3]
- A portion of consumed water will go into the spinal space and increase its volume and pressure.
- Increased pressure will reduce spinal headache.
- Drink at least 3 liters (0.8 US gal) of fluid daily to keep yourself hydrated.
-
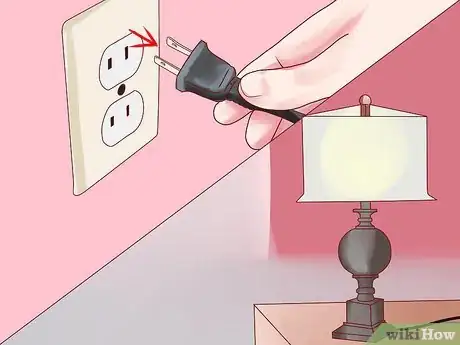
4Turn off or dim the lights. Most people suffering from headaches are sensitive to light, so it can help to turn them off or dim them.[4]
- Overly lighted rooms or bright lights aggravate headache because the brain is unable to mediate the glare and light during an episode of headache.
-
5Use visual imagery and distraction to reduce your focus on pain. Visual imagery is done by focusing on a picture or image of pleasant scenery or events.
- Another way to practice visual imagery is by repeating positive words or phrases.
- Distraction techniques are done by focusing your attention on positive mental thoughts and activities.
- These activities include watching television, listening to music, or talking to family.
- Distraction and visual imagery help a person divert attention from the pain to other positive activities.
-
6Lie down to increase pressure in your spine. Bed rest usually has no intrinsic role in reducing spinal headache, but lying vertically does.[5]
- When you are lying in bed, it can increase the pressure in your spine and reduce headache.
-
7Position yourself on your abdomen instead of your back. Try to lie on your abdomen instead of facing up to increase your abdominal pressure.
- This pressure increase will in turn transmit a signal to your spinal canal and raise spinal pressure.
- Many people find pain relief in this position.
-
8Wear an abdominal binder to increase abdominal pressure. Wearing a tight abdominal binder will raise your abdominal pressure, transmitting signals to your spinal cord that reduce headache.
- You can find abdominal binders in many specialty medical stores.
-
9Try anti-emetics if you suffer from nausea or vomiting. If you suffer from severe spinal headache, nausea or vomiting may accompany it due to irritation of the brain areas that control appetite and vomiting.
- Take anti-emetics like promethazine, prochlorperazine or metoclopramide to control these feelings.
- These drugs act by blocking the sites in the brain where certain chemicals (such as dopamine, histamine etc) responsible for vomiting act.
- Take tab promethazine at a dosage of 25 mg, 2-3 times daily.
- Take these drugs before you have a meal for optimum results.
- Discontinue the medication as soon as you feel better.
Getting Professional Medical Treatment
-
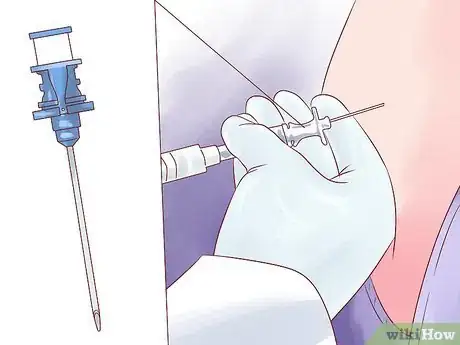
1Get an epidural blood patch for severe chronic headache. If your headache does not resolve within 24 hours, despite taking steps mentioned above, get an epidural blood patch.[6]
- During an epidural blood patch procedure, a small amount of your own blood will be injected in the space just outside the perforation in your spine.
- The blood will clot, sealing the perforation and restoring pressure in the spinal membrane.[7]
- This restores spinal pressure and stops further leakage, relieving headache symptoms.
- The success rate of this technique is more than 70%.
- Usually, 15-30 ml of your blood will be taken from your arm, and then you will lie on your side for 2 hours.
- This procedure can be repeated up to 2 times if the primary attempt fails to control headache.
- An epidural blood patch should not be done if you have a fever or skin infection.
-
2Try an epidural saline solution. A saline solution such can be injected into the epidural space instead of blood.[8]
- It produces a similar effect as blood, but is sterile and comes with a much lower risk of infection.
- However, saline solution is thin and rapidly absorbed by the epidural space, meaning that the pressure is not as effectively maintained as with a blood epidural.
- 1–1.5 liters (0.4 US gal) of Hartmann saline solution can be administered over a 24 hour period, starting the same day of the spinal tap or anesthesia.
-
3Get surgery as a last resort. Surgery is the last treatment option for spinal headache.[9]
- When all other measures fail to stop a spinal leak, surgery can be attempted to repair the perforation.
- It immediately stops the CSF leak, but carries the risk of infection and is somewhat invasive.
- Therefore, your doctor will counsel you thoroughly (regarding the procedure, and its pros and cons) before undergoing surgery.
-
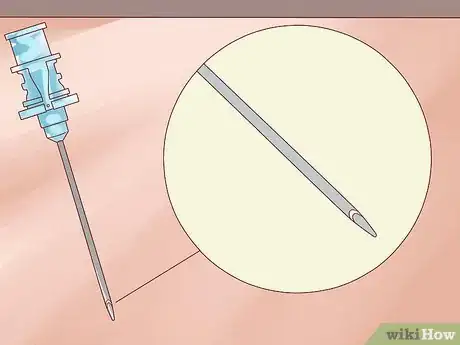
4Make sure an appropriate needle is used during your spinal tap or anesthesia procedure. By using a small needle, the risk of spinal fluid leak is dramatically reduced, because the likelihood of a leak is related to the size of the needle perforation.
- Using an appropriately needle size and shape can minimize the likelihood of spinal headache.
- A large needle bore will produce a large perforation, so it is always best to use small bore needles, usually between 24-27 gauge.
- Use a pencil point needle instead of a cutting type to minimize the chance of leakage.
- If possible, use a new type of needle, known as an Atraucan needle that has a narrow cutting tip and a bevel that greatly reduces the chance of spinal headache.
-
5Make sure the needle is oriented properly. Orientation of the needle is also important. If the beveled edge of the needle is kept horizontal when it is introduced, there a greater chance of tissue damage.
- The beveled edge should always be kept vertical and parallel to the fibers.
Expert Q&A
-
QuestionHow do you get rid of a spinal headache?
 Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Board Certified Neurologist The first step is to be evaluated by your doctor to determine if there is a spinal headache, and where the location may be. This often requires an MRI of the brain and spine. Conservative treatments include rest, hydration with water, caffeine, and lying flat on your back as much as possible for a day or two. Many times the spinal headache will resolve spontaneously.
The first step is to be evaluated by your doctor to determine if there is a spinal headache, and where the location may be. This often requires an MRI of the brain and spine. Conservative treatments include rest, hydration with water, caffeine, and lying flat on your back as much as possible for a day or two. Many times the spinal headache will resolve spontaneously. -
QuestionWhat causes a spinal headache?
 Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Eric Baron, DODr. Eric P. Baron is a staff ABPN (American Board of Psychiatry and Neurology) board certified Neurologist and a UCNS (United Council for Neurologic Subspecialties) Diplomat board certified in Headache Medicine at Cleveland Clinic Neurological Institute, Center for Neurological Restoration – Headache and Chronic Pain Medicine, in Cleveland, Ohio. With over 15 years of experience practicing medicine, he specializes in helping patients with headaches, migraines, and facial pain. Dr. Baron holds a BS in Biology from the University of Toledo and a DO from The Ohio University Heritage College of Osteopathic Medicine. Following his medical education, he completed his neurology residency and fellowship in headache medicine at Cleveland Clinic. Dr. Baron has authored publications in journals such as The Journal of Headache and Pain and was named one of “America’s Top Physicians."
Board Certified Neurologist A spinal headache occurs when there is a small leak in the thick membrane that surrounds the brain and spine, and keeps them cushioned in cerebrospinal fluid.
A spinal headache occurs when there is a small leak in the thick membrane that surrounds the brain and spine, and keeps them cushioned in cerebrospinal fluid.
References
- ↑ Eric Baron, DO. Board Certified Neurologist. Expert Interview. 13 September 2021.
- ↑ Eric Baron, DO. Board Certified Neurologist. Expert Interview. 13 September 2021.
- ↑ https://my.clevelandclinic.org/health/diseases/17927-spinal-headaches
- ↑ https://my.clevelandclinic.org/health/diseases/17927-spinal-headaches
- ↑ https://my.clevelandclinic.org/health/diseases/17927-spinal-headaches
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK482336/
- ↑ Eric Baron, DO. Board Certified Neurologist. Expert Interview. 13 September 2021.
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4261270/
- ↑ https://my.clevelandclinic.org/health/diseases/17927-spinal-headaches
- Basurto Ona X, et al. Drug therapy for treating post-dural puncture headache (Review). The Cochrane Collaboration. 2011;8:1.
- Boonmak P, et al. Epidural blood patching for preventing and treating post-dural puncture headache (Review). The Cochrane Collaboration. 2010;1:1.
- Grant R, Condon B, Hart I, et al. Changes in intracranial CSF volume after lumbar puncture and their relationship to post-LP headache. J Neurol Neurosurg Psychiatry 1991;54:440 –2.
- Kuntz KM, Kokmen E, Stevens JC, et al. Post‐lumbar puncture headaches: experience in 501 consecutive procedures. Neurology 1992;42:1884–7.
- Lavi R, et al. Lumbar puncture: It is time to change the needle. European Neurology. 2010;64:108.
- Silberstein, SD, Marcelis, J. Headache associated with changes in intracranial pressure. Headache 1992; 32:84.
- Vercauteren MP, Hoffman VH, Mertens E, Sermeus L, Adriaensen HA. Seven-year review of requests for epidural blood patches for headache after dural puncture: referral patterns and the effectiveness of blood patches. Eur J Anaesthesiol 1999;16: 298–303.
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2660496/
- http://bja.oxfordjournals.org/content/91/5/718.full
- http://www.medscape.com/viewarticle/578254_8
- http://www.mayoclinic.org/diseases-conditions/spinal-headaches/basics/definition/con-20025295








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...