This article was medically reviewed by Theodore Leng, MD. Dr. Leng is a board certified Ophthalmologist and Vitreoretinal Surgeon and an Assistant Professor of Ophthalmology at Stanford University. He completed his MD and Vitreoretinal Surgical Fellowship at Stanford University in 2010. Dr. Leng is a Fellow of the American Academy of Ophthalmology and the American College of Surgeons. He is also a member of the Association for Research in Vision and Ophthalmology, the Retina Society, the Macula Society, the Vit-Buckle Society, as well as the American Society of Retina Specialists. He received the Honor Award by the American Society of Retina Specialists in 2019.
There are 13 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 89% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 53,202 times.
Cataracts can be difficult to detect. While the clouding of the lens of eye may be obvious to many people, it may not be noticeable to others until it's very far along. Cataracts can make it extremely difficult to see, so it's important to detect them early if possible. In order to detect cataracts, it's best to notice common symptoms, get a cataract test at your doctor's office, and know the likelihood of getting cataracts. Detecting cataracts is the first step in treating and recovering from cataracts.
Steps
Noticing Common Symptoms of Cataracts
-
1Determine if you have cloudy vision. Cloudy vision can be a sign of cataracts. Though it can also be a symptom of many other illnesses, cloudy vision can also be a clear sign of cataracts.[1]
- It's easy to confuse cloudy and blurry vision. While blurry vision is a lack of sharpness in your vision, cloudy vision is best described as a haziness or dullness in what you can see.
- Cloudy vision is caused by a lack of transparency in your eye, in particular the lens. It can also be caused by diabetes, optic nerve damage, and macular degeneration.
-
2Pay attention to any issues with halos or glare. Halos are usually an issue during the evening, but can occur other times when things are mostly dark. Glare, on the other hand, happens mostly during the daytime.
- Halos are a small circle that is around a source of light, such as headlights. They happen mostly during the evening or when it is dark outside.
- Glare is light that seems too bright and does not help you see better. It can happen either during the day or night and can cause your eyes to be teary due to the too intense light source.
Advertisement -
3Notice double vision. Double vision can be caused by a variety of conditions. If you are suffering from double vision due to cataracts, your double vision will be due to problems with the lens of your eye.[2]
- Double vision from cataracts can be in one or both eyes. If it's in both eyes, then you have cataracts in both eyes. Try this test: cover one eye at a time and notice if you still see double. If you do, then it could be the cataract. iI the double vision goes away after you cover one eye, you may actually have an ocular alignment problem (strabismus) instead of cataract as the cause of the double vision.
- When your double vision is due to cataracts, it's an issue with your lens rather than your eye muscle or cornea. The main difference between double vision from cataracts or other issues is that light will be a factor in your double vision.
-
4Recognize any frequent changes in your prescription. Your prescription should be relatively stable, though it will likely become stronger with age. If you find your prescription is changing from year to year, it could be a sign of cataracts.
- Proteins from your lens can build up and change your prescription. This may be a sign of fluctuating blood sugar as well.[3]
- Cataracts could cause changes in prescription based on your vision quality. If your vision is changing regularly alongside other symptoms, you should schedule an appointment with your optometrist.
Getting Cataracts Tests at Your Doctor's Office
-
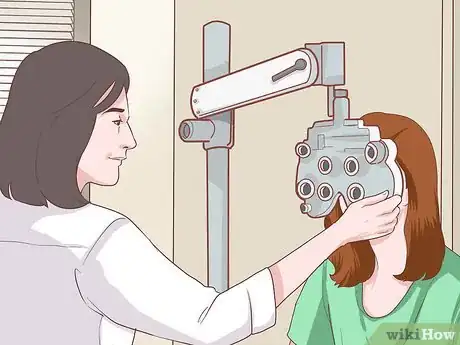
1Visit your optometrist to be screened. Your optometrist may give you a variety of tests as well as questions to determine if you may have cataracts. While some tests will be routine, other are more specific to detect cataracts.
- Your optometrist will ask you questions about your vision such as what symptoms you're having and how long you've experienced them.
- They will also perform a standard eye exam by using the eye chart and the viewing device to determine if you need corrective lenses.
-
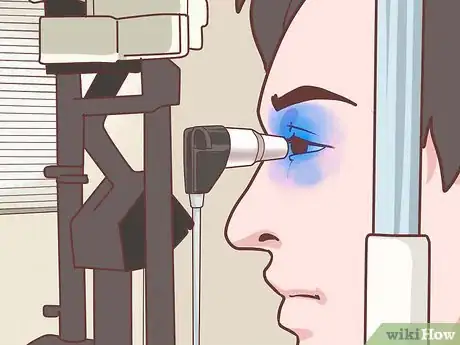
2Use light and magnification to examine your eye. The test is called the slit-lamp examination. It lets your optometrist see the front of your eye under magnification to check for anything unusual.[4]
- The slit refers to an intense line of light that your optometrist uses. Along with magnification, this helps your optometrist examine each section of the cornea, iris, and lens.
- If cataracts are visible at this test, your optometrist may perform additional tests or diagnose you at this time. In either case, they will need to know the severity of the cataracts for a full plan of treatment.
-
3Perform a pupil dilation test. This test dilates your pupils and makes it easier for your optometrist to examine the retina at the back of your eye. If you get this test, get a ride home, since it may be unsafe for you to drive.[5]
- When you're given a pupil dilation test, special drops are placed in your eye to dilate the pupil. The doctor may use either an ophthalmoscope or slit lamp for this examination.
- Since the pupils are artificially dilated, your doctor will probably recommend sunglasses for your trip home to avoid excessive UV exposure to the eye.
-
4Get a tonometry test. The tonometry test is also known as the pressure test. It lets your optometrist know if you have elevated pressure in your eyes, which can be dangerous and a sign of severe cataracts.[6]
- Tonometry tests can be electronic, contact, or non-contact. The most familiar tonometry test is the eye puff test, in which a small puff of air flattens your cornea to check for increased eye pressure.[7]
- The tonometry test also tests for glaucoma. Since many of the symptoms of cataracts can also be symptoms of glaucoma, it's a good idea to make sure this is not your problem instead of cataracts.
-
5Schedule an appointment with an ophthalmologist. If your optometrist thinks you may have cataracts, they may refer you to an ophthalmologist. An ophthalmologist will make the final diagnosis and determine a treatment plan.[8]
- Your ophthalmologist may suggest corrective lenses if your cataracts are not severe; however, in many cases, cataracts are serious enough to require surgery.
- Surgery for cataracts is generally a routine, outpatient procedure. In this surgery, your ophthalmologist removes the cloudy lens and replaces it with an artificial lens.
- After the surgery, you'll want to have someone drive you home. Your vision may be blurry for a while after the surgery; however, if it's still blurry after a few hours or if you experience any pain, contact your ophthalmologist immediately.[9]
Knowing the Likelihood of Getting Cataracts
-
1Know your risk factors for getting cataracts. There are a few big risks for getting cataracts that depend upon your lifestyle, age, and diet. Additionally, previous eye injury can make you more likely to get cataracts.[10]
- While some risk factors for cataracts can be prevented, others are inevitable with age. If you're at an advanced age, you'll want to get checked for cataracts on a regular basis.
- Some risk factors for cataracts can be prevented. A change in diet, management of diabetes or blood pressure, or ceasing drinking or smoking can minimize your risks for diabetes.
-
2Realize that advanced age may cause cataracts. At age 75, nearly 70% of all people have cataracts. With age, your eyes become less flexible and more prone to the accumulation of protein that causes cataracts.[11]
- Our eyes' lenses become thicker with age, making them less transparent and less flexible. This can lead to cataracts due to protein build up.
- Cataracts are pretty common in older people. If you're over 40, it's important to get checked for cataracts on a regular basis.
-
3Limit overexposure to sunlight. Sunlight exposure can also damage your eyes and cause cataracts later in life. Stay out of direct sunlight without UV protected sunglasses to protect your eyes.[12]
- Since one of the major causes of cataracts is cumulative exposure to sunlight, a simple precaution is to wear sunglasses that block UV rays. Wearing a hat with a brim can decrease exposure by 30 – 50 percent.
- High altitude can also contribute to cataracts due to overexposure to sunlight. If you live at a high altitude, it's especially important to keep your eyes protected from the sun.
-
4Know that diabetes, obesity, or high blood pressure can cause cataracts. Since all three issues deal with protein creation, excessive proteins in the eye can create cataracts later in life. If possible, manage any of these issues to minimize cataract development.[13]
- Diabetes can cause a number of eye-related illnesses. High blood sugar creates the conditions for cataract development.[14]
- Obesity or high blood pressure can also cause cataracts. Losing weight and taking blood pressure medicine can potentially reduce the risk of cataracts later in life.
-
5Avoid smoking or drinking too much alcohol. Both activities dramatically increase your likelihood of developing cataracts. While an occasional drink will not severely increase your chances, excessive drinking or smoking can cause major problems.
- Smoking cigarettes can double your chances of developing cataracts. Additionally, the longer you smoke, the worse your risks are for cataracts. [15]
- More than two drinks per day can potentially increase your risks for cataracts. However, moderate drinking can actually reduce your chances.
References
- ↑ https://www.healthgrades.com/symptoms/cloudy-vision
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/003029.htm
- ↑ https://www.ncascade.com/what-causes-your-vision-to-fluctuate/
- ↑ http://www.mayoclinic.org/diseases-conditions/cataracts/basics/tests-diagnosis/con-20015113
- ↑ http://www.mayoclinic.org/diseases-conditions/cataracts/basics/tests-diagnosis/con-20015113
- ↑ http://www.medicinenet.com/tonometry/article.htm
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/003447.htm
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/26829569
- ↑ http://www.allaboutvision.com/conditions/cataract-surgery-recovery.htm
- ↑ http://www.aao.org/eye-health/diseases/cataracts-risk
- ↑ http://www.aao.org/eye-health/diseases/cataracts-risk
- ↑ https://nei.nih.gov/news/briefs/uv_cataract
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2698026/
- ↑ https://nei.nih.gov/health/cataract/cataract_facts
- ↑ http://www.allaboutvision.com/smoking/








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...