This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 22 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 46,118 times.
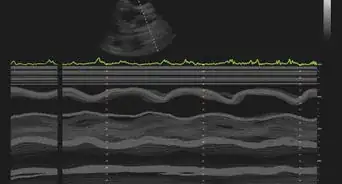
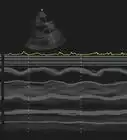
Angina is chest pain or discomfort that happens because your heart isn't getting enough oxygen—usually due to some kind of physical exertion or stress. While you should always talk to your doctor about chest pains, our guide will go over some of the symptoms you might experience and how to tell if it's a medical emergency.
Steps
Recognizing the Signs of Angina
-
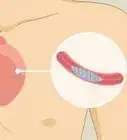
1Note a pain localized behind your breastbone. The main symptom of angina is chest pain or discomfort, which is usually localized just behind the breastbone, or sternum. Typical descriptions of the type of pain include pressure, squeezing, tightness, and heaviness.[1]
- This pain may also result in a difficulty of breathing. Chest heaviness is often described as an elephant sitting on the chest.
- Some also compare the pain to that of indigestion.[2]
-
2Notice whether or not the pain radiates to other parts of your body. The pain may radiate from your chest to your arms, shoulders, jaw, or neck. It may also occur as primary pain in other areas such as your shoulders, arms, neck, jaw, or back.[3]
- Women are statistically more likely than men to experience primary angina pain localized to an area other than the chest, or the chest pain may feel more like stabbing than pressure or tightness.
Advertisement -
3Recognize any accompanying symptoms. Angina pain is caused by myocardial ischemia, which means reduced blood flow to your heart stops it from receiving enough oxygen. Because of this, you are likely to experience a range of symptoms in addition to the actual angina pain. Generally speaking, women are more likely to experience these additional symptoms, sometimes without even feeling typical chest pain. These symptoms include:[4]
- Fatigue
- Nausea
- Dizziness/fainting
- Sweating
- Shortness of breath
- Tightness in your chest
-
4Time the duration of the pain. You should immediately rest and stop putting any undue stress on your heart when you begin feeling a chest pain that you believe to be angina. Once you sit down and rest or take nitroglycerin, the pain should subside in a short amount of time—around five minutes—if you have what is called “stable angina,” which is the most common form.[5]
Warning: Unstable angina is another possibility where the pain is more severe and can last up to 30 minutes. It is no longer relieved by rest or medications. Unstable angina is considered a medical emergency and requires immediate professional evaluation to ensure that you’re not having a heart attack.
-
5Look for patterns in the cause of the pain. Stable angina is deemed as such because the causes and severity are usually both consistent and predictable—at times when you force your heart to work harder. This means that the pain can flare up consistently after exercise, climbing stairs, cold temperature, smoking, and when you’re feeling especially stressed or emotional.[6]
- If you’re accustomed to monitoring symptoms of stable angina and your pain, the cause, the duration, or anything else deviates significantly from the norm, then you should seek immediate medical assistance because your angina has become unstable and could be a sign of a heart attack.
- Prinzmetal angina (or variant angina) is another form, but it’s related to heart spasms that interfere with blood flow. This form of angina can be alarming because it also deviates from a predictable schedule and is very painful. However, medications are available to help control the heart spasms at the root of it. These angina symptoms are often severe and occur at rest often between midnight and early morning and can be mistaken for unstable angina. Causes of Prinzmetal angina include cold weather, stress, medication, smoking and cocaine use. Consult your doctor immediately for a proper diagnosis.
Knowing When to Seek Emergency Care
-
1Call 911 if you’ve never experienced angina before. If you’ve never experience angina pain before and you’ve never been diagnosed with any heart condition, then you should call 911 at the first onset. Your symptoms could indicate a heart attack, so you should not wait to see if the symptoms subside on their own. If the symptoms indicate the onset of CAD, then your doctor will discuss treatment options and what to do for future instances of angina.
-
2Call 911 if your episode deviates from your stable angina history. If you’ve been diagnosed with CAD and know the usual triggers of your angina pain, then you should seek immediate medical care if your symptoms deviate from their usual pattern.[7] This can be a sign of a heart attack. Your symptoms differ in several ways, including:[8]
- Increased severity
- Symptoms lasting longer than 20 minutes
- Occurring at rest
- Occurring with less activity than usual
- New symptoms in association such as nausea, shortness of breath, a cold sweat, or a sense of impending doom
- Symptoms are not relieved by taking medication, such as nitroglycerin
-
3Call 911 if your stable angina doesn’t respond to medication. Nitroglycerin is often prescribed to those with CAD because it dilates the arteries, helping to restore proper blood flow. You should call 911 if your pains don’t subside with rest or if they don’t respond to your nitroglycerin.[9]
- Directions for nitroglycerin tablets and sprays usually suggest resting while taking a dose every five minutes (up to three doses) while symptoms continue. Use as directed and contact your care provider if the symptoms do not respond.
Identifying Risk Factors
-
1Recognize your age as a risk. The risk for angina increases with age. Specifically, the risk for angina increases for men older than 45 years and women older than 55 years.[10] In general, the development of angina in women lags approximately ten years behind men. A decline in the natural hormone estrogen may be a factor in the increased risk for angina and heart disease among postmenopausal women.[11]
-
2Consider your sex. Angina is more often the presenting symptom of coronary artery disease (CAD) in women than in men.[12] Low estrogen levels in women after menopause may play a role in the development of coronary microvascular disease (MVD), and thus microvascular angina.[13] Up to 50 percent of women with angina have coronary MVD.[14] The leading killer of both men and women is CAD.[15]
- Estrogen protects women from heart disease. After menopause, estrogen levels drop drastically and translate into higher risks for angina in women. Women who have gone through early menopause, either naturally or as a result of hysterectomy (removal of the uterus), are twice as likely to develop angina as women of the same age who have not yet entered menopause.[16]
-
3Look at your family history. A family history of early heart disease increases an individual’s risk for angina and heart disease. If you have a father or brother who was diagnosed earlier than age 55—or if your mother or sister was diagnosed before age 65—then your risk is highest.
- Having one first-degree relative diagnosed with early heart disease may increase your risk for angina and heart disease by as much as 33 percent. That risk can jump to as high as 50 percent if you have two or more first-degree relatives diagnosed.[17]
-
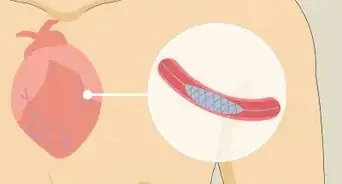
4Examine your smoking habits. Smoking increases the risk for angina and heart disease through several mechanisms. Smoking accelerates the development of atherosclerosis (buildup of fatty deposits and cholesterol in your arteries) by as much as 50 percent. Carbon monoxide in smoke also displaces oxygen in the blood, leading to a deficiency of oxygen in the cells of heart muscle (cardiac ischemia). Cardiac ischemia can lead to angina and heart attack. Smoking also decreases exercise tolerance, which can shorten exercise times associated with the development of angina.[18]
-
5Take into account if you’re diabetic. Diabetes is a modifiable risk factor for heart disease and thus angina. Diabetics have blood with a higher viscosity (thickness) than usual.[19] This makes the heart work harder to pump blood. Diabetics also have thicker atrial walls in their hearts, allowing the passageways to block more easily.
-
6Test your blood pressure. Consistently high blood pressure (hypertension) can cause hardening and thickening in your arteries. Persistently, or chronically, elevated blood pressure leads to damage of the walls of your arteries, which predisposes you to atherosclerosis (arterial buildup).[20]
- If you are younger than 60 years of age, hypertension is defined as a blood pressure of 140/90 mm Hg or higher on more than one occasion. If you are older than 60 years of age, hypertension is defined as a blood pressure of 150/90 mm Hg or higher on more than one occasion.
-
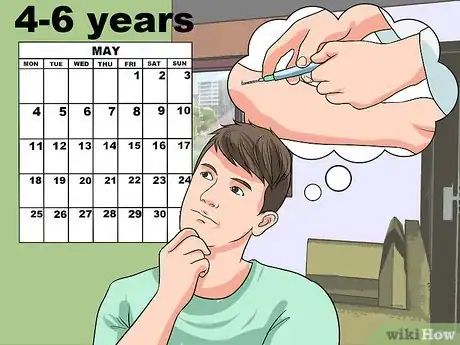
7Try to reduce your cholesterol. High cholesterol (hypercholesterolemia) also contributes to buildup on the atrial walls of your heart (atherosclerosis). The American Heart Association (AHA) recommends that all adults age 20 or older have a complete lipoprotein profile checked every four to six years to assess their risk for angina and heart disease.[21]
- A complete lipoprotein profile is a blood test that measures total blood cholesterol, high density lipoprotein (HDL) cholesterol (also known as “good” cholesterol), LDL cholesterol, and triglycerides.[22]
- Both high levels of LDL (so-called “bad” cholesterol) and low levels of HDL (“good” cholesterol) can also result in atherosclerosis.
-
8Consider your weight. Obesity (a BMI of 30 or higher[23] ) increases other risk factors since obesity is tied to high blood pressure, high cholesterol, and developing diabetes. In fact, this collection of associated symptoms is referred to a metabolic syndrome and includes:[24]
- Hyperinsulinemia (fasting blood glucose level >100 mg/dL)
- Abdominal obesity (waist circumference >40 in for men or >35 in for women)
- Decreased HDL cholesterol levels (<40 mg/dL for men or <50 mg/dL for women)
- Hypertriglyceridemia (triglycerides >150 mg/dL)
- Hypertension
-
9Find out if you have high levels of certain substances in your blood. Your doctor may check your blood to find out if you have high blood levels of homocysteine, C-Reactive protein (CRP), ferritin (or stored iron levels), interleukin-6 and lipoprotein (a).[25] [26] [27] [28] These substances can all increase your risk of CAD and angina if you are outside of the normal ranges. You can also request these tests from your doctor, and then talk to your doctor about what you can do to lower your risk if any of your levels are abnormal.
-
10Evaluate your stress levels. Stress makes your heart work harder by making it beat faster and more heavily. People who suffer from chronic stress are much more likely to develop heart conditions.[29]
Warnings
- Exposure to cold weather will narrow the opening of the blood vessels in the body, including the heart arteries. This, too, can be a cause.⧼thumbs_response⧽
- While this article offers information related to angina, you should not consider it medical advice. Contact your doctor immediately for any symptoms related to angina.⧼thumbs_response⧽
- If you're experiencing chest pain, see your doctor immediately.⧼thumbs_response⧽
References
- ↑ https://my.clevelandclinic.org/health/diseases/21489-angina
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/angina
- ↑ https://www.nhs.uk/conditions/angina/symptoms/
- ↑ https://my.clevelandclinic.org/health/diseases/21489-angina
- ↑ https://www.nhs.uk/conditions/angina/symptoms/
- ↑ https://pubmed.ncbi.nlm.nih.gov/28120185/
- ↑ http://www.emedicinehealth.com/angina_pectoris/page4_em.htm#when_to_seek_medical_care
- ↑ http://www.emedicinehealth.com/angina_pectoris/page4_em.htm#when_to_seek_medical_care
- ↑ http://www.emedicinehealth.com/angina_pectoris/page4_em.htm#when_to_seek_medical_care
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/angina
- ↑ http://www.heart.org/HEARTORG/Conditions/More/MyHeartandStrokeNews/Menopause-and-Heart-Disease_UCM_448432_Article.jsp
- ↑ http://emedicine.medscape.com/article/150215-overview
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/cmd
- ↑ http://www.heart.org/HEARTORG/Conditions/More/MyHeartandStrokeNews/Menopause-and-Heart-Disease_UCM_448432_Article.jsp
- ↑ http://emedicine.medscape.com/article/150215-overview
- ↑ http://www.nhlbi.nih.gov/health/educational/hearttruth/lower-risk/risk-factors.htm
- ↑ http://www.nhlbi.nih.gov/health-pro/guidelines/current/cardiovascular-health-pediatric-guidelines/full-report-chapter-4
- ↑ http://circ.ahajournals.org/content/48/6/1169.full.pdf
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC333092/
- ↑ https://pubmed.ncbi.nlm.nih.gov/30197243/
- ↑ https://pubmed.ncbi.nlm.nih.gov/7968073/
- ↑ http://www.heart.org/HEARTORG/Conditions/Cholesterol/AboutCholesterol/What-Your-Cholesterol-Levels-Mean_UCM_305562_Article.jsp
- ↑ http://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm
- ↑ https://pubmed.ncbi.nlm.nih.gov/28587579/?from_term=metabolic+syndrome+symptoms&from_pos=1
- ↑ https://www.scielo.br/j/abc/a/vKC7qSkvMMwhJJ6FBwFxJZC/?lang=en
- ↑ https://handls.nih.gov/pubs/2012-Olesnevich-PublicHealthNutr-1291-1298-1.pdf
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/25635749
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/8651092
- ↑ https://pubmed.ncbi.nlm.nih.gov/25727240/
About This Article
Angina pains feel like chest pains or discomfort that sometimes radiates down the arm, and these pains are dangerous because they're similar to heart attack symptoms. If you've never experienced angina before, call emergency services immediately because you may be suffering from cardiac arrest. In addition to generalized pain, angina pain often feels like a squeezing, heaviness, or pressure behind your breastbone. You might also experience pain that radiates to other parts of your body, like your arms, shoulders, jaw, or neck. Other symptoms to watch for include fatigue, nausea, dizziness, sweating, or shortness of breath. If you have any of these symptoms, immediately stop and rest or take nitroglycerin, which should help the pain subside. For more tips from our Medical co-author, including how to assess your risk factors for angina, keep reading!





































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...