This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 19,647 times.
Heel pain can be due to a variety of causes, from overuse, sprain, and jumping on a hard surface to plantar fasciitis. See your doctor if you’ve suffered an injury, have severe pain, and can’t bear weight on your foot. For minor pain, try to rest as much as possible, ice the area, and take over the counter pain medication. Foot and calf stretches could help, but you should talk to your doctor before stretching, especially if you’ve suffered an injury. You should also swap flimsy footwear, such as flip-flops, for sturdy, supportive shoes. If pain doesn’t go away after 2 to 3 weeks of home care, schedule an appointment with your doctor or a podiatrist.
Steps
Providing Home Care
-
1See a doctor if you suffered an injury and can’t put weight on your foot. Minor pain can often goes away after 1 to 2 weeks of home care. However, you should see a doctor promptly if sudden, severe pain prevents you from bearing weight on your heel. Injuries such as a moderate to severe sprain or stress fracture require medical attention.[1]
- If your pain is minor, provide home care for 2 to 3 weeks, then see your doctor if your heel doesn’t get better.
-
2Rest your foot as much as possible. Avoid running, jumping, lifting heavy objects, and other demanding activities. Try to stay off of your feet as much as possible for at least a week.[2]
- If necessary, use crutches or a cane to keep weight off the affected foot.
Advertisement -
3Apply ice for 15 minutes up to 4 times daily. Icing the area can help reduce inflammation and temporarily remove pain. Don’t apply ice directly to your skin. Instead, wrap an ice pack or ice in a cloth, then hold it to your skin for 15 minutes.[3]
- You can also place your heel in an ice foot bath. Fill a tub with ice water, then place your heel into the water for a few minutes at a time. The water's temperature should not go below 55 °F (13 °C). Continue to dip your foot for up to 15 minutes.
-
4Wrap your foot with sports tape. Taping your foot can help stabilize its tendons, muscles, and joints. Anchor the end of a strip of sports tape just under your big toe, wrap the strip under your foot, bring it around your heel, then cross it under your foot again to the underside of your pinky toe.[4]
- You should have made an X on the bottom of your foot, with the center of the X aligned with the center of your foot.
- Repeat crossing the tape in X shapes 3 times, then wrap the tape around your foot horizontally until you’ve covered your entire foot from the ball to the heel.
- Make sure your wrap is not too loose nor too tight.
-
5Take an over the counter pain reliever. Aspirin or ibuprofen can help reduce inflammation and manage pain. Take any medication according to the label’s instructions.[5]
- You can also take acetaminophen as long as you don’t drink alcohol while you take it. In combination, acetaminophen and alcohol can cause liver damage.
Trying Stretches
-
1Call your doctor before stretching, especially if you’re injured. It’s best to consult a doctor before stretching when you’re in pain or if you’ve recently suffered an injury. If they approve, stretch the area for up to 3 minutes total 2 to 3 times per day.
- Stop stretching immediately if you feel sharp pain.[6]
- Stretches and yoga poses can help manage plantar fasciitis, which is one of the most common causes of heel pain.
-
2Gently massage your heels and feet. Apply an oil or lotion to your foot and then massage it into your feet. Use your thumbs to apply pressure to sore points. Pay special attention to your arch and areas that are giving you trouble.
- If you tilt the ball of your foot forward, you can more easily rub your plantar fascia.[7]
- Avoid applying pressure that causes you pain.
-
3Loosen your foot using a wooden or foam roller. Wooden or foam rollers can help work out tightness in your foot or deepen a massage. You can manually rub the roller against your foot, or you can place it on the ground and rub your foot over it.[8]
- Wooden rollers are often made small just for feet. You can even find some that rest on the floor so that you can easily rub your foot against them.
- Foam rollers can also be laid on the floor under your foot so that you can rub your foot over it.
-
4Stretch your plantar fascia with a towel or strap. Sit up straight with your legs outstretched. Loop a long towel or strap around your foot. While keeping your knee straight, gently pull your toes toward your torso.[9]
- Hold the stretch for 20 seconds, switch feet, and do a total of 5 reps per foot.[10]
-
5Cross your legs and stretch your plantar fascia with your hands. Sit in a chair with your feet flat on the floor and your knees bent at 90 degree angles. Cross your legs by bringing your right foot to the opposite knee. Rest the foot on your knee so your toes point forward.[11]
- Use your right hand to gently pull your right toes toward your right shin. As you stretch, use your left thumb to gently rub the your right foot’s plantar fascia, which feels firm and taut, like a guitar string.
- Hold the stretch for 20 seconds, switch legs, and to a total of 5 reps for each foot.
-
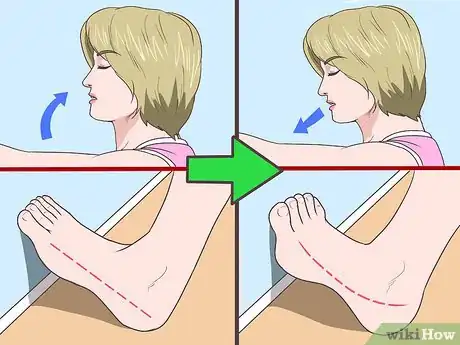
6Do calf stretches. While standing, lean toward a wall and place your palms against it with your elbows outstretched (but not locked). Extend your left leg behind you so it’s straight with your heel flat on the floor. Your right knee should be slightly bent.[12]
- You should feel a stretch in your left calf and heel chord. Hold the stretch for 20 seconds, switch legs, and do 5 reps total per leg.
-
7Hold a stretch steadily and remember to breathe. Don't bounce in and out of a stretch, and don’t push your body past your normal range of motion. Breathe in as you move into a stretch, then exhale as you stretch. Never hold your breath as you stretch.[13]
Wearing Supportive Footwear
-
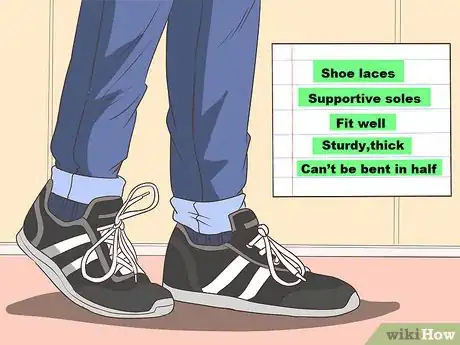
1Choose shoes with laces and supportive soles. Your shoes should fit well, and you should be able to tie them securely so they fit snugly around your feet. To check if a shoe is supportive, hold it by the toe and heel and try to gently bend it in half. If you can easily bend the sole in half, it won’t provide enough support for your feet.[14]
- Go for shoes with soles that are sturdy, thick, and can’t be bent in half.
-
2Avoid wearing flip-flops and other flimsy footwear. Footwear that doesn’t support your feet can cause or worsen pain. If possible, only wear supportive shoes, especially when you experience heel pain. Additionally, avoid walking around barefoot.[15]
-
3Try using heel pads or shoe inserts. Look for heel pads or orthotic inserts at your local drugstore. They cushion your feet, provide support, and preserve your arches as you walk.[16]
- You could also ask your doctor or podiatrist for custom inserts, but there’s no evidence that they’re more effective than store-bought options.[17]
-
4Don’t wear worn-out athletic shoes. Replace old and worn out shoes as they have lost comfort and arch support. Runners should buy a new pair of shoes after using it for 500 miles. Shoes should be checked for cushioning and adequacy of arch support well before use.
- Always prefer shoes with greater support and optimal inner lining to absorb the shock and stress. It is not suggested to walk barefoot on hard or rigid surfaces.
Consulting a Medical Professional
-
1See your doctor or a podiatrist if pain persists or worsens. If your pain doesn’t go away after 2 to 3 weeks of home care, your best option is to seek medical treatment. If you don’t have a podiatrist, or a foot specialist, ask your primary doctor for a referral.[18]
- Your doctor or specialist will perform a physical exam and ask about your physical activity, when the pain started, and if it’s worse at certain times of the day.
- Depending on your physical exam and severity of your symptoms, they might recommend an x-ray.
-
2Have your doctor or specialist examine your posture and gait. The way you stand or walk can cause or aggravate heel pain. If necessary, your doctor will recommend ways to correct imbalances or gait abnormalities.[19]
-
3Ask if they recommend night splints. Night splints keep your ankle in a neutral position while you sleep. This gently stretches your plantar fascia and calf muscle, and prevents your ankle from rolling into a position that might aggravate your pain.[20]
- If your podiatrist recommends, wear a night splint overnight for at least 1 to 3 months. Continuing use even after your pain goes away can help prevent symptoms from returning.
-
4Ask about ultrasound therapy. If other treatment methods aren’t effective, your doctor might recommend ultrasound therapy. In this procedure, sound waves are projected into the affected area. It could relieve inflammation and stimulate blood flow.[21]
- Ultrasound therapy is non-invasive, so it’s usually recommended before injections or surgery.
-
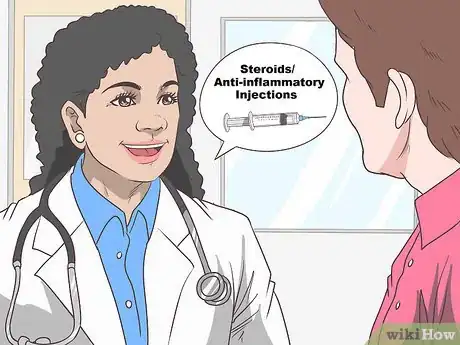
5Discuss steroid or anti-inflammatory injections. Your doctor or specialist will first recommend conservative treatment, such as stretching, taping, or night splints. If your symptoms are severe or conservative treatment doesn’t work, they might inject a corticosteroid or other anti-inflammatory medication into the heel.[22]
- They’ll numb the area first, so the injection won't hurt.
-
6Discuss surgical treatments with your podiatrist, if necessary. If your symptoms persist for more than 6 to 12 months and no other treatments are effective, surgery might be the best option. While cases are rare, surgery is sometimes necessary to correct plantar fasciitis, remove a heel spur, or relieve compressed nerves.[23]
- People who have surgery for heel pain can usually go home on the day of surgery. You might have to wear a boot or splint, and your doctor will likely advise you to avoid bearing weight on the affected foot for 2 to 3 weeks.
References
- ↑ https://medlineplus.gov/ency/article/003181.htm
- ↑ https://medlineplus.gov/ency/article/003181.htm
- ↑ https://www.healthdirect.gov.au/plantar-fasciitis
- ↑ https://www.apma.org/Patients/FootHealth.cfm?ItemNumber=985
- ↑ https://medlineplus.gov/ency/article/003181.htm
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3687890/#!po=31.8182
- ↑ https://www.verywell.com/five-tips-to-fix-your-aching-feet-1337689
- ↑ https://www.verywell.com/five-tips-to-fix-your-aching-feet-1337689
- ↑ https://www.nhs.uk/conditions/heel-pain/treatment/
- ↑ https://www.nhs.uk/conditions/heel-pain/treatment/
- ↑ http://www.aofas.org/footcaremd/conditions/ailments-of-the-heel/Pages/Plantar-Fasciitis.aspx
- ↑ http://www.aofas.org/footcaremd/conditions/ailments-of-the-heel/Pages/Plantar-Fasciitis.aspx
- ↑ https://www.youtube.com/watch?v=73Wpb9TlP4k
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/foot-problems-heel-pain
- ↑ https://www.apma.org/Patients/FootHealth.cfm?ItemNumber=985
- ↑ https://medlineplus.gov/ency/article/003181.htm
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3687890/#!po=31.8182
- ↑ https://medlineplus.gov/ency/article/003181.htm
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/foot-problems-heel-pain
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3687890/#!po=31.8182
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3687890/#!po=31.8182
- ↑ https://www.nhs.uk/conditions/heel-pain/treatment/#corticosteroid-injections
- ↑ https://www.apma.org/Patients/FootHealth.cfm?ItemNumber=985
- ↑ https://www.apma.org/Patients/FootHealth.cfm?ItemNumber=985










































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...