Cerebral contusion
Cerebral contusion, Latin contusio cerebri, a form of traumatic brain injury, is a bruise of the brain tissue.[2] Like bruises in other tissues, cerebral contusion can be associated with multiple microhemorrhages, small blood vessel leaks into brain tissue. Contusion occurs in 20–30% of severe head injuries.[3] A cerebral laceration is a similar injury except that, according to their respective definitions, the pia-arachnoid membranes are torn over the site of injury in laceration and are not torn in contusion.[4][5] The injury can cause a decline in mental function in the long term and in the emergency setting may result in brain herniation, a life-threatening condition in which parts of the brain are squeezed past parts of the skull.[3] Thus treatment aims to prevent dangerous rises in intracranial pressure, the pressure within the skull.
| Cerebral contusion | |
|---|---|
 | |
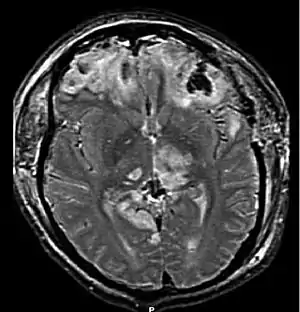
| CT scan showing cerebral contusions, hemorrhage within the hemispheres, subdural hematoma on the left, and skull fractures[1] | |
| Specialty | Emergency medicine |
| Complications | cerebral edema , transtentorial herination |
Contusions are likely to heal on their own without medical intervention.[6]
Signs and symptoms
The symptoms of a cerebral contusion depend on the severity of the injury, ranging from minor to severe. Individuals may experience a headache, confusion, sleepiness, dizziness, loss of consciousness, nausea and vomiting, seizures, difficulty with coordination and movement, lightheadedness, tinnitus, and spinning sensations. They may also have difficulty with memory, vision, speech, hearing, managing emotions, and thinking.[7] Signs also depend on the contusion's location in the brain.[7]
Causes

Often caused by a blow to the head, contusions commonly occur in coup or contre-coup injuries. In coup injuries, the brain is injured directly under the area of impact, while in contrecoup injuries it is injured on the side opposite the impact.
Contusions occur primarily in the cortical tissue, especially under the site of impact or in areas of the brain located near sharp ridges on the inside of the skull. The brain may be contused when it collides with bony protuberances on the inside surface of the skull.[8] The protuberances are located on the inside of the skull under the frontal and temporal lobes and on the roof of the ocular orbit.[9] Thus, the tips of the frontal and temporal lobes located near the bony ridges in the skull are areas where contusions frequently occur and are most severe.[10] For this reason, attention, emotional and memory problems, which are associated with damage to frontal and temporal lobes, are much more common in head trauma survivors than are syndromes associated with damage to other areas of the brain.[11]
Features
Contusions, which are frequently associated with edema, are especially likely to cause increases in intracranial pressure (ICP) and concomitant crushing of delicate brain tissue. They typically form in a wedge-shape with the widest part in the outermost part of the brain.[12] The distinction between contusion and intracerebral hemorrhage is blurry because both involve bleeding within the brain tissue; however, an arbitrary cutoff exists that the injury is a contusion if two thirds or less of the tissue involved is blood and a hemorrhage otherwise.[3]
The contusion may cause swelling of the surrounding brain tissue, which may be irritated by toxins released in the contusion.[3] The swelling is worst at around four to six days after the injury.[3] Extensive contusion associated with subdural hematoma is called burst lobe.[5] Cases of a burst frontal or temporal lobe are associated with high mortality and morbidity.[5]
Old or remote contusions are associated with resorption of the injured tissue, resulting in various degrees of cavitation, in addition to the presence of a golden-yellow discoloration due to residual hemosiderin. These remote contusions are often referred to as plaque jaune or yellow plaque.[13]
Multiple petechial hemorrhages
Numerous small contusions from broken capillaries that occur in grey matter under the cortex are called multiple petechial hemorrhages or multifocal hemorrhagic contusion.[14] Caused by shearing injuries at the time of impact, these contusions occur especially at the junction between grey and white matter and in the upper brain stem, basal ganglia, thalamus and areas near the third ventricle.[14] The hemorrhages can occur as the result of brain herniation, which can cause arteries to tear and bleed.[14] A type of diffuse brain injury, multiple petechial hemorrhages are not always visible using current imaging techniques like CT and MRI scans. This may be the case even if the injury is quite severe, though these may show up days after the injury.[15] Hemorrhages may be larger than in normal contusions if the injury is quite severe. This type of injury has a poor prognosis if the patient is comatose, even with no apparent causes for the coma.[15]
Treatment
Since cerebral swelling presents a danger to the patient, treatment of cerebral contusion aims to prevent swelling. Measures to avoid swelling include prevention of hypotension (low blood pressure), hyponatremia (insufficient sodium), and hypercapnia (increased carbon dioxide in the blood).[3] Due to the danger of increased intracranial pressure, surgery may be necessary to reduce it.[3] People with cerebral contusion may require intensive care and close monitoring.[3]
References
- Rehman T, Ali R, Tawil I, Yonas H (2008). "Rapid progression of traumatic bifrontal contusions to transtentorial herniation: A case report". Cases Journal. 1 (1): 203. doi:10.1186/1757-1626-1-203. PMC 2566562. PMID 18831756.
- Hardman JM, Manoukian A (2002). "Pathology of Head Trauma". Neuroimaging Clinics of North America. 12 (2): 175–187, vii. doi:10.1016/S1052-5149(02)00009-6. PMID 12391630.
- Khoshyomn S, Tranmer BI (May 2004). "Diagnosis and management of pediatric closed head injury". Seminars in Pediatric Surgery. 13 (2): 80–86. doi:10.1053/j.sempedsurg.2004.01.003. PMID 15362277.
- Granacher RP (2007). Traumatic Brain Injury: Methods for Clinical & Forensic Neuropsychiatric Assessment (Second ed.). Boca Raton: CRC. p. 26. ISBN 978-0-8493-8138-6. Retrieved 2008-07-06.
- Gennarelli GA, Graham DI (2005). "Neuropathology". In Silver JM, McAllister TW, Yudofsky SC (eds.). Textbook Of Traumatic Brain Injury. Washington, DC: American Psychiatric Association. p. 29. ISBN 1-58562-105-6. Retrieved 2008-06-10.
- Sanders MJ and McKenna K. 2001. Mosby's Paramedic Textbook, 2nd revised Ed. Chapter 22, "Head and Facial Trauma." Mosby.
- Kushner D (1998). "Mild Traumatic Brain Injury: Toward Understanding Manifestations and Treatment". Archives of Internal Medicine. 158 (15): 1617–1624. doi:10.1001/archinte.158.15.1617. PMID 9701095.
- Rao V, Lyketsos C (2000). "Neuropsychiatric Sequelae of Traumatic Brain Injury". Psychosomatics. 41 (2): 95–103. doi:10.1176/appi.psy.41.2.95. PMID 10749946.
- Shepherd S. 2004. "Head Trauma." Emedicine.com. Retrieved on 2008-01-10.
- Graham DI and Gennareli TA. Chapter 5, "Pathology of Brain Damage After Head Injury" Cooper P and Golfinos G. 2000. Head Injury, 4th Ed. Morgan Hill, New York.
- Bigler, ED. 2000. The Lesion(s) in Traumatic Brain Injury: Implications for Clinical Neuropsychology. Accessed through web archive. Retrieved on 2008-01-17.
- Vinas FC and Pilitsis J. 2006. "Penetrating Head Trauma." Emedicine.com. Retrieved on 2008-01-10.
- "Brain Traumatic Lesions". Archived from the original on 2010-11-09. Retrieved 2009-01-07.
- "Brain Injury, Traumatic". Medcyclopaedia. GE. Archived from the original on 2011-05-26.
- Downie A. 2001. "Tutorial: CT in Head Trauma" Archived 2005-11-06 at the Wayback Machine. Retrieved May 8, 2008