Iron supplement
Iron supplements, also known as iron salts and iron pills, are a number of iron formulations used to treat and prevent iron deficiency including iron deficiency anemia.[1][2] For prevention they are only recommended in those with poor absorption, heavy menstrual periods, pregnancy, hemodialysis, or a diet low in iron.[2][3] Prevention may also be used in low birth weight babies.[2] They are taken by mouth, injection into a vein, or injection into a muscle.[2] While benefits may be seen in days, up to two months may be required until iron levels return to normal.[4]
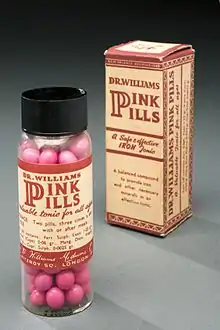 Iron supplement from the late 19th and early 20th century | |
| Clinical data | |
|---|---|
| Trade names | Feosol, Feostat, Feratab, others |
| Other names | Iron pills, iron salts, ferrous salts, ferric salts |
| AHFS/Drugs.com | Monograph |
| Routes of administration | By mouth, by injection |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
| CAS Number | |
| ChemSpider |
|
Common side effects include constipation, abdominal pain, dark stools, and diarrhea.[4] Other side effects, which may occur with excessive use, include iron overload and iron toxicity.[1][3] Ferrous salts used as supplements by mouth include ferrous fumarate, ferrous gluconate, ferrous succinate, and ferrous sulfate.[3] Injectable forms include iron dextran and iron sucrose.[3] They work by providing the iron needed for making red blood cells.[4]
Iron pills have been used medically since at least 1681, with an easy-to-use formulation being created in 1832.[5] Ferrous salt is on the World Health Organization's List of Essential Medicines.[6] Ferrous salts are available as a generic medication and over the counter.[1] Slow release formulations, while available, are not recommended.[2] In 2017, ferrous sulfate was the 92nd most commonly prescribed medication in the United States, with more than eight million prescriptions.[7][8]
Medical uses
Iron supplements are used to treat iron deficiency and iron-deficiency anemia;[9] parenteral irons can also be used to treat functional iron deficiency, where requirements for iron are greater than the body's ability to supply iron such as in inflammatory states. The main criterion is that other causes of anemia have also been investigated, such as vitamin B12 or folate deficiency, drug induced or due to other poisons such as lead, as often the anemia has more than one underlying cause.
Iron deficiency anemia is classically a microcytic, hypochromic anemia. Generally, in the UK oral preparations are trialled before using parenteral delivery,[10] unless there is the requirement for a rapid response, previous intolerance to oral iron or likely failure to respond. Intravenous iron may decrease the need for blood transfusions however it increases the risk of infections when compared to oral iron.[11] A 2015 Cochrane Collaboration review found that daily oral supplementation of iron during pregnancy reduces the risk of maternal anemia and that effects on infant and on other maternal outcomes are not clear.[12] Another review found tentative evidence that intermittent iron supplements by mouth for mothers and babies is similar to daily supplementation with fewer side effects.[13] Supplements by mouth should be taken on an empty stomach, optionally with a small amount of food to reduce discomfort.[14]
Athletes
Athletes may be at elevated risk of iron deficiency and so benefit from supplementation, but the circumstances vary between individuals and dosage should be based on tested ferritin levels, since in some cases supplementation may be harmful.[15]
Frequent blood donors
Frequent blood donors may be advised to take iron supplements. Canadian Blood Services recommends discussing "taking iron supplements with your doctor or pharmacist" as "the amount of iron in most multivitamins may not meet your needs and iron supplements may be necessary".[16] The American Red Cross recommends "taking a multivitamin with 18 mg of iron or an iron supplement with 18-38 mg of elemental iron for 60 days after each blood donation, for 120 days after each power red donation or after frequent platelet donations".[17] A 2014 Cochrane Review found that blood donors were less likely to be deferred for low hemoglobin levels if they were taking oral iron supplements, although 29% of those who took them experienced side effects in contrast to the 17% that took a placebo. It is unknown what the long-term effects of iron supplementation for blood donors may be.[18]
Side effects
Side effects of therapy with oral iron are most often diarrhea or constipation and epigastric abdominal discomfort. Taken after a meal, side effects decrease, but there is an increased risk of interaction with other substances. Side effects are dose-dependent, and the dose may be adjusted.
The patient may notice that their stools become black. This is completely harmless, but patients must be warned about this to avoid unnecessary concern. When iron supplements are given in a liquid form, teeth may reversibly discolor (this can be avoided through the use of a straw). Intramuscular injection can be painful, and brown discoloration may be noticed.
Treatments with iron(II) sulfate have higher incidence of adverse events than iron(III)-hydroxide polymaltose complex (IPC)[19][20][21] or iron bis-glycinate chelate.[22][23]
Iron overdose has been one of the leading causes of death caused by toxicological agents in children younger than 6 years.[24]
Iron poisoning may result in mortality or short-term and long-term morbidity.[25]
Infection risk
Because one of the functions of elevated ferritin (an acute phase reaction protein) in acute infections is thought to be to sequester iron from bacteria, it is generally thought that iron supplementation (which circumvents this mechanism) should be avoided in patients who have active bacterial infections. Replacement of iron stores is seldom such an emergency situation that it cannot wait for any such acute infection to be treated.
Some studies have found that iron supplementation can lead to an increase in infectious disease morbidity in areas where bacterial infections are common. For example, children receiving iron-enriched foods have demonstrated an increased rate in diarrhea overall and enteropathogen shedding. Iron deficiency protects against infection by creating an unfavorable environment for bacterial growth. Nevertheless, while iron deficiency might lessen infections by certain pathogenic diseases, it also leads to a reduction in resistance to other strains of viral or bacterial infections, such as Salmonella typhimurium or Entamoeba histolytica. Overall, it is sometimes difficult to decide whether iron supplementation will be beneficial or harmful to an individual in an environment that is prone to many infectious diseases; however this is a different question than the question of supplementation in individuals who are already ill with a bacterial infection.[26]
Children living in areas prone for malarial infections are also at risk of developing anemia. It was thought that iron supplementation given to such children could increase the risk of malarial infection in them. A Cochrane systematic review published in 2016 found high quality evidence that iron supplementation does not increase the risk of clinical malaria in children.[27]
Contraindications
Contraindications often depend on the substance in question. Documented hypersensitivity to any ingredients and anemias without proper work-up (i.e., documentation of iron deficiency) is true of all preparations. Some can be used in iron deficiency, others require iron deficiency anaemia to be present. Some are also contraindicated in rheumatoid arthritis.[28]
Hemochromatosis
Individuals may be genetically predisposed to excessive iron absorption, as is the case with those with HFE hereditary hemochromatosis. Within the general population, 1 out of 400 people has the homozygous form of this genetic trait, and 1 out of every 10 people has its heterozygous form.[29] Neither individuals with the homozygous or heterozygous form should take iron supplements.[29]
Interactions
Non-heme iron forms an insoluble complex with several other drugs, resulting in decreased absorption of both iron and the other drug. Examples include tetracycline, penicillamine, methyldopa, levodopa, bisphosphonates and quinolones. The same can occur with elements in food, such as calcium, which impacts both heme and non-heme iron absorption.[30] Absorption of iron is better at a low pH (i.e. an acidic environment), and absorption is decreased if there is a simultaneous intake of antacids.
Many other substances decrease the rate of non-heme iron absorption. One example is tannins from foods such as tea[31] and phytic acid.[32] Because iron from plant sources is less easily absorbed than the heme-bound iron of animal sources, vegetarians and vegans should have a somewhat higher total daily iron intake than those who eat meat, fish or poultry.[33][34]
Taken after a meal, there are fewer side effects but there is also less absorption because of interaction and pH alteration. Generally, an interval of 2–3 hours between the iron intake and that of other drugs seems advisable, but is less convenient for patients and can impact on compliance.
History
The first pills were commonly known as Blaud's pills,[35] which were named after P. Blaud of Beaucaire, the French physician who introduced and started the use of these medications as a treatment for patients with anemia.[36]
Administration
By mouth
Iron can be supplemented by mouth using various forms, such as iron(II) sulfate. This is the most common and well studied soluble iron salt sold under brand names such as Feratab, Fer-Iron, and Slow-FE. It is in complex with gluconate, dextran, carbonyl iron, and other salts. Ascorbic acid, vitamin C, increases the absorption of non-heme sources of iron.[37]
Heme iron polypeptide (HIP) (e.g. Proferrin ES and Proferrin Forte) can be used when regular iron supplements such as ferrous sulfate or ferrous fumarate are not tolerated or absorbed. A clinical study demonstrated that HIP increased serum iron levels 23 times greater than ferrous fumarate on a milligram-per-milligram basis.[38]
Another alternative is ferrous glycine sulfate or ferroglycine sulfate, has less gastrointestinal side-effects than standard preparations such as iron fumarate.[39] It is unusual among oral preparations of iron supplements in that the iron in this preparation has very high oral bioavailability, especially in the liquid formulation. This option should be evaluated before resorting to parenteral therapy. It is especially useful in iron deficiency anemia associated with autoimmune gastritis and Helicobacter pylori gastritis, where it generally has satisfactory effect.[40]
Since iron stores in the body are generally depleted, and there is a limit to what the body can process (about 2–6 mg/kg of body mass per day; i.e. for a 100 kg/220 lb man this is equal to a maximum dose of 200–600 mg/per day) without iron poisoning, this is a chronic therapy which may take 3–6 months.[41]
Due to the frequent intolerance of oral iron and the slow improvement, parenteral iron is recommended in many indications.[42][43]
By injection
Iron therapy (intravenously or intramuscular) is given when therapy by mouth has failed (not tolerated), oral absorption is seriously compromised (by illnesses, or when the person cannot swallow), benefit from oral therapy cannot be expected, or fast improvement is required (for example, prior to elective surgery).[44] Parenteral therapy is more expensive than oral iron preparations and is not suitable during the first trimester of pregnancy.[45]
There are cases where parenteral iron is preferable over oral iron. These are cases where oral iron is not tolerated, where the haemoglobin needs to be increased quickly (e.g. post partum, post operatively, post transfusion), where there is an underlying inflammatory condition (e.g. inflammatory bowel disease) or renal patients, the benefits of parenteral iron far outweigh the risks. In many cases, use of intravenous iron such as ferric carboxymaltose has lower risks of adverse events than a blood transfusion and as long as the person is stable is a better alternative.[46] Ultimately this always remains a clinical decision based on local guidelines, although National Guidelines are increasingly stipulating IV iron in certain groups of patients.[47][48]
Soluble iron salts have a significant risk of adverse effects and can cause toxicity due to damage to cellular macromolecules. Delivering iron parenterally has utilised various different molecules to limit this. This has included dextrans, sucrose, carboxymaltose and more recently Isomaltoside 1000.
One formulation of parenteral iron is iron dextran which covers the old high molecular weight (trade name DexFerrum) and the much safer low molecular iron dextrans (tradenames including Cosmofer and Infed).[49]
Iron sucrose has an occurrence of allergic reactions of less than 1 in 1000.[50] A common side effect is taste changes, especially a metallic taste, occurring in between 1 in 10 and 1 in 100 treated patients.[50] It has a maximum dose of 200 mg on each occasion according to the SPC, but it has been given in doses of 500 mg. Doses can be given up to 3 times a week.[51]
Iron carboxymaltose is marketed as Ferinject, Injectafer, and Iroprem in various countries.[52][53] The most common side effects are headaches which occur in 3.3%, and hypophosphatemia, which occurs in more than 35%.[54][55]
Iron Isomaltoside 1000 (Trade name Monofer) is a newer formulation of parenteral iron that has a matrix structure that results in very low levels of free iron and labile iron. It can be given at high doses – 20 mg/kg in a single visit – no upper dose limit. This formulation has the benefit of giving a full iron correction in a single visit.[56][53]
Follow-up
Follow-up is needed to ensure compliance and to detect adequate response to therapy. The interval of follow up can widely depend on both the method of administration, and the underlying pathology. For parenteral irons it is recommended that there be a period of 4 weeks before repeating blood test to allow the body to utilise the iron.[9] For oral iron, this can take considerably longer, so waiting three months may be appropriate.
See also
References
- Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 217. ISBN 9781284057560.
- British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. pp. 660–664. ISBN 9780857111562.
- World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. pp. 247–250. hdl:10665/44053. ISBN 9789241547659.
- "Iron Preparations, Oral". The American Society of Health-System Pharmacists. Archived from the original on 22 May 2016. Retrieved 8 January 2017.
- Upfal, Jonathan (2006). Australian Drug Guide. Black Inc. pp. 378–379. ISBN 9781863951746. Archived from the original on 2017-09-18.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- "Ferrous Sulfate - Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- Ferinject (ferric n 2012-12-21. Archived 2014-03-09 at the Wayback Machine
- Goddard AF, James MW, McIntyre AS and Scott BB (May 2005). Guidelines for the management of iron deficiency anaemia Archived 2012-04-22 at the Wayback Machine. British Society of Gastroenterology
- Litton, E; Xiao, J; Ho, KM (Aug 15, 2013). "Safety and efficacy of intravenous iron therapy in reducing requirement for allogeneic blood transfusion: systematic review and meta-analysis of randomised clinical trials". BMJ (Clinical Research Ed.). 347: f4822. doi:10.1136/bmj.f4822. PMC 3805480. PMID 23950195.
- Peña-Rosas JP, De-Regil LM, Garcia-Casal MN, Dowswell T (2015). "Daily oral iron supplementation during pregnancy". Cochrane Database Syst Rev. 2015 (7): CD0047361. doi:10.1002/14651858.CD004736.pub5. PMC 4233117. PMID 26198451.
- Peña-Rosas, Juan Pablo (19 October 2015). "Intermittent oral iron supplementation during pregnancy". Cochrane Database of Systematic Reviews. 2015 (10): CD009997. doi:10.1002/14651858.CD009997.pub2. PMC 7092533. PMID 26482110.
- "Taking iron supplements: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2018-08-11.
- Clénin G, Cordes M, Huber A, Schumacher YO, Noack P, Scales J, Kriemler S (2015). "Iron deficiency in sports – definition, influence on performance and therapy". Swiss Med Wkly (Review). 145: w14196. doi:10.4414/smw.2015.14196. PMID 26512429.
- "What you need to know about iron". Canadian Blood Services. Retrieved 30 May 2022.
- "Frequent Blood Donors and the Importance of Iron". American Red Cross Blood Services. Retrieved 30 May 2022.
- Smith, Graham; Fisher, Sheila; Doree, Carolyn; Di Angelantonio, Emanuele; Roberts, David (2014). "Oral or parenteral iron supplementation to reduce deferral, iron deficiency and/or anaemia in blood donors". Cochrane Database of Systematic Reviews (7): CD009532. doi:10.1002/14651858.CD009532.pub2. PMID 24990381. S2CID 205200473. Retrieved 31 May 2022.
- Geisser P (2007). "Safety and efficacy of iron(III)-hydroxide polymaltose complex / a review of over 25 years experience". Arzneimittelforschung. 57 (6A): 439–52. doi:10.1055/s-0031-1296693. PMID 17691594.
- Toblli JE, Brignoli R (2007). "Iron(III)-hydroxide polymaltose complex in iron deficiency anemia / review and meta-analysis". Arzneimittelforschung. 57 (6A): 431–8. doi:10.1055/s-0031-1296692. PMID 17691593.
- Saha L, Pandhi P, Gopalan S, Malhotra S, Saha PK (2007). "Comparison of efficacy, tolerability, and cost of iron polymaltose complex with ferrous sulfate in the treatment of iron deficiency anemia in pregnant women". MedGenMed. 9 (1): 1. PMC 1924983. PMID 17435611.
- Szarfarc SC, de Cassana LM, Fujimori E, Guerra-Shinohara EM, de Oliveira IM (2001). "Relative effectiveness of iron bis-glycinate chelate (Ferrochel) and ferrous sulfate in the control of iron deficiency in pregnant women". Arch Latinoam Nutr. 51 (1 Suppl 1): 42–7. PMID 11688081.
- Ashmead SD (2001). "The chemistry of ferrous bis-glycinate chelate". Arch Latinoam Nutr. 51 (1 Suppl 1): 7–12. PMID 11688084.
- Iron Toxicity at eMedicine
- Toxicity, Iron (Overview) Archived 2016-03-08 at the Wayback Machine. Tripdatabase.com. Retrieved on 2012-12-21.
- Oppenheimer, Stephen J. (2001). "Iron and its Relation to Immunity and Infectious Disease". The Journal of Nutrition. 131 (2): 616S–635S. doi:10.1093/jn/131.2.616S. PMID 11160594.
- Neuberger, A; Okebe, J; Yahav, D; Paul, M (27 February 2016). "Oral iron supplements for children in malaria-endemic areas". The Cochrane Database of Systematic Reviews. 2016 (2): CD006589. doi:10.1002/14651858.CD006589.pub4. PMC 4916933. PMID 26921618.
- CosmoFer – Summary of Product Characteristics (SPC) – (eMC) Archived 2014-04-26 at the Wayback Machine. Medicines.org.uk. Retrieved on 2012-12-21.
- Nielson, Peter; Nachtigall, Detlef (Oct 1998). "Iron supplementation in athletes: current recommendations" (PDF). Sports Med. 26 (4): 207–216. doi:10.2165/00007256-199826040-00001. PMID 9820921. S2CID 25517866. Retrieved 7 July 2013.
- Zjip, Itske; Korver, Onno; Tijburg, Lillian (2000). "Effect of Tea and Other Dietary Factors on Iron Absorption". Critical Reviews in Food Science and Nutrition. 40 (5): 371–398. doi:10.1080/10408690091189194. PMID 11029010. S2CID 12423113. Retrieved 31 May 2022.
- Delimont, Nicole; Haub, Mark; Lindshield, Brian (2017). "The Impact of Tannin Consumption on Iron Bioavailability and Status: A Narrative Review". Current Developments in Nutrition. 1 (2): e000042. doi:10.3945/cdn.116.000042. PMC 5998341. PMID 29955693.
- Reddy, MB; Hurrell, RF; Juillerat, MA; Cook, JD (1996). "The influence of different protein sources on phytate inhibition of nonheme-iron absorption in humans". American Journal of Clinical Nutrition. 63 (2): 203–207. doi:10.1093/ajcn/63.2.203. PMID 8561061.
- Mangels, Reed. Iron in the vegan diet. The Vegetarian Resource Group.
- Henjum, Sigrun; Groufh-Jacobsen, Synne; Stea, Tonja Holte; Tonheim, Live Edvardsen; Almendingen, Kari; Nurchi, Valeria (2021). "Iron Status of Vegans, Vegetarians and Pescatarians in Norway". Biomolecules. 11 (3): 454. doi:10.3390/biom11030454. PMC 8003004. PMID 33803700.
- Blaud's pill – Medical Definition and More from Archived 2010-02-19 at the Wayback Machine. Merriam-Webster. Retrieved on 2012-12-21.
- Robinson, Victor, ed. (1939). "P. Blaud of Beaucaire, Blaud's Pills for Anemia, Iron pills, Iron". The Modern Home Physician, A New Encyclopedia of Medical Knowledge. WM. H. Wise & Company (New York)., p. 435.
- Lynch, SR; Cook, JD (1980). "Interaction of vitamin C and iron". Annals of the New York Academy of Sciences. 355 (1): 32–44. Bibcode:1980NYASA.355...32L. CiteSeerX 10.1.1.530.1906. doi:10.1111/j.1749-6632.1980.tb21325.x. PMID 6940487. S2CID 35848195.
- Seligman, Paul A.; Moore, Gary M.; Schleicher, Rhoda B. (2000). "Clinical studies of hip: An oral heme-iron product". Nutrition Research. 20 (9): 1279–86. doi:10.1016/s0271-5317(00)00215-3.
- Aronstam, A.; Aston, D. (1982). "A comparative trial of a controlled-release iron tablet preparation ('Ferrocontin' Continus) and ferrous fumarate tablets". Pharmatherapeutica. 3 (4): 263–267. PMID 7146040.
- Hershko, C.; Ianculovich, M.; Souroujon, M. (2007). "Decreased Treatment Failure Rates following Duodenal Release Ferrous Glycine Sulfate in Iron Deficiency Anemia Associated with Autoimmune Gastritis and Helicobacter pylori Gastritis". Acta Haematologica. 118 (1): 19–26. doi:10.1159/000101701. PMID 17426393. S2CID 46720321.
- Iron Poisoning Archived 2012-04-12 at the Wayback Machine. Webmd.com (2012-09-27). Retrieved on 2012-12-21.
- National Clinical Guideline Centre (2015). Anaemia Management in Chronic Kidney Disease. NICE Guideline, No. 8. London: Royal College of Physicians. PMID 26065064. Archived from the original on 2017-09-18.
- Mowat, C; Cole, A; Windsor, A; Ahmad, T; Arnott, I; Driscoll, R; Mitton, S; Orchard, T; et al. (2011). "Guidelines for the management of inflammatory bowel disease in adults" (PDF). Gut. 60 (5): 571–607. doi:10.1136/gut.2010.224154. PMID 21464096. S2CID 8269837. Archived from the original (PDF) on 2013-06-21. Retrieved 2012-08-08.
- Kumpf, V. (1996). "Parenteral iron supplementation". Nutrition in Clinical Practice. 11 (4): 139–46. doi:10.1177/0115426596011004139. PMID 9070014.
- "Ferinject (ferric carboxymaltose) - Summary of Product Characteristics (SmPC) - (eMC)". Archived from the original on 2017-03-08. Retrieved 2017-03-07.
- Moore, R Andrew; Gaskell, Helen; Rose, Peter; Allan, Jonathan (2011). "Meta-analysis of efficacy and safety of intravenous ferric carboxymaltose (Ferinject) from clinical trial reports and published trial data". BMC Blood Disorders. 11: 4. doi:10.1186/1471-2326-11-4. PMC 3206450. PMID 21942989.
- Ponikowski, Piotr; Voors, Adriaan A.; Anker, Stefan D.; Bueno, Héctor; Cleland, John G. F.; Coats, Andrew J. S.; Falk, Volkmar; González-Juanatey, José Ramón; Harjola, Veli-Pekka; Jankowska, Ewa A.; Jessup, Mariell; Linde, Cecilia; Nihoyannopoulos, Petros; Parissis, John T.; Pieske, Burkert; Riley, Jillian P.; Rosano, Giuseppe M. C.; Ruilope, Luis M.; Ruschitzka, Frank; Rutten, Frans H.; Van Der Meer, Peter; ESC Scientific Document Group (2016). "2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure". European Heart Journal. 37 (27): 2129–2200. doi:10.1093/eurheartj/ehw128. PMID 27206819.
- Dignass, Axel U.; Gasche, Christoph; Bettenworth, Dominik; Birgegård, Gunnar; Danese, Silvio; Gisbert, Javier P.; Gomollon, Fernando; Iqbal, Tariq; Katsanos, Konstantinos; Koutroubakis, Ioannis; Magro, Fernando; Savoye, Guillaume; Stein, Jürgen; Vavricka, Stephan (2015). "European Consensus on the Diagnosis and Management of Iron Deficiency and Anaemia in Inflammatory Bowel Diseases". Journal of Crohn's and Colitis. 9 (3): 211–222. doi:10.1093/ecco-jcc/jju009. PMID 25518052.
- Chertow, Glenn M.; Mason, Phillip D.; Vaage-Nilsen, Odd; Ahlmén, Jarl (2004). "On the relative safety of parenteral iron formulations". Nephrology Dialysis Transplantation. 19 (6): 1571–5. doi:10.1093/ndt/gfh185. PMID 15150356.
- Venofer Archived 2011-10-01 at the Wayback Machine in FASS (drug formulary), translated from Swedish "Allergiska reaktioner (inträffar hos färre än 1 av 1 000 patienter)" and "Vanliga (inträffar hos färre än 1 av 10 patienter): Tillfälliga smakförändringar (speciellt metallsmak)."
- "Venofer (iron sucrose) - Summary of Product Characteristics (SmPC) - (eMC)". Archived from the original on 2017-03-08. Retrieved 2017-03-07.
- "Summary review: Application number 203565Orig1s000 by Luitpold Pharmaceuticals, Inc" (PDF). FDA. July 24, 2013. Archived (PDF) from the original on February 28, 2017.
- Cançado, Rodolfo Delfini; Muñoz, Manuel (2011). "Intravenous iron therapy". Revista Brasileira de Hematologia e Hemoterapia. 33 (6): 461–9. doi:10.5581/1516-8484.20110123. PMC 3459360. PMID 23049364.
- Ferinject (ferric carboxymaltose) – Summary of Product Characteristics (SPC) – (eMC) Archived 2014-03-09 at the Wayback Machine. Medicines.org.uk. Retrieved on 2012-12-21.
- "Injectafer US label" (PDF). FDA. July 2013. Archived (PDF) from the original on 2017-04-06. See FDA index page for NDA 203565 Archived 2017-04-07 at the Wayback Machine for updates and further information.
- Jahn, Markus R.; Andreasen, Hans B.; Fütterer, Sören; Nawroth, Thomas; Schünemann, Volker; Kolb, Ute; Hofmeister, Wolfgang; Muñoz, Manuel; Bock, Klaus; Meldal, Morten; Langguth, Peter (2011). "A comparative study of the physicochemical properties of iron isomaltoside 1000 (Monofer®), a new intravenous iron preparation and its clinical implications". European Journal of Pharmaceutics and Biopharmaceutics. 78 (3): 480–91. doi:10.1016/j.ejpb.2011.03.016. PMID 21439379.