Internal bleeding
Internal bleeding (also called internal hemorrhage) is a loss of blood from a blood vessel that collects inside the body. Internal bleeding is usually not visible from the outside.[1] It is a serious medical emergency but the extent of severity depends on bleeding rate and location of the bleeding (e.g. head, torso, extremities). Severe internal bleeding into the chest, abdomen, retroperitoneal space, pelvis, and thighs can cause hemorrhagic shock or death if proper medical treatment is not received quickly.[2] Internal bleeding is a medical emergency and should be treated immediately by medical professionals.[2]
| Internal bleeding | |
|---|---|
| Other names | Internal hemorrhage |
 | |
| Internal bleeding in the brain | |
| Complications | Hemorrhagic shock, hypovolemic shock, exsanguination |
Signs and symptoms
At first, there may be no symptoms of internal bleeding. If an organ is damaged and it bleeds, it can be painful. Over time, internal bleeding can cause low blood pressure (hypotension), increased heart rate (tachycardia), increased breathing rate (tachypnea), confusion, drowsiness, and loss of consciousness.[3]
A patient may lose more than 30% of their blood volume before there are changes in their vital signs or level of consciousness.[4] This is called hemorrhagic or hypovolemic shock, which is a type of shock that occurs when there is not enough blood to reach organs in the body.[5]
Early symptoms include anxiety, increased breathing rate, weak peripheral pulses, and cold skin on the arms and legs. If internal bleeding is not treated, the heart and breathing rate will continue to increase while blood pressure and mental status decrease. Eventually, internal bleeding can result in death by blood loss (exsanguination).[4] The median time from the onset of hemorrhagic shock to death by exsanguination is 2 hours.[4]
Causes
Trauma
The most common cause of death in trauma is bleeding.[6] Death from trauma accounts for 1.5 million of the 1.9 million deaths per year due to bleeding.[4]
There are two types of trauma: penetrating trauma and blunt trauma.[2]
- Penetrating trauma is the most common cause of vascular injury and can result in internal bleeding. It can occur after a ballistic injury or stab wound. If penetrating trauma occurs in blood vessels close to the heart, it can quickly lead to hemorrhagic or hypovolemic shock, exsanguination, and death.[2]
- Blunt trauma is another cause of vascular injury that can result in internal bleeding. It can occur after a high speed deceleration in an automobile accident.[2][7]
Non-traumatic
A number of pathological conditions and diseases can lead to internal bleeding. These include:
- Blood vessel rupture as a result of high blood pressure, aneurysms, esophageal varices, peptic ulcers, or ectopic pregnancy.[8]
- Other diseases linked to internal bleeding include cancer, hematologic disease, Vitamin K deficiency, and rare viral hemorrhagic fevers, such as the Ebola, Dengue or Marburg viruses.[9]
Other
Internal bleeding could be caused by medical error as a result of complications after surgical operations or medical treatment. Some medication effects may also lead to internal bleeding, such as the use of anticoagulant drugs or antiplatelet drugs in the treatment of coronary artery disease.[10]
Diagnosis
Vital signs
Blood loss can be estimated based on heart rate, blood pressure, respiratory rate, and mental status.[11] Advanced trauma life support (ATLS) by the American College of Surgeons separates hemorrhagic shock into four categories.[3][4][12]
| Estimated blood loss | Heart rate (per minute) | Blood pressure | Pulse pressure (mmHg) | Respiratory rate (per minute) | Other | |
|---|---|---|---|---|---|---|
| Class I hemorrhage | < 15% | Normal or minimally elevated | Normal | Normal | Normal |
|
| Class II hemorrhage | 15 - 30% | 100 - 120 | Normal or minimally decreased systolic blood pressure | Narrowed | 20 - 30 |
|
| Class III hemorrhage | 30 - 40% | 120 - 140 | Systolic blood pressure < 90 mmHg or change in blood pressure > 20-30% from presentation | Narrowed | 30 - 40 |
|
| Class IV hemorrhage | > 40% | > 140 | Systolic blood pressure < 90 mmHg | Narrowed (< 25 mmHg) | >35 |
|
Assessing circulation occurs after assessing the patient's airway and breathing (ABC (medicine)).[5] If internal bleeding is suspected, a patient's circulatory system is assessed through palpation of pulses and doppler ultrasonography.[2]
Physical examination
It is important to examine the person for visible signs that may suggest internal bleeding:[2]
- a wound
- bruising [ecchymosis]
- blood collection [hematoma]
- abnormal skin sensation [paresthesia]
- signs of compartment syndrome
It is also important to look for the source of the internal bleeding.[2] If internal bleeding is suspected after trauma, a FAST exam may be performed to look for bleeding in the abdomen.[2][3]
Imaging
If the patient has stable vital signs, they may undergo diagnostic imaging such as a CT scan.[4] If the patient has unstable vital signs, they may not undergo diagnostic imaging and instead may receive immediate medical or surgical treatment.[4]
By location
Internal bleeding can occur anywhere in the body. Some symptoms of internal bleeding depend on the location of the bleed. Some examples of types of internal bleeding include:
- Head: Intracranial hemorrhage, cerebral hemorrhage, subarachnoid hemorrhage, subdural hematoma, epidural hematoma
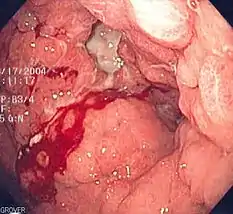
- Torso: cardiac tamponade, pulmonary hemorrhage, hemothorax, aortic aneurysm, gastrointestinal bleeding (upper gastrointestinal bleeding, lower gastrointestinal bleeding), blunt kidney trauma, splenic injury retroperitoneal bleeding, postpartum bleeding, ectopic pregnancy
- Extremities: bone fracture, hemarthrosis
Treatment
Management of internal bleeding depends on the cause and severity of the bleed. Internal bleeding is a medical emergency and should be treated immediately by medical professionals.[2]
Fluid replacement
If a patient has low blood pressure (hypotension), intravenous fluids can be used until they can receive a blood transfusion. In order to replace blood loss quickly and with large amounts of IV fluids or blood, patients may need a central venous catheter.[3] Patients with severe bleeding need to receive large quantities of replacement blood via a blood transfusion. As soon as the clinician recognizes that the patient may have a severe, continuing hemorrhage requiring more than 4 units in 1 hour or 10 units in 6 hours, they should initiate a massive transfusion protocol.[3] The massive transfusion protocol replaces red blood cells, plasma, and platelets in varying ratios based on the cause of the bleeding (traumatic vs. non-traumatic).[4]
Stopping the bleeding
.png.webp)
It is crucial to stop the internal bleeding immediately (achieve hemostasis) after identifying its cause.[4] The longer it takes to achieve hemostasis in people with traumatic causes (e.g. pelvic fracture) and non-traumatic causes (e.g. gastrointestinal bleeding, ruptured abdominal aortic aneurysm), the higher the death rate is.[4]
Unlike with external bleeding, most internal bleeding cannot be controlled by applying pressure to the site of injury.[3] Internal bleeding in the thorax and abdominal cavity (including both the intraperitoneal and retroperitoneal space) cannot be controlled with direct pressure (compression). A patient with acute internal bleeding in the thorax after trauma should be diagnosed, resuscitated, and stabilized in the Emergency Department in less than 10 minutes before undergoing surgery to reduce the risk of death from internal bleeding.[4] A patient with acute internal bleeding in the abdomen or pelvis after trauma may require use of a REBOA device to slow the bleeding.[4] The REBOA has also been used for non-traumatic causes of internal bleeding, including bleeding during childbirth and gastrointestinal bleeding.[4]
Internal bleeding from a bone fracture in the arms or legs may be partially controlled with direct pressure using a tourniquet.[3] After tourniquet placement, the patient may need immediate surgery to find the bleeding blood vessel.[4]
Internal bleeding where the torso meets the extremities ("junctional sites" such as the axilla or groin) cannot be controlled with a tourniquet; however there is an FDA approved device known as an Abdominal Aortic and Junctional Tourniquet (AAJT) designed for proximal aortic control, although very few studies examining its use have been published.[13][14][15][16][17][18] For bleeding at junctional sites, a dressing with a blood clotting agent (hemostatic dressing) should be applied.[4]
A campaign is to improve the care of the bleeding known as Stop The Bleed campaign is also taking place.[19]
References
- Auerback, Paul. Field Guide to Wilderness Medicine (PDF) (12 ed.). pp. 129–131. Retrieved 13 March 2019.
- Fritz, Davis (2011). "Vascular Emergencies". Current Diagnosis & Treatment: Emergency Medicine (7e ed.). New York: McGraw-Hill. ISBN 978-0071701075.
- Colwell, Christopher. "Initial management of moderate to severe hemorrhage in the adult trauma patient". UpToDate. Retrieved 5 March 2019.
- Cannon, Jeremy (January 25, 2018). "Hemorrhagic Shock". The New England Journal of Medicine. 378 (4): 370–379. doi:10.1056/NEJMra1705649. PMID 29365303. S2CID 205117992.
- International Trauma Life Support for Emergency Care Providers. Pearson Education Limited. 2018. pp. 172–173. ISBN 978-1292-17084-8.
- Teixeira, Pedro G. R.; Inaba, Kenji; Hadjizacharia, Pantelis; Brown, Carlos; Salim, Ali; Rhee, Peter; Browder, Timothy; Noguchi, Thomas T.; Demetriades, Demetrios (December 2007). "Preventable or Potentially Preventable Mortality at a Mature Trauma Center". The Journal of Trauma: Injury, Infection, and Critical Care. 63 (6): 1338–46, discussion 1346–7. doi:10.1097/TA.0b013e31815078ae. PMID 18212658.
- Duncan, Nicholas S.; Moran, Chris (2010). "(i) Initial resuscitation of the trauma victim". Orthopaedics and Trauma. 24: 1–8. doi:10.1016/j.mporth.2009.12.003.
- Lee, Edward W.; Laberge, Jeanne M. (2004). "Differential Diagnosis of Gastrointestinal Bleeding". Techniques in Vascular and Interventional Radiology. 7 (3): 112–122. doi:10.1053/j.tvir.2004.12.001. PMID 16015555.
- Bray, M. (2009). "Hemorrhagic Fever Viruses". Encyclopedia of Microbiology. pp. 339–353. doi:10.1016/B978-012373944-5.00303-5. ISBN 9780123739445.
- Pospíšil, Jan; Hromádka, Milan; Bernat, Ivo; Rokyta, Richard (2013). "STEMI - the importance of balance between antithrombotic treatment and bleeding risk". Cor et Vasa. 55 (2): e135–e146. doi:10.1016/j.crvasa.2013.02.004.
- Current Diagnosis & Treatment: Emergency Medicine. McGraw-Hill. 2011-05-23. ISBN 978-0071701075.
- ATLS- Advanced Trauma Life Support - Student Course Manual (10th ed.). American College of Surgeons. 2018. pp. 43–52. ISBN 978-78-0-9968267.
- Croushorn J. Abdominal Aortic and Junctional Tourniquet controls hemor-rhage from a gunshot wound of the left groin.JSpecOperMed.2014;14(2):6–8.
- Croushorn J, Thomas G, McCord SR. Abdominal aortic tourniquet controlsjunctional hemorrhage from a gunshot wound of the axilla.J Spec Oper Med.2013;13(3):1–4.
- Rall JM, Ross JD, Clemens MS, Cox JM, Buckley TA, Morrison JJ. Hemo-dynamic effects of the Abdominal Aortic and Junctional Tourniquet in ahemorrhagic swine model.JSurgRes. 2017;212:159–166.
- Kheirabadi BS, Terrazas IB, Miranda N, Voelker AN, Grimm R, Kragh JF Jr,Dubick MA. Physiological Consequences of Abdominal Aortic and Junc-tional Tourniquet (AAJT) application to control hemorrhage in a swinemodel.Shock (Augusta, Ga). 2016;46(3 Suppl 1):160–166.
- Taylor DM, Coleman M, Parker PJ. The evaluation of an abdominal aortictourniquet for the control of pelvic and lower limb hemorrhage.Mil Med.2013;178(11):1196–1201.
- Brannstrom A., Rocksen D., Hartman J., et al Abdominal aortic and junctional tourniquet release after 240 minutes is survivable and associated with small intestine and liver ischemia after porcine class II hemorrhage. J. Trauma Acute Care Surg.. 2018;85(4):717-724. doi:10.1097/TA.0000000000002013
- Pons, MD, Peter. "Stop the Bleed - SAVE A LIFE: What Everyone Should Know to Stop Bleeding After an Injury".