Esophageal varices
Esophageal varices are extremely dilated sub-mucosal veins in the lower third of the esophagus.[1] They are most often a consequence of portal hypertension,[2] commonly due to cirrhosis.[3] People with esophageal varices have a strong tendency to develop severe bleeding which left untreated can be fatal. Esophageal varices are typically diagnosed through an esophagogastroduodenoscopy.[4]
| Esophageal varices | |
|---|---|
| Other names | Esophageal varix, oesophageal varices |
 | |
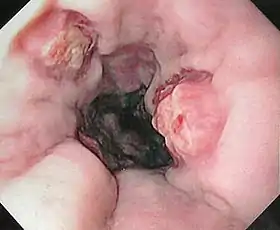
| Gastroscopy image of esophageal varices with prominent cherry-red spots | |
| Specialty | Gastroenterology, Hematology, Hepatology (liver disease) |
| Symptoms | vomiting blood passing black stool |
| Complications | Internal bleeding, hypovolemic shock, cardiac arrest |
| Causes | portal hypertension (high blood pressure in the portal vein and the associated blood vessels in the hepatic, or liver-based, circulation) |
| Diagnostic method | Endoscopy |
Pathogenesis
The upper two thirds of the esophagus are drained via the esophageal veins, which carry deoxygenated blood from the esophagus to the azygos vein, which in turn drains directly into the superior vena cava. These veins have no part in the development of esophageal varices. The lower one third of the esophagus is drained into the superficial veins lining the esophageal mucosa, which drain into the left gastric vein, which in turn drains directly into the portal vein. These superficial veins (normally only approximately 1 mm in diameter) become distended up to 1–2 cm in diameter in association with portal hypertension.
Normal portal pressure is approximately 9 mmHg compared to an inferior vena cava pressure of 2–6 mmHg. This creates a normal pressure gradient of 3–7 mmHg. If the portal pressure rises above 12 mmHg, this gradient rises to 7–10 mmHg.[5] A gradient greater than 5 mmHg is considered portal hypertension. At gradients greater than 10 mmHg, blood flowing through the hepatic portal system is redirected from the liver into areas with lower venous pressures. This means that collateral circulation develops in the lower esophagus, abdominal wall, stomach, and rectum. The small blood vessels in these areas become distended, becoming more thin-walled, and appear as varicosities.
In situations where portal pressures increase, such as with cirrhosis, there is dilation of veins in the anastomosis, leading to esophageal varices.[3] Splenic vein thrombosis is a rare condition that causes esophageal varices without a raised portal pressure. Splenectomy can cure the variceal bleeding due to splenic vein thrombosis.
Varices can also form in other areas of the body, including the stomach (gastric varices), duodenum (duodenal varices), and rectum (rectal varices). Treatment of these types of varices may differ. In some cases, schistosomiasis also leads to esophageal varices.
Histology

Dilated submucosal veins are the most prominent histologic feature of esophageal varices. The expansion of the submucosa leads to elevation of the mucosa above the surrounding tissue, which is apparent during endoscopy and is a key diagnostic feature. Evidence of recent variceal hemorrhage includes necrosis and ulceration of the mucosa. Evidence of past variceal hemorrhage includes inflammation and venous thrombosis.
Prevention

In ideal circumstances, people with known varices should receive treatment to reduce their risk of bleeding.[6] The non-selective β-blockers (e.g., propranolol, timolol or nadolol) and nitrates (e.g., isosorbide mononitrate (IMN) have been evaluated for secondary prophylaxis. Non-selective β-blockers (but not cardioselective β-blockers like atenolol) are preferred because they decrease both cardiac output by β1 blockade and splanchnic blood flow by blocking vasodilating β2 receptors at splanchnic vasculature. The effectiveness of this treatment has been shown by a number of different studies.[7]
However, non-selective β-blockers do not prevent the formation of esophageal varices.[8]
When medical contraindications to beta-blockers exist, such as significant reactive airway disease, then treatment with prophylactic endoscopic variceal ligation is often performed.[9]
Treatment
In emergency situations, care is directed at stopping blood loss, maintaining plasma volume, correcting disorders in coagulation induced by cirrhosis, and appropriate use of antibiotics such as quinolones or ceftriaxone. Blood volume resuscitation should be done promptly and with caution. The goal should be hemodynamic stability and hemoglobin of over 8 g/dl. Resuscitation of all lost blood leads to increase in portal pressure leading to more bleeding. Volume resuscitation can also worsen ascites and increase portal pressure. (AASLD guidelines)
Therapeutic endoscopy is considered the mainstay of urgent treatment. The two main therapeutic approaches are variceal ligation (banding) and sclerotherapy.
In cases of refractory bleeding, balloon tamponade with a Sengstaken-Blakemore tube may be necessary, usually as a bridge to further endoscopy or treatment of the underlying cause of bleeding (i.e.: portal hypertension). Esophageal devascularization operations such as the Sugiura procedure can also be used to stop complicated bleeding. Methods of treating the portal hypertension include: transjugular intrahepatic portosystemic shunt (TIPS), distal splenorenal shunt procedure, or liver transplantation.
Nutritional supplementation is necessary if the person has been unable to eat for more than four days.[10]
Terlipressin and octreotide for one to five days have also been used.[11]
See also
References
- Rubin, Raphael; Strayer, David S.; Rubin, Emanuel, eds. (2012). Rubin's Pathology: Clinicopathologic Foundations of Medicine (6th ed.). Lippincot Williams & Wilkins. p. 612. ISBN 9781605479682.
- Cushman, James (2018-01-01), Harken, Alden H.; Moore, Ernest E. (eds.), "Chapter 44 - Portal Hypertension and Esophageal Varices", Abernathy's Surgical Secrets (Seventh Edition), Elsevier, pp. 195–199, doi:10.1016/b978-0-323-47873-1.00044-9, ISBN 978-0-323-47873-1, retrieved 2020-11-23
- Awad, Joseph; Wattacheril, Julia (2012-01-01), Jarnagin, William R.; Blumgart, Leslie H. (eds.), "Chapter 75B - Esophageal varices: Acute management of portal hypertension", Blumgart's Surgery of the Liver, Pancreas and Biliary Tract (Fifth Edition), Philadelphia: W.B. Saunders, pp. 1135–1138.e1, doi:10.1016/b978-1-4377-1454-8.00120-x, ISBN 978-1-4377-1454-8, retrieved 2020-11-23
- Biecker E, Schepke M, Sauerbruch T (2005). "The role of endoscopy in portal hypertension". Dig Dis. 23 (1): 11–7. doi:10.1159/000084721. PMID 15920321.
- Arguedas M (2003). "The critically ill liver patient: the variceal bleeder". Semin Gastrointest Dis. 14 (1): 34–8. PMID 12610853.
- Lebrec D, Poynard T, Hillon P, Benhamou JP (1981). "Propranolol for prevention of recurrent gastrointestinal bleeding in patients with cirrhosis: a controlled study". N Engl J Med. 305 (23): 1371–1374. doi:10.1056/NEJM198112033052302. PMID 7029276.
- Talwalkar JA, Kamath PS (2004). "An evidence-based medicine approach to beta-blocker therapy in patients with cirrhosis". Am J Med. 116 (11): 759–766. doi:10.1016/j.amjmed.2004.03.006. PMID 15144913.
- Groszmann RJ, Garcia-Tsao G, Bosch J, et al. (2005). "Beta-Blockers to Prevent Gastroesophageal Varices in Patients with Cirrhosis" (PDF). N Engl J Med. 353 (21): 2254–2261. doi:10.1056/NEJMoa044456. PMID 16306522.
- Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W (2007). "Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis". Hepatology. 46 (3): 922–938. doi:10.1002/hep.21907. PMID 17879356.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - de Lédinghen V, Beau P, Mannant PR, et al. (1997). "Early feeding or enteral nutrition in patients with cirrhosis after bleeding from esophageal varices? A randomized controlled study". Dig. Dis. Sci. 42 (3): 536–41. doi:10.1023/A:1018838808396. PMID 9073135. S2CID 2819476.
- Abid S, Jafri W, Hamid S, et al. (March 2009). "Terlipressin vs. octreotide in bleeding esophageal varices as an adjuvant therapy with endoscopic band ligation: a randomized double-blind placebo-controlled trial". Am. J. Gastroenterol. 104 (3): 617–23. doi:10.1038/ajg.2008.147. PMID 19223890. S2CID 19130876.