Essential hypertension
Essential hypertension (also called primary hypertension, or idiopathic hypertension) is the form of hypertension that by definition has no identifiable secondary cause.[1][2] It is the most common type affecting 85% of those with high blood pressure.[3][4] The remaining 15% is accounted for by various causes of secondary hypertension.[3] Primary hypertension tends to be familial and is likely to be the consequence of an interaction between environmental and genetic factors. Prevalence of essential hypertension increases with age, and individuals with relatively high blood pressure at younger ages are at increased risk for the subsequent development of hypertension. Hypertension can increase the risk of cerebral, cardiac, and renal events.[5]
| Essential hypertension | |
|---|---|
| Other names | Primary hypertension |
| Specialty | Cardiology |
Classification
A recent classification recommends blood pressure criteria for defining normal blood pressure, prehypertension, hypertension (stages I and II), and isolated systolic hypertension, which is a common occurrence among the elderly. These readings are based on the average of seated blood pressure readings that were properly measured during 2 or more office visits. In individuals older than 50 years, hypertension is considered to be present when a person's blood pressure is consistently at least 140 mmHg systolic or 90 mmHg diastolic. Patients with blood pressures over 130/80 mmHg along with Type 1 or Type 2 diabetes, or kidney disease require further treatment.[6]
| Classification | Systolic pressure | Diastolic pressure | ||
|---|---|---|---|---|
| mmHg | kPa (kN/m2) | mmHg | kPa (kN/m2) | |
| Normal | 90–119 | 12–15.9 | 60–79 | 8.0–10.5 |
| Prehypertension | 120–139 | 16.1–18.5 | 80–89 | 10.8–11.9 |
| Stage 1 | 140–159 | 18.7–21.2 | 90–99 | 12.0–13.2 |
| Stage 2 | ≥160 | ≥21.3 | ≥100 | ≥13.3 |
| Isolated systolic hypertension |
≥140 | ≥18.7 | <90 | <12.0 |
| Source: American Heart Association (2003).[6] | ||||
Resistant hypertension is defined as the failure to reduce blood pressure to the appropriate level after taking a three-drug regimen.[6] Guidelines for treating resistant hypertension have been published in the UK, and US.[7]
Risk factors
Hypertension is one of the most common complex disorders. The etiology of hypertension differs widely amongst individuals within a large population.[8] And by definition, essential hypertension has no identifiable cause. However, several risk factors have been identified.
Genetic variation
- Having a personal family history of hypertension increases the likelihood that an individual develops it.[9]
- Essential hypertension is four times more common in black than white people, accelerates more rapidly and is often more severe with higher mortality in black patients.There are numerous racial inequities that contribute to black individuals having higher prevalence of essential hypertension than white people. These racial disparity-related risk factors are less conspicuous. Discrimination may have both a direct and indirect effect on hypertension. Chronic stress, like that caused by discrimination, has been linked to a number of health problems. Black people often have a higher risk profile, which includes factors including stress, family history of cardiovascular disease, low socioeconomic status, excess sodium intake, obesity, physical inactivity, and low socioeconomic position. Access to social, financial, and educational resources that can enhance one's health is unequally impacted by racial prejudice.Numerous studies have demonstrated the connection between feeling discriminated against and having elevated blood pressure. In comparison to participants who reported low levels of lifetime discrimination, a study from the Jackson Heart Study indicated that those people who reported high or medium levels of prejudice were more likely to acquire hypertension. Racial inequities are rarely acknowledged as significant risk factors in the healthcare industry.[10][11][12][9][13][14][15]
More than 50 genes have been examined in association studies with hypertension, and the number is constantly growing. One of these genes is the angiotensinogen (AGT) gene, studied extensively by Kim et al. They showed that increasing the number of AGT increases the blood pressure and hence this may cause hypertension.[8] In single variant tests, it has been shown that SNPs were enriched for variants associated with adiposity, type 2 diabetes, coronary heart disease and kidney function in previously published GWAS, providing evidence that genetic loci related to blood pressure contribute to cardiovascular outcomes.[16] Twins have been included in studies measuring ambulatory blood pressure; from these studies it has been suggested that there is a large genetic influence on essential hypertension.[8] Supporting data has emerged from animal studies as well as clinical studies in human populations. The majority of these studies support the concept that the inheritance is probably multifactorial or that a number of different genetic defects each has an elevated blood pressure as one of its phenotypic expressions. However, the genetic influence on hypertension is not fully understood at the moment. It is believed that linking hypertension-related phenotypes with specific variations of the genome may yield definitive evidence of heritability.[17] Another view is that hypertension can be caused by mutations in single genes, inherited on a Mendelian basis.[18]
Unhealthy diet
An unhealthy diet is a recognized risk factor for hypertension. A balanced diet is recommended for both its prevention and control.[19]
Aging
Hypertension can also be age-related when associated with a western diet and lifestyle, and if this is the case, it is likely to be multifactorial.[20] One possible mechanism involves a reduction in vascular compliance due to the stiffening of the arteries. This can build up due to isolated systolic hypertension with a widened pulse pressure. A decrease in glomerular filtration rate is related to aging and this results in decreasing efficiency of sodium excretion. The developing of certain diseases such as renal microvascular disease and capillary rarefaction may relate to this decrease in efficiency of sodium excretion. There is experimental evidence that suggests that renal microvascular disease is an important mechanism for inducing salt-sensitive hypertension.[21]
Obesity
Obesity can increase the risk of hypertension to fivefold as compared with normal weight, and up to two-thirds of hypertension cases can be attributed to excess weight.[22] More than 85% of cases occur in those with a Body mass index (BMI) greater than 25.[22] A definitive link between obesity and hypertension has been found using animal and clinical studies; from these it has been realized that many mechanisms are potential causes of obesity-induced hypertension. These mechanisms include the activation of the sympathetic nervous system as well as the activation of the renin–angiotensin–aldosterone system.[23]
Salt
Another risk factor is salt (sodium) sensitivity which is an environmental factor that has received the greatest attention. Approximately one third of the essential hypertensive population is responsive to sodium intake.[24][25] When sodium intake exceeds the capacity of the body to excrete it through the kidneys, vascular volume expands secondary to movement of fluids into the intra-vascular compartment. This causes the arterial pressure to rise as the cardiac output increases. Local autoregulatory mechanisms counteract this by increasing vascular resistance to maintain normotension in local vascular beds. As arterial pressure increases in response to high sodium chloride intake, urinary sodium excretion increases and the excretion of salt is maintained at expense of increased vascular pressures.[9] The increased sodium ion concentration stimulates ADH and thirst mechanisms, leading to increased reabsorption of water in the kidneys, concentrated urine, and thirst with higher intake of water. Also, the water movement between cells and the interstitium plays a minor role compared to this.
Alcohol
Excessive alcohol consumption will increase blood pressure over time. Alcohol also contains a high density of calories and may contribute to obesity.[26]
Renin
Renin elevation is another risk factor. Renin is an enzyme secreted by the juxtaglomerular apparatus of the kidney and linked with aldosterone in a negative feedback loop. In consequence, some hypertensive patients have been defined as having low-renin and others as having essential hypertension. Low-renin hypertension is more common in African Americans than white Americans, and may explain why African Americans tend to respond better to diuretic therapy than drugs that interfere with the renin–angiotensin system.
High renin levels predispose to hypertension by causing sodium retention through the following mechanism: Increased renin → Increased angiotensin II → Increased vasoconstriction, thirst/ADH and aldosterone → Increased sodium reabsorption in the kidneys (DCT and CD) → Increased blood pressure.
Diabetes
Hypertension can also be caused by Insulin resistance and/or hyperinsulinemia, which are components of syndrome X, or the metabolic syndrome. Insulin is a polypeptide hormone secreted by cells in the islets of Langerhans, which are contained throughout the pancreas. Its main purpose is to regulate the levels of glucose in the body antagonistically with glucagon through negative feedback loops. Insulin also exhibits vasodilatory properties. In normotensive individuals, insulin may stimulate sympathetic activity without elevating mean arterial pressure. However, in more extreme conditions such as that of the metabolic syndrome, the increased sympathetic neural activity may over-ride the vasodilatory effects of insulin.
Recent studies claim that obesity is a risk factor for hypertension because of activation of the renin–angiotensin system (RAS) in adipose tissue,[27][28] and also linked renin–angiotensin system with insulin resistance, and claims that any one can cause the other.[29]
Smoking
Smoking does not directly cause high blood pressure. However it is a known risk factor for other serious cardiovascular disease.[26]
Vitamin deficiency
It has been suggested that vitamin D deficiency is associated with cardiovascular risk factors.[30] It has been observed that individuals with a vitamin D deficiency have higher systolic and diastolic blood pressures than average. Vitamin D inhibits renin secretion and its activity, it therefore acts as a "negative endocrine regulator of the renin–angiotensin system". Hence, a deficiency in vitamin D leads to an increase in renin secretion. This is one possible mechanism of explaining the observed link between hypertension and vitamin D levels in the blood plasma.[31]
Also, some authorities claim that potassium might both prevent and treat hypertension.[32]
Lack of exercise
Regular physical exercise reduces blood pressure. The UK National Health Service advises 150 minutes (2 hours and 30 minutes) of moderate-intensity aerobic activity per week to help prevent hypertension.[26]
Pathophysiology

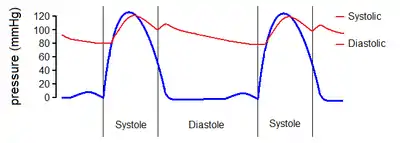
Cardiac output and peripheral resistance are the two determinants of arterial pressure and so blood pressure is normally dependent on the balance between cardiac output and peripheral resistance.[33] Cardiac output is determined by stroke volume and heart rate; stroke volume is related to myocardial contractility and to the size of the vascular compartment. Peripheral resistance is determined by functional and anatomic changes in small arteries and arterioles. The pathophysiology of essential hypertension is an area of research, and until now remains not well understood, but many theories have been proposed to explain this.
What is known is that cardiac output is raised early in the disease course, with total peripheral resistance (TPR) normal; over time cardiac output drops to normal levels but TPR is increased. Three theories have been proposed to explain this:
- An overactive Renin–angiotensin system leads to vasoconstriction and retention of sodium and water. The increase in blood volume leads to hypertension.
- An overactive sympathetic nervous system, leading to increased stress responses.
It is also known that hypertension is highly heritable and polygenic (caused by more than one gene) and a few candidate genes have been postulated in the etiology of this condition.[34][35][36] [37]
Essential hypertension can lead to impaired white matter of the brain, which is accompanied by specific cognitive impairment.[38]
Diagnosis
For most patients, health care providers diagnose high blood pressure when blood pressure readings are consistently 140/90 mmHg or above. A blood pressure test can be done in a health care provider's office or clinic. To track blood pressure readings over a period of time, the health care provider may ask the patient to come into the office on different days and at different times. The health care provider also may ask the patient to check readings at home or at other locations that have blood pressure equipment and to keep a written log of results. The health care provider usually takes 2–3 readings at several medical appointments to diagnose high blood pressure.[39] Using the results of the blood pressure test, the health care provider will diagnose prehypertension or high blood pressure if:
- For an adult, systolic or diastolic readings are consistently higher than 120/80 mmHg.
- A child's blood pressure numbers are outside average numbers for children of the same age, gender, and height.[39]
Once the health care provider determines the severity, he or she can order additional tests to determine if the blood pressure is due to other conditions or medicines or if there is primary high blood pressure. Health care providers can use this information to develop a treatment plan.[39]
History
Prior to the work of Australian cardiovascular physiologist Paul Korner, in the 1940s, little was known about essential hypertension.[40]
See also
References
- "Essential hypertension - Symptoms, diagnosis and treatment | BMJ Best Practice". bestpractice.bmj.com. Retrieved 30 July 2020.
- Hall, John (2011). Guyton and Hall textbook of medical physiology (Twelfth ed.). p. 225. ISBN 9781416045748.
- Ferri, Fred (2019). Ferri's clinical advisor 2019 : 5 books in 1. p. 729. ISBN 9780323530422.
- "Hypertension: eMedicine Nephrology". Retrieved 2009-06-05.
- Messerli FH, Williams B, Ritz E (August 2007). "Essential hypertension". Lancet. 370 (9587): 591–603. doi:10.1016/S0140-6736(07)61299-9. PMID 17707755. S2CID 26414121.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. (December 2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension. 42 (6): 1206–52. doi:10.1161/01.HYP.0000107251.49515.c2. PMID 14656957.
- Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. (June 2008). "Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research". Hypertension. 51 (6): 1403–19. doi:10.1161/HYPERTENSIONAHA.108.189141. PMID 18391085.
- Dickson ME, Sigmund CD (July 2006). "Genetic basis of hypertension: revisiting angiotensinogen". Hypertension. 48 (1): 14–20. doi:10.1161/01.HYP.0000227932.13687.60. PMID 16754793.
- Loscalzo J, Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL (2008). Harrison's principles of internal medicine. McGraw-Hill Medical. ISBN 978-0-07-147691-1.
- Wazlowski, S. (2020, September 1). Study: Racial discrimination can increase hypertension in blacks. The Nation's Health. Retrieved October 24, 2022, from https://www.thenationshealth.org/content/50/7/5.1
- Chester Hedgepeth, I. I. I. (2020, September 21). Discrimination, high blood pressure, and health disparities in African Americans. Harvard Health. Retrieved October 24, 2022, from https://www.health.harvard.edu/blog/discrimination-high-blood-pressure-and-health-disparities-in-african-americans-2020092120943
- Lackland DT. Racial differences in hypertension: implications for high blood pressure management. Am J Med Sci. 2014 Aug;348(2):135-8. doi: 10.1097/MAJ.0000000000000308. PMID: 24983758; PMCID: PMC4108512.
- Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M (July 1998). "Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction". The New England Journal of Medicine. 339 (4): 229–34. doi:10.1056/NEJM199807233390404. PMID 9673301.
- Lindhorst J, Alexander N, Blignaut J, Rayner B (2007). "Differences in hypertension between blacks and whites: an overview". Cardiovascular Journal of Africa. 18 (4): 241–7. PMC 4170224. PMID 17940670.
- Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, et al. (March 1995). "Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988-1991". Hypertension. 25 (3): 305–13. doi:10.1161/01.HYP.25.3.305. PMID 7875754. Archived from the original on 2012-12-05.
- Kato N, Loh M, Takeuchi F, Verweij N, Wang X, Zhang W, et al. (November 2015). "Trans-ancestry genome-wide association study identifies 12 genetic loci influencing blood pressure and implicates a role for DNA methylation". Nature Genetics. 47 (11): 1282–1293. doi:10.1038/ng.3405. PMC 4719169. PMID 26390057.
- Kotchen TA, Kotchen JM, Grim CE, George V, Kaldunski ML, Cowley AW, et al. (July 2000). "Genetic determinants of hypertension: identification of candidate phenotypes". Hypertension. 36 (1): 7–13. CiteSeerX 10.1.1.560.4838. doi:10.1161/01.HYP.36.1.7. PMID 10904005. Archived from the original on 2012-07-08.
- Williams B, et al. (British Hypertension Society) (2006). Sutters M (ed.). "Hypertension Etiology & Classification – Secondary Hypertension". Armenian Medical Network. Retrieved 2007-12-02.
- Mills KT, Stefanescu A, He J (February 2020). "The global epidemiology of hypertension". Nature Reviews Nephrology (16): 223–237. doi:10.1038/s41581-019-0244-2.
- Carrera-Bastos, Pedro; Fontes-Villalba, Maelan; O'Keefe, James H.; Lindeberg, Staffan; Cordain, Loren (2011-03-09). "The western diet and lifestyle and diseases of civilization". Research Reports in Clinical Cardiology. 2: 15–35. doi:10.2147/RRCC.S16919. Retrieved 2021-02-09.
- Kosugi T, Nakagawa T, Kamath D, Johnson RJ (February 2009). "Uric acid and hypertension: an age-related relationship?". Journal of Human Hypertension. 23 (2): 75–6. doi:10.1038/jhh.2008.110. PMID 18754017. S2CID 20887832.
- Haslam DW, James WP (October 2005). "Obesity". Lancet. 366 (9492): 1197–209. doi:10.1016/S0140-6736(05)67483-1. PMID 16198769. S2CID 208791491.
- Rahmouni K, Correia ML, Haynes WG, Mark AL (January 2005). "Obesity-associated hypertension: new insights into mechanisms". Hypertension. 45 (1): 9–14. doi:10.1161/01.HYP.0000151325.83008.b4. PMID 15583075.
- http://www.jstage.jst.go.jp/article/jphs/100/5/370/_pdf%5B%5D A Missing Link Between a High Salt Intake and Blood Pressure Increase: Makoto Katori and Masataka Majima, Department of Pharmacology, Kitasato University School of Medicine, Kitasato, Sagamihara, Kanagawa, Japan February 8, 2006
- http://hyper.ahajournals.org/content/27/3/481.full Salt Sensitivity of Blood Pressure in Humans Myron H. Weinberger Indiana University School of Medicine, Hypertension 1996 doi:10.1161/01.HYP.27.3.481
- "Prevention". nhs.uk. 2017-10-23. Retrieved 11 April 2018.
- Segura J, Ruilope LM (October 2007). "Obesity, essential hypertension and renin-angiotensin system". Public Health Nutrition. 10 (10A): 1151–5. doi:10.1017/S136898000700064X. PMID 17903324.
- Hasegawa H, Komuro I (April 2009). "[The progress of the study of RAAS]". Nihon Rinsho. Japanese Journal of Clinical Medicine (in Japanese). 67 (4): 655–61. PMID 19348224.
- Saitoh S (April 2009). "[Insulin resistance and renin-angiotensin-aldosterone system]". Nihon Rinsho. Japanese Journal of Clinical Medicine (in Japanese). 67 (4): 729–34. PMID 19348235.
- Lee JH, O'Keefe JH, Bell D, Hensrud DD, Holick MF (December 2008). "Vitamin D deficiency an important, common, and easily treatable cardiovascular risk factor?". Journal of the American College of Cardiology. 52 (24): 1949–56. doi:10.1016/j.jacc.2008.08.050. PMID 19055985.
- Forman JP, Giovannucci E, Holmes MD, Bischoff-Ferrari HA, Tworoger SS, Willett WC, Curhan GC (May 2007). "Plasma 25-hydroxyvitamin D levels and risk of incident hypertension". Hypertension. 49 (5): 1063–9. doi:10.1161/HYPERTENSIONAHA.107.087288. PMID 17372031.
- Eva May Nunnelley Hamilton, M.S., Eleanor Noss Whitney, R.D., Frances Sienkiewicz Sizer, M.S., R.D. (1991). Fifth Edition Annotated Instructor's Edition Nutrition Concepts & Controversies. West Publishing Company. ISBN 978-0-314-81092-2. OCLC 22451334.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Klabunde, Richard E. (2007). "Cardiovascular Physiology Concepts – Mean Arterial Pressure". Retrieved 2008-09-29.
- Sagnella GA, Swift PA (June 2006). "The renal epithelial sodium channel: genetic heterogeneity and implications for the treatment of high blood pressure". Current Pharmaceutical Design. 12 (18): 2221–34. doi:10.2174/138161206777585157. PMID 16787251.
- Johnson JA, Turner ST (June 2005). "Hypertension pharmacogenomics: current status and future directions". Current Opinion in Molecular Therapeutics. 7 (3): 218–25. PMID 15977418.
- Izawa H, Yamada Y, Okada T, Tanaka M, Hirayama H, Yokota M (May 2003). "Prediction of genetic risk for hypertension". Hypertension. 41 (5): 1035–40. doi:10.1161/01.HYP.0000065618.56368.24. PMID 12654703.
- Bello Inumidun Taofik (2017). diagnosis impact of hypertension
- Pervichko E, Ostroumova T, Darevskaya M, Perepelova E, Perepelov V, Vartanov A, et al. (2018). "A psychophysiological study ofcognitive disorders in naivemiddle-age patients withuncomplicated essential hypertensionand white matter lesions". European Psychiatry. 48S: 114.
- "Diagnosis of High Blood Pressure - NHLBI, NIH". National Institutes of Health.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "World authority on blood pressure: Paul Korner". Sydney Morning Herald. Fairfax Media. 30 November 2012.