Gastroenteritis
Gastroenteritis, also known as infectious diarrhea and gastro, is inflammation of the gastrointestinal tract including the stomach and intestine.[8] Symptoms may include diarrhea, vomiting, and abdominal pain.[1] Fever, lack of energy, and dehydration may also occur.[2][3] This typically lasts less than two weeks.[8] It is not related to influenza, even though in the U.S. it is sometimes called the "stomach flu".[9]
| Gastroenteritis | |
|---|---|
| Other names | Gastro, stomach bug, stomach virus, stomach flu, gastric flu, gastrointestinitis |
 | |
| Gastroenteritis viruses: A = rotavirus, B = adenovirus, C = norovirus and D = astrovirus. The virus particles are shown at the same magnification to allow size comparison. | |
| Specialty | Infectious disease, gastroenterology |
| Symptoms | Diarrhea, vomiting, abdominal pain, fever[1][2] |
| Complications | Dehydration[2][3] |
| Causes | Viruses, bacteria, parasites, fungus[2][4] |
| Diagnostic method | Based on symptoms, occasionally stool culture[2] |
| Differential diagnosis | Inflammatory bowel disease, malabsorption syndrome, lactose intolerance[5] |
| Prevention | Hand washing, drinking clean water, proper disposal of human waste, breastfeeding[2] |
| Treatment | Oral rehydration solution (combination of water, salts, and sugar), intravenous fluids[2] |
| Frequency | 2.4 billion (2015)[6] |
| Deaths | 1.3 million (2015)[7] |
Gastroenteritis is usually caused by viruses;[4] however, gut bacteria, parasites, and fungi can also cause gastroenteritis.[2][4] In children, rotavirus is the most common cause of severe disease.[10] In adults, norovirus and Campylobacter are common causes.[11][12] Eating improperly prepared food, drinking contaminated water or close contact with a person who is infected can spread the disease.[2] Treatment is generally the same with or without a definitive diagnosis, so testing to confirm is usually not needed.[2]
For young children in impoverished countries, prevention includes hand washing with soap, drinking clean water, breastfeeding babies instead of using formula,[2] and proper disposal of human waste. The rotavirus vaccine is recommended as a prevention for children.[2][10] Treatment involves getting enough fluids.[2] For mild or moderate cases, this can typically be achieved by drinking oral rehydration solution (a combination of water, salts and sugar).[2] In those who are breastfed, continued breastfeeding is recommended.[2] For more severe cases, intravenous fluids may be needed.[2] Fluids may also be given by a nasogastric tube.[13] Zinc supplementation is recommended in children.[2] Antibiotics are generally not needed.[14] However, antibiotics are recommended for young children with a fever and bloody diarrhea.[1]
In 2015, there were two billion cases of gastroenteritis, resulting in 1.3 million deaths globally.[6][7] Children and those in the developing world are affected the most.[15] In 2011, there were about 1.7 billion cases, resulting in about 700,000 deaths of children under the age of five.[16] In the developing world, children less than two years of age frequently get six or more infections a year.[17] It is less common in adults, partly due to the development of immunity.[18]
Signs and symptoms
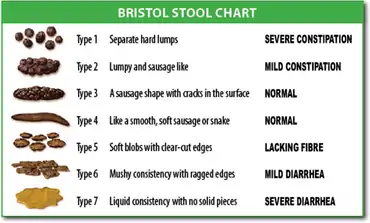
Gastroenteritis usually involves both diarrhea and vomiting.[18] Sometimes, only one or the other is present.[1] This may be accompanied by abdominal cramps.[1] Signs and symptoms usually begin 12–72 hours after contracting the infectious agent.[15] If due to a virus, the condition usually resolves within one week.[18] Some viral infections also involve fever, fatigue, headache and muscle pain.[18] If the stool is bloody, the cause is less likely to be viral[18] and more likely to be bacterial.[19] Some bacterial infections cause severe abdominal pain and may persist for several weeks.[19]
Children infected with rotavirus usually make a full recovery within three to eight days.[20] However, in poor countries treatment for severe infections is often out of reach and persistent diarrhea is common.[21] Dehydration is a common complication of diarrhea.[22] Severe dehydration in children may be recognized if the skin color and position returns slowly when pressed.[23] This is called "prolonged capillary refill" and "poor skin turgor".[23] Abnormal breathing is another sign of severe dehydration.[23] Repeat infections are typically seen in areas with poor sanitation, and malnutrition.[15] Stunted growth and long-term cognitive delays can result.[17]
Reactive arthritis occurs in 1% of people following infections with Campylobacter species.[19] Guillain–Barré syndrome occurs in 0.1%.[19] Hemolytic uremic syndrome (HUS) may occur due to infection with Shiga toxin-producing Escherichia coli or Shigella species.[24] HUS causes low platelet counts, poor kidney function, and low red blood cell count (due to their breakdown).[24] Children are more predisposed to getting HUS than adults.[17] Some viral infections may produce benign infantile seizures.[1]
Cause
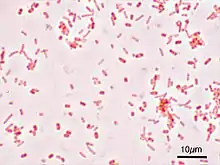
Viruses (particularly rotavirus (in children) and norovirus (in adults)) and the bacteria Escherichia coli and Campylobacter species are the primary causes of gastroenteritis.[15][25] There are, however, many other infectious agents that can cause this syndrome including parasites and fungus.[17][4] Non-infectious causes are seen on occasion, but they are less likely than a viral or bacterial cause.[1] Risk of infection is higher in children due to their lack of immunity.[1] Children are also at higher risk because they are less likely to practice good hygiene habits.[1] Children living in areas without easy access to water and soap are especially vulnerable.[1]
Viral
Rotaviruses, noroviruses, adenoviruses, and astroviruses are known to cause viral gastroenteritis.[26] Rotavirus is the most common cause of gastroenteritis in children,[25] and produces similar rates in both the developed and developing world.[20] Viruses cause about 70% of episodes of infectious diarrhea in the pediatric age group.[13] Rotavirus is a less common cause in adults due to acquired immunity.[27] Norovirus is the cause in about 18% of all cases.[28] Generally speaking, viral gastroenteritis accounts for 21–40% of the cases of infectious diarrhea in developed countries.[29]
Norovirus is the leading cause of gastroenteritis among adults in America accounting for about 90% of viral gastroenteritis outbreaks.[18] These localized epidemics typically occur when groups of people spend time proximate to each other, such as on cruise ships,[18] in hospitals, or in restaurants.[1] People may remain infectious even after their diarrhea has ended.[18] Norovirus is the cause of about 10% of cases in children.[1]
Bacterial
In some countries, Campylobacter jejuni is the primary cause of bacterial gastroenteritis, with half of these cases associated with exposure to poultry.[19] In children, bacteria are the cause in about 15% of cases, with the most common types being Escherichia coli, Salmonella, Shigella, and Campylobacter species.[13] If food becomes contaminated with bacteria and remains at room temperature for a period of several hours, the bacteria multiply and increase the risk of infection in those who consume the food.[17] Some foods commonly associated with illness include raw or undercooked meat, poultry, seafood, and eggs; raw sprouts; unpasteurized milk and soft cheeses; and fruit and vegetable juices.[30] In the developing world, especially sub-Saharan Africa and Asia, cholera is a common cause of gastroenteritis. This infection is usually transmitted by contaminated water or food.[31]
Toxigenic Clostridium difficile is an important cause of diarrhea that occurs more often in the elderly.[17] Infants can carry these bacteria without developing symptoms.[17] It is a common cause of diarrhea in those who are hospitalized and is frequently associated with antibiotic use.[32] Staphylococcus aureus infectious diarrhea may also occur in those who have used antibiotics.[33] Acute "traveler's diarrhea" is usually a type of bacterial gastroenteritis, while the persistent form is usually parasitic.[34] Acid-suppressing medication appears to increase the risk of significant infection after exposure to a number of organisms, including Clostridium difficile, Salmonella, and Campylobacter species.[35] The risk is greater in those taking proton pump inhibitors than with H2 antagonists.[35]
Parasitic
A number of parasites can cause gastroenteritis.[13] Giardia lamblia is most common, but Entamoeba histolytica, Cryptosporidium spp., and other species have also been implicated.[13][34] As a group, these agents comprise about 10% of cases in children.[24][34] Giardia occurs more commonly in the developing world, but this type of illness can occur nearly everywhere.[36] It occurs more commonly in persons who have traveled to areas with high prevalence, children who attend day care, men who have sex with men, and following disasters.[36]
Transmission
Transmission may occur from drinking contaminated water or when people share personal objects.[15] Water quality typically worsens during the rainy season and outbreaks are more common at this time.[15] In areas with four seasons, infections are more common in the winter.[17] Worldwide, bottle-feeding of babies with improperly sanitized bottles is a significant cause.[15] Transmission rates are also related to poor hygiene, (especially among children),[18] in crowded households,[37] and in those with poor nutritional status.[17] Adults who have developed immunities might still carry certain organisms without exhibiting symptoms.[17] Thus, adults can become natural reservoirs of certain diseases.[17] While some agents (such as Shigella) only occur in primates, others (such as Giardia) may occur in a wide variety of animals.[17]
Non-infectious
There are a number of non-infectious causes of inflammation of the gastrointestinal tract.[1] Some of the more common include medications (like NSAIDs), certain foods such as lactose (in those who are intolerant), and gluten (in those with celiac disease). Crohn's disease is also a non-infectious source of (often severe) gastroenteritis.[1] Disease secondary to toxins may also occur. Some food-related conditions associated with nausea, vomiting, and diarrhea include: ciguatera poisoning due to consumption of contaminated predatory fish, scombroid associated with the consumption of certain types of spoiled fish, tetrodotoxin poisoning from the consumption of puffer fish among others, and botulism typically due to improperly preserved food.[38]
In the United States, rates of emergency department use for noninfectious gastroenteritis dropped 30% from 2006 until 2011. Of the twenty most common conditions seen in the emergency department, rates of noninfectious gastroenteritis had the largest decrease in visits in that time period.[39]
Pathophysiology
Gastroenteritis is defined as vomiting or diarrhea due to inflammation of the small or large bowel, often due to infection.[17] The changes in the small bowel are typically noninflammatory, while the ones in the large bowel are inflammatory.[17] The number of pathogens required to cause an infection varies from as few as one (for Cryptosporidium) to as many as 108 (for Vibrio cholerae).[17]
Diagnosis
Gastroenteritis is typically diagnosed clinically, based on a person's signs and symptoms.[18] Determining the exact cause is usually not needed as it does not alter the management of the condition.[15]
However, stool cultures should be performed in those with blood in the stool, those who might have been exposed to food poisoning, and those who have recently traveled to the developing world.[13] It may also be appropriate in children younger than 5, old people, and those with poor immune function.[40] Diagnostic testing may also be done for surveillance.[18] As hypoglycemia occurs in approximately 10% of infants and young children, measuring serum glucose in this population is recommended.[23] Electrolytes and kidney function should also be checked when there is a concern about severe dehydration.[13]
Dehydration
A determination of whether or not the person has dehydration is an important part of the assessment, with dehydration typically divided into mild (3–5%), moderate (6–9%), and severe (≥10%) cases.[1] In children, the most accurate signs of moderate or severe dehydration are a prolonged capillary refill, poor skin turgor, and abnormal breathing.[23][41] Other useful findings (when used in combination) include sunken eyes, decreased activity, a lack of tears, and a dry mouth.[1] A normal urinary output and oral fluid intake is reassuring.[23] Laboratory testing is of little clinical benefit in determining the degree of dehydration.[1] Thus the use of urine testing or ultrasounds is generally not needed.[42]
Differential diagnosis
Other potential causes of signs and symptoms that mimic those seen in gastroenteritis that need to be ruled out include appendicitis, volvulus, inflammatory bowel disease, urinary tract infections, and diabetes mellitus.[13] Pancreatic insufficiency, short bowel syndrome, Whipple's disease, coeliac disease, and laxative abuse should also be considered.[43] The differential diagnosis can be complicated somewhat if the person exhibits only vomiting or diarrhea (rather than both).[1]
Appendicitis may present with vomiting, abdominal pain, and a small amount of diarrhea in up to 33% of cases.[1] This is in contrast to the large amount of diarrhea that is typical of gastroenteritis.[1] Infections of the lungs or urinary tract in children may also cause vomiting or diarrhea.[1] Classical diabetic ketoacidosis (DKA) presents with abdominal pain, nausea, and vomiting, but without diarrhea.[1] One study found that 17% of children with DKA were initially diagnosed as having gastroenteritis.[1]
Prevention
Water, sanitation, hygiene
A supply of easily accessible uncontaminated water and good sanitation practices are important for reducing rates of infection and clinically significant gastroenteritis.[17] Personal hygiene measures (such as hand washing with soap) have been found to decrease rates of gastroenteritis in both the developing and developed world by as much as 30%.[23] Alcohol-based gels may also be effective.[23] Food or drink that is thought to be contaminated should be avoided.[44] Breastfeeding is important, especially in places with poor hygiene, as is improvement of hygiene generally.[15] Breast milk reduces both the frequency of infections and their duration.[1]
Vaccination
Due to both its effectiveness and safety, in 2009 the World Health Organization recommended that the rotavirus vaccine be offered to all children globally.[25][45] Two commercial rotavirus vaccines exist and several more are in development.[45] In Africa and Asia these vaccines reduced severe disease among infants[45] and countries that have put in place national immunization programs have seen a decline in the rates and severity of disease.[46][47] This vaccine may also prevent illness in non-vaccinated children by reducing the number of circulating infections.[48] Since 2000, the implementation of a rotavirus vaccination program in the United States has substantially decreased the number of cases of diarrhea by as much as 80 percent.[49][50][51] The first dose of vaccine should be given to infants between 6 and 15 weeks of age.[25] The oral cholera vaccine has been found to be 50–60% effective over two years.[52]
There are a number of vaccines against gastroenteritis in development. For example, vaccines against Shigella and enterotoxigenic Escherichia coli (ETEC), which are two of the leading bacterial causes of gastroenteritis worldwide.[53][54]
Management
Gastroenteritis is usually an acute and self-limiting disease that does not require medication.[22] The preferred treatment in those with mild to moderate dehydration is oral rehydration therapy (ORT).[24] For children at risk of dehydration from vomiting, taking a single dose of the anti vomiting medication metoclopramide or ondansetron, may be helpful,[55] and butylscopolamine is useful in treating abdominal pain.[56]
Rehydration
The primary treatment of gastroenteritis in both children and adults is rehydration. This is preferably achieved by drinking rehydration solution, although intravenous delivery may be required if there is a decreased level of consciousness or if dehydration is severe.[57][58] Drinking replacement therapy products made with complex carbohydrates (i.e. those made from wheat or rice) may be superior to those based on simple sugars.[59] Drinks especially high in simple sugars, such as soft drinks and fruit juices, are not recommended in children under five years of age as they may increase diarrhea.[22] Plain water may be used if more specific ORT preparations are unavailable or the person is not willing to drink them.[22] A nasogastric tube can be used in young children to administer fluids if warranted.[13] In those who require intravenous fluids, one to four hours' worth is often sufficient.[60]
Dietary
It is recommended that breast-fed infants continue to be nursed in the usual fashion, and that formula-fed infants continue their formula immediately after rehydration with ORT.[61] Lactose-free or lactose-reduced formulas usually are not necessary.[61] Children should continue their usual diet during episodes of diarrhea with the exception that foods high in simple sugars should be avoided.[61] The BRAT diet (bananas, rice, applesauce, toast and tea) is no longer recommended, as it contains insufficient nutrients and has no benefit over normal feeding.[61]
A Cochrane Review from 2020 concludes that probiotics make little or no difference to people who have diarrhea lasting 2 days or longer and that there is no proof that they reduce its duration.[62] They may be useful in preventing and treating antibiotic associated diarrhea.[63] Fermented milk products (such as yogurt) are similarly beneficial.[64] Zinc supplementation appears to be effective in both treating and preventing diarrhea among children in the developing world.[65]
Antiemetics
Antiemetic medications may be helpful for treating vomiting in children. Ondansetron has some utility, with a single dose being associated with less need for intravenous fluids, fewer hospitalizations, and decreased vomiting.[55][66][67][68] Metoclopramide might also be helpful.[68] However, the use of ondansetron might possibly be linked to an increased rate of return to hospital in children.[69] The intravenous preparation of ondansetron may be given orally if clinical judgment warrants.[70] Dimenhydrinate, while reducing vomiting, does not appear to have a significant clinical benefit.[1]
Antibiotics
Antibiotics are not usually used for gastroenteritis, although they are sometimes recommended if symptoms are particularly severe[71] or if a susceptible bacterial cause is isolated or suspected.[72] If antibiotics are to be employed, a macrolide (such as azithromycin) is preferred over a fluoroquinolone due to higher rates of resistance to the latter.[19] Pseudomembranous colitis, usually caused by antibiotic use, is managed by discontinuing the causative agent and treating it with either metronidazole or vancomycin.[73] Bacteria and protozoans that are amenable to treatment include Shigella[74] Salmonella typhi,[75] and Giardia species.[36] In those with Giardia species or Entamoeba histolytica, tinidazole treatment is recommended and superior to metronidazole.[36][76] The World Health Organization (WHO) recommends the use of antibiotics in young children who have both bloody diarrhea and fever.[1]
Antimotility agents
Antimotility medication has a theoretical risk of causing complications, and although clinical experience has shown this to be unlikely,[43] these drugs are discouraged in people with bloody diarrhea or diarrhea that is complicated by fever.[77] Loperamide, an opioid analogue, is commonly used for the symptomatic treatment of diarrhea.[78] Loperamide is not recommended in children, however, as it may cross the immature blood–brain barrier and cause toxicity. Bismuth subsalicylate, an insoluble complex of trivalent bismuth and salicylate, can be used in mild to moderate cases,[43] but salicylate toxicity is theoretically possible.[1]
Epidemiology
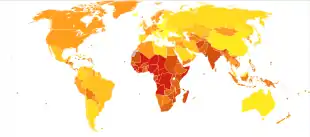
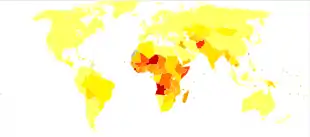
|
no data
≤less 500
500–1000
1000–1500
1500–2000
2000–2500
2500–3000 |
3000–3500
3500–4000
4000–4500
4500–5000
5000–6000
≥6000
|
It is estimated that there were two billion cases of gastroenteritis that resulted in 1.3 million deaths globally in 2015.[6][7] Children and those in the developing world are most commonly affected.[15] As of 2011, in those younger than five, there were about 1.7 billion cases resulting in 0.7 million deaths,[16] with most of these occurring in the world's poorest nations.[17] More than 450,000 of these fatalities are due to rotavirus in children under five years of age.[10][79] Cholera causes about three to five million cases of disease and kills approximately 100,000 people yearly.[31] In the developing world, children less than two years of age frequently get six or more infections a year that result in significant gastroenteritis.[17] It is less common in adults, partly due to the development of acquired immunity.[18]
In 1980, gastroenteritis from all causes caused 4.6 million deaths in children, with the majority occurring in the developing world.[73] Death rates were reduced significantly (to approximately 1.5 million deaths annually) by 2000, largely due to the introduction and widespread use of oral rehydration therapy.[80] In the US, infections causing gastroenteritis are the second most common infection (after the common cold), and they result in between 200 and 375 million cases of acute diarrhea[17][18] and approximately ten thousand deaths annually,[17] with 150 to 300 of these deaths in children less than five years of age.[1]
Society and culture
Gastroenteritis is associated with many colloquial names, including "Montezuma's revenge", "Delhi belly", "la turista", and "back door sprint", among others.[17] It has played a role in many military campaigns and is believed to be the origin of the term "no guts no glory".[17]
Gastroenteritis is the main reason for 3.7 million visits to physicians a year in the United States[1] and 3 million visits in France.[81] In the United States gastroenteritis as a whole is believed to result in costs of US$23 billion per year[82] with that due to rotavirus alone resulting in estimated costs of US$1 billion a year.[1]
Terminology
The first usage of "gastroenteritis" was in 1825.[83] Before this time it was commonly known as typhoid fever or "cholera morbus", among others, or less specifically as "griping of the guts", "surfeit", "flux", "colic", "bowel complaint", or any one of a number of other archaic names for acute diarrhea.[84] Cholera morbus is a historical term that was used to refer to gastroenteritis rather than specifically cholera.[85]
Other animals
Many of the same agents cause gastroenteritis in cats and dogs as in humans. The most common organisms are Campylobacter, Clostridium difficile, Clostridium perfringens, and Salmonella.[86] A large number of toxic plants may also cause symptoms.[87]
Some agents are more specific to a certain species. Transmissible gastroenteritis coronavirus (TGEV) occurs in pigs resulting in vomiting, diarrhea, and dehydration.[88] It is believed to be introduced to pigs by wild birds and there is no specific treatment available.[89] It is not transmissible to humans.[90]
See also
References
- Singh, Amandeep (July 2010). "Pediatric Emergency Medicine Practice Acute Gastroenteritis — An Update". Pediatric Emergency Medicine Practice. 7 (7).
- Ciccarelli, S; Stolfi, I; Caramia, G (29 October 2013). "Management strategies in the treatment of neonatal and pediatric gastroenteritis". Infection and Drug Resistance. 6: 133–61. doi:10.2147/IDR.S12718. PMC 3815002. PMID 24194646.
- Ferri's Clinical Advisor 2015: 5 Books in 1. Elsevier Health Sciences. 2014. p. 479. ISBN 978-0-323-08430-7. Archived from the original on 2017-09-08.
- A. Helms, Richard (2006). Textbook of therapeutics : drug and disease management (8. ed.). Philadelphia [u.a.]: Lippincott Williams & Wilkins. p. 2003. ISBN 978-0-7817-5734-8. Archived from the original on 2017-09-08.
- Caterino, Jeffrey M.; Kahan, Scott (2003). In a Page: Emergency medicine. Lippincott Williams & Wilkins. p. 293. ISBN 978-1-4051-0357-2. Archived from the original on 2017-09-08.
- GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
{{cite journal}}:|first1=has generic name (help) - GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
{{cite journal}}:|first1=has generic name (help) - Schlossberg, David (2015). Clinical infectious disease (Second ed.). p. 334. ISBN 978-1-107-03891-2. Archived from the original on 2017-09-08.
- Shors, Teri (2013). The microbial challenge : a public health perspective (3rd ed.). Burlington, MA: Jones & Bartlett Learning. p. 457. ISBN 978-1-4496-7333-8. Archived from the original on 2017-09-08.
- Tate JE, Burton AH, Boschi-Pinto C, Steele AD, Duque J, Parashar UD (February 2012). "2008 estimate of worldwide rotavirus-associated mortality in children younger than 5 years before the introduction of universal rotavirus vaccination programmes: a systematic review and meta-analysis". The Lancet Infectious Diseases. 12 (2): 136–41. doi:10.1016/S1473-3099(11)70253-5. PMID 22030330.
- Marshall JA, Bruggink LD (April 2011). "The dynamics of norovirus outbreak epidemics: recent insights". International Journal of Environmental Research and Public Health. 8 (4): 1141–9. doi:10.3390/ijerph8041141. PMC 3118882. PMID 21695033.
- Man SM (December 2011). "The clinical importance of emerging Campylobacter species". Nature Reviews Gastroenterology & Hepatology. 8 (12): 669–85. doi:10.1038/nrgastro.2011.191. PMID 22025030. S2CID 24103030.
- Webb, A; Starr, M (April 2005). "Acute gastroenteritis in children". Australian Family Physician. 34 (4): 227–31. PMID 15861741.
- Zollner-Schwetz, I; Krause, R (August 2015). "Therapy of acute gastroenteritis: role of antibiotics". Clinical Microbiology and Infection. 21 (8): 744–9. doi:10.1016/j.cmi.2015.03.002. PMID 25769427.
- Webber, Roger (2009). Communicable disease epidemiology and control : a global perspective (3rd ed.). Wallingford, Oxfordshire: Cabi. p. 79. ISBN 978-1-84593-504-7. Archived from the original on 2015-10-26.
- Walker, CL; Rudan, I; Liu, L; Nair, H; Theodoratou, E; Bhutta, ZA; O'Brien, KL; Campbell, H; Black, RE (Apr 20, 2013). "Global burden of childhood pneumonia and diarrhoea". Lancet. 381 (9875): 1405–16. doi:10.1016/S0140-6736(13)60222-6. PMC 7159282. PMID 23582727.
- Dolin, Raphael; Mandell, Gerald L.; Bennett, John E., eds. (2010). "Chapter 93". Mandell, Douglas, and Bennett's principles and practice of infectious diseases (7th ed.). Philadelphia: Churchill Livingstone/Elsevier. ISBN 978-0-443-06839-3.
- Eckardt AJ, Baumgart DC (January 2011). "Viral gastroenteritis in adults". Recent Patents on Anti-Infective Drug Discovery. 6 (1): 54–63. doi:10.2174/157489111794407877. PMID 21210762.
- Galanis, E (11 September 2007). "Campylobacter and bacterial gastroenteritis". Canadian Medical Association Journal. 177 (6): 570–1. doi:10.1503/cmaj.070660. PMC 1963361. PMID 17846438.
- Meloni, A; Locci, D; Frau, G; Masia, G; Nurchi, AM; Coppola, RC (October 2011). "Epidemiology and prevention of rotavirus infection: an underestimated issue?". Journal of Maternal-Fetal and Neonatal Medicine. 24 (Suppl 2): 48–51. doi:10.3109/14767058.2011.601920. PMID 21749188. S2CID 44379279.
- "Toolkit". DefeatDD. Archived from the original on 27 April 2012. Retrieved 3 May 2012.
- "Management of acute diarrhoea and vomiting due to gastoenteritis in children under 5". National Institute of Clinical Excellence. April 2009. Archived from the original on 2009-08-02. Retrieved 2009-06-11.
- Tintinalli, Judith E. (2010). Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine (Tintinalli)). New York: McGraw-Hill Companies. pp. 830–839. ISBN 978-0-07-148480-0.
- Elliott, EJ (6 January 2007). "Acute gastroenteritis in children". The BMJ. 334 (7583): 35–40. doi:10.1136/bmj.39036.406169.80. PMC 1764079. PMID 17204802.
- Szajewska, H; Dziechciarz, P (January 2010). "Gastrointestinal infections in the pediatric population". Current Opinion in Gastroenterology. 26 (1): 36–44. doi:10.1097/MOG.0b013e328333d799. PMID 19887936. S2CID 5083478.
- Barlow, Gavin; Irving, William L.; Moss, Peter J. (2020). "20. Infectious disease". In Feather, Adam; Randall, David; Waterhouse, Mona (eds.). Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. pp. 529–530. ISBN 978-0-7020-7870-5.
- Desselberger U, Huppertz HI (January 2011). "Immune responses to rotavirus infection and vaccination and associated correlates of protection". The Journal of Infectious Diseases. 203 (2): 188–95. doi:10.1093/infdis/jiq031. PMC 3071058. PMID 21288818.
- Ahmed, Sharia M; Hall, Aron J; Robinson, Anne E; Verhoef, Linda; Premkumar, Prasanna; Parashar, Umesh D; Koopmans, Marion; Lopman, Benjamin A (Aug 2014). "Global prevalence of norovirus in cases of gastroenteritis: a systematic review and meta-analysis". The Lancet Infectious Diseases. 14 (8): 725–30. doi:10.1016/S1473-3099(14)70767-4. PMC 8006533. PMID 24981041.
- Baumgart, Alexander J. Eckardt and Daniel C. (2010-12-31). "Viral Gastroenteritis in Adults". Recent Patents on Anti-Infective Drug Discovery. 6 (1): 54–63. doi:10.2174/157489111794407877. PMID 21210762. Retrieved 2020-12-22.
- Nyachuba, DG (May 2010). "Foodborne illness: is it on the rise?". Nutrition Reviews. 68 (5): 257–69. doi:10.1111/j.1753-4887.2010.00286.x. PMID 20500787.
- Charles, RC; Ryan, ET (October 2011). "Cholera in the 21st century". Current Opinion in Infectious Diseases. 24 (5): 472–7. doi:10.1097/QCO.0b013e32834a88af. PMID 21799407. S2CID 6907842.
- Moudgal, V; Sobel, JD (February 2012). "Clostridium difficile colitis: a review". Hospital Practice. 40 (1): 139–48. doi:10.3810/hp.2012.02.954. PMID 22406889. S2CID 23015631.
- Lin, Z; Kotler, DP; Schlievert, PM; Sordillo, EM (May 2010). "Staphylococcal enterocolitis: forgotten but not gone?". Digestive Diseases and Sciences. 55 (5): 1200–7. doi:10.1007/s10620-009-0886-1. PMID 19609675. S2CID 2023416.
- "Persistent Travelers' Diarrhea". United States Centers for Disease Control and Prevention. 10 July 2015. Archived from the original on 3 January 2016. Retrieved 9 January 2016.
Although most cases of travelers' diarrhea are acute and self-limited, a certain percentage of travelers will develop persistent (>14 days) gastrointestinal symptoms ... Parasites as a group are the pathogens most likely to be isolated from patients with persistent diarrhea
- Leonard, J; Marshall, JK; Moayyedi, P (September 2007). "Systematic review of the risk of enteric infection in patients taking acid suppression". The American Journal of Gastroenterology. 102 (9): 2047–56, quiz 2057. doi:10.1111/j.1572-0241.2007.01275.x. PMID 17509031. S2CID 12326803.
- Escobedo, AA; Almirall, P; Robertson, LJ; Franco, RM; Hanevik, K; Mørch, K; Cimerman, S (October 2010). "Giardiasis: the ever-present threat of a neglected disease". Infectious Disorders Drug Targets. 10 (5): 329–48. doi:10.2174/187152610793180821. PMID 20701575.
- Grimwood, K; Forbes, DA (December 2009). "Acute and persistent diarrhea". Pediatric Clinics of North America. 56 (6): 1343–61. doi:10.1016/j.pcl.2009.09.004. PMID 19962025.
- Lawrence, DT; Dobmeier, SG; Bechtel, LK; Holstege, CP (May 2007). "Food poisoning". Emergency Medicine Clinics of North America. 25 (2): 357–73, abstract ix. doi:10.1016/j.emc.2007.02.014. PMID 17482025.
- Skiner HG, Blanchard J, Elixhauser A (September 2014). "Trends in Emergency Department Visits, 2006–2011". HCUP Statistical Brief #179. Rockville, MD: Agency for Healthcare Research and Quality. Archived from the original on 2014-12-24.
- Shane, Andi L; Mody, Rajal K; Crump, John A; Tarr, Phillip I; Steiner, Theodore S; Kotloff, Karen; Langley, Joanne M; Wanke, Christine; Warren, Cirle Alcantara; Cheng, Allen C; Cantey, Joseph; Pickering, Larry K (19 October 2017). "2017 Infectious Diseases Society of America Clinical Practice Guidelines for the Diagnosis and Management of Infectious Diarrhea". Clinical Infectious Diseases. 65 (12): e45–e80. doi:10.1093/cid/cix669. PMC 5850553. PMID 29053792.
- Steiner, MJ; DeWalt, DA; Byerley JS (9 June 2004). "Is this child dehydrated?". JAMA: The Journal of the American Medical Association. 291 (22): 2746–54. doi:10.1001/jama.291.22.2746. PMID 15187057.
- Freedman, SB; Vandermeer, B; Milne, A; Hartling, L; Pediatric Emergency Research Canada Gastroenteritis Study, Group (April 2015). "Diagnosing clinically significant dehydration in children with acute gastroenteritis using noninvasive methods: a meta-analysis". The Journal of Pediatrics. 166 (4): 908–916.e6. doi:10.1016/j.jpeds.2014.12.029. PMID 25641247.
- Warrell D.A.; Cox T.M.; Firth J.D.; Benz E.J., eds. (2003). The Oxford Textbook of Medicine (4th ed.). Oxford University Press. ISBN 978-0-19-262922-7. Archived from the original on 2012-03-21.
- "Viral Gastroenteritis". Center for Disease Control and Prevention. February 2011. Archived from the original on 24 April 2012. Retrieved 16 April 2012.
- World Health Organization (December 2009). "Rotavirus vaccines: an update" (PDF). Weekly Epidemiological Record. 84 (50): 533–540. PMID 20034143. Archived (PDF) from the original on 9 July 2012. Retrieved 10 May 2012.
- Giaquinto C, Dominiak-Felden G, Van Damme P, Myint TT, Maldonado YA, Spoulou V, Mast TC, Staat MA (July 2011). "Summary of effectiveness and impact of rotavirus vaccination with the oral pentavalent rotavirus vaccine: a systematic review of the experience in industrialized countries". Human Vaccines. 7 (7): 734–748. doi:10.4161/hv.7.7.15511. PMID 21734466. S2CID 23996836. Archived from the original on 17 February 2013. Retrieved 10 May 2012.
- Jiang, V; Jiang B; Tate J; Parashar UD; Patel MM (July 2010). "Performance of rotavirus vaccines in developed and developing countries". Human Vaccines. 6 (7): 532–542. doi:10.4161/hv.6.7.11278. PMC 3322519. PMID 20622508. Archived from the original on 17 February 2013. Retrieved 10 May 2012.
- Patel, MM; Steele, D; Gentsch, JR; Wecker, J; Glass, RI; Parashar, UD (January 2011). "Real-world impact of rotavirus vaccination". The Pediatric Infectious Disease Journal. 30 (1 Suppl): S1–5. doi:10.1097/INF.0b013e3181fefa1f. PMID 21183833. S2CID 1893099.
- US Center for Disease Control and Prevention (2008). "Delayed onset and diminished magnitude of rotavirus activity—United States, November 2007 – May 2008". Morbidity and Mortality Weekly Report. 57 (25): 697–700. PMID 18583958. Archived from the original on 8 June 2012. Retrieved 3 May 2012.
- Centers for Disease Control Prevention (CDC) (October 2009). "Reduction in rotavirus after vaccine introduction—United States, 2000–2009". Morbidity and Mortality Weekly Report. 58 (41): 1146–9. PMID 19847149. Archived from the original on 2009-10-31.
- Tate, JE; Cortese, MM; Payne, DC; Curns, AT; Yen, C; Esposito, DH; Cortes, JE; Lopman, BA; Patel, MM; Gentsch, JR; Parashar, UD (January 2011). "Uptake, impact, and effectiveness of rotavirus vaccination in the United States: review of the first 3 years of postlicensure data". The Pediatric Infectious Disease Journal. 30 (1 Suppl): S56–60. doi:10.1097/INF.0b013e3181fefdc0. PMID 21183842. S2CID 20940659.
- Sinclair, D; Abba, K; Zaman, K; Qadri, F; Graves, PM (16 March 2011). Sinclair, David (ed.). "Oral vaccines for preventing cholera". Cochrane Database of Systematic Reviews (3): CD008603. doi:10.1002/14651858.CD008603.pub2. PMC 6532691. PMID 21412922.
- World Health Organization. "Enterotoxigenic Escherichia coli (ETEC)". Diarrhoeal Diseases. Archived from the original on 15 May 2012. Retrieved 3 May 2012.
- World Health Organization. "Shigellosis". Diarrhoeal Diseases. Archived from the original on 15 December 2008. Retrieved 3 May 2012.
- Fedorowicz, Zbys; Jagannath, Vanitha A.; Carter, Ben (2011-09-07). "Antiemetics for reducing vomiting related to acute gastroenteritis in children and adolescents". Cochrane Database of Systematic Reviews. 130 (9): 270. doi:10.1002/14651858.CD005506.pub5. ISSN 1469-493X. PMC 6768985. PMID 21901699.
- Tytgat GN (2007). "Hyoscine butylbromide: a review of its use in the treatment of abdominal cramping and pain". Drugs. 67 (9): 1343–57. doi:10.2165/00003495-200767090-00007. PMID 17547475. S2CID 46971321.
- "BestBets: Fluid Treatment of Gastroenteritis in Adults". Archived from the original on 2009-02-12.
- Canavan A, Arant BS (October 2009). "Diagnosis and management of dehydration in children". American Family Physician. 80 (7): 692–6. PMID 19817339.
- Gregorio, GV; Gonzales, ML; Dans, LF; Martinez, EG (13 December 2016). "Polymer-based oral rehydration solution for treating acute watery diarrhoea". Cochrane Database of Systematic Reviews. 2016 (12): CD006519. doi:10.1002/14651858.CD006519.pub3. PMC 5450881. PMID 27959472.
- Toaimah, FH; Mohammad, HM (February 2016). "Rapid Intravenous Rehydration Therapy in Children With Acute Gastroenteritis: A Systematic Review". Pediatric Emergency Care. 32 (2): 131–5. doi:10.1097/pec.0000000000000708. PMID 26835574. S2CID 20509810.
- King CK, Glass R, Bresee JS, Duggan C (November 2003). "Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy". Morbidity and Mortality Weekly Report: Recommendations and Reports. 52 (RR-16): 1–16. PMID 14627948. Archived from the original on 2014-10-28.
- Collinson S , Deans A , Padua-Zamora A , Gregorio 3GV, Li 4C, Dans LF , Allen SJ (December 8, 2020). "Probiotics for treating acute infectious diarrhoea". Cochrane Database Syst Rev. 2020 (12): CD003048. doi:10.1002/14651858.CD003048.pub4. PMC 8166250. PMID 33295643.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Hempel, S; Newberry, SJ; Maher, AR; Wang, Z; Miles, JN; Shanman, R; Johnsen, B; Shekelle, PG (9 May 2012). "Probiotics for the prevention and treatment of antibiotic-associated diarrhea: a systematic review and meta-analysis". JAMA: The Journal of the American Medical Association. 307 (18): 1959–69. doi:10.1001/jama.2012.3507. PMID 22570464.
- Mackway-Jones, Kevin (June 2007). "Does yogurt decrease acute diarrhoeal symptoms in children with acute gastroenteritis?". BestBets. Archived from the original on 2009-02-12.
- Telmesani, AM (May 2010). "Oral rehydration salts, zinc supplement and rota virus vaccine in the management of childhood acute diarrhea". Journal of Family and Community Medicine. 17 (2): 79–82. doi:10.4103/1319-1683.71988. PMC 3045093. PMID 21359029.
- DeCamp LR, Byerley JS, Doshi N, Steiner MJ (September 2008). "Use of antiemetic agents in acute gastroenteritis: a systematic review and meta-analysis". Archives of Pediatrics & Adolescent Medicine. 162 (9): 858–65. doi:10.1001/archpedi.162.9.858. PMID 18762604.
- Mehta S, Goldman RD (2006). "Ondansetron for acute gastroenteritis in children". Canadian Family Physician. 52 (11): 1397–8. PMC 1783696. PMID 17279195.
- Fedorowicz, Z; Jagannath, VA; Carter, B (7 September 2011). Fedorowicz, Zbys (ed.). "Antiemetics for reducing vomiting related to acute gastroenteritis in children and adolescents". Cochrane Database of Systematic Reviews. 9 (9): CD005506. doi:10.1002/14651858.CD005506.pub5. PMC 6768985. PMID 21901699.
- Sturm JJ, Hirsh DA, Schweickert A, Massey R, Simon HK (May 2010). "Ondansetron use in the pediatric emergency department and effects on hospitalization and return rates: are we masking alternative diagnoses?". Annals of Emergency Medicine. 55 (5): 415–22. doi:10.1016/j.annemergmed.2009.11.011. PMID 20031265.
- "Ondansetron". Lexi-Comp. May 2011. Archived from the original on 2012-06-06.
- Traa BS, Walker CL, Munos M, Black RE (April 2010). "Antibiotics for the treatment of dysentery in children". International Journal of Epidemiology. 39 (Suppl 1): i70–4. doi:10.1093/ije/dyq024. PMC 2845863. PMID 20348130.
- Grimwood K, Forbes DA (December 2009). "Acute and persistent diarrhea". Pediatric Clinics of North America. 56 (6): 1343–61. doi:10.1016/j.pcl.2009.09.004. PMID 19962025.
- Mandell, Gerald L.; Bennett, John E.; Dolin, Raphael (2004). Mandell's Principles and Practices of Infection Diseases (6th ed.). Churchill Livingstone. ISBN 978-0-443-06643-6. Archived from the original on 2013-10-18. Retrieved 2006-04-22.
- Christopher, PR; David, KV; John, SM; Sankarapandian, V (4 August 2010). Christopher, Prince RH (ed.). "Antibiotic therapy for Shigella dysentery". Cochrane Database of Systematic Reviews (8): CD006784. doi:10.1002/14651858.CD006784.pub4. PMC 6532574. PMID 20687081.
- Effa, EE; Lassi, ZS; Critchley, JA; Garner, P; Sinclair, D; Olliaro, PL; Bhutta, ZA (5 October 2011). Bhutta, Zulfiqar A (ed.). "Fluoroquinolones for treating typhoid and paratyphoid fever (enteric fever)". Cochrane Database of Systematic Reviews (10): CD004530. doi:10.1002/14651858.CD004530.pub4. PMC 6532575. PMID 21975746.
- Gonzales, Maria Liza M.; Dans, Leonila F.; Sio-Aguilar, Juliet (9 January 2019). "Antiamoebic drugs for treating amoebic colitis". The Cochrane Database of Systematic Reviews. 1: CD006085. doi:10.1002/14651858.CD006085.pub3. ISSN 1469-493X. PMC 6326239. PMID 30624763.
- Harrison's Principles of Internal Medicine (16th ed.). McGraw-Hill. 2005. ISBN 978-0-07-140235-4. Archived from the original on 2012-08-04. Retrieved 2006-04-22.
- Feldman, Mark; Friedman, Lawrence S.; Sleisenger, Marvin H. (2002). Sleisenger & Fordtran's Gastrointestinal and Liver Disease (7th ed.). Saunders. ISBN 978-0-7216-8973-9.
- World Health Organization (November 2008). "Global networks for surveillance of rotavirus gastroenteritis, 2001–2008" (PDF). Weekly Epidemiological Record. 83 (47): 421–428. PMID 19024780. Archived (PDF) from the original on 9 July 2012. Retrieved 10 May 2012.
- Victora CG, Bryce J, Fontaine O, Monasch R (2000). "Reducing deaths from diarrhoea through oral rehydration therapy". Bulletin of the World Health Organization. 78 (10): 1246–55. PMC 2560623. PMID 11100619.
- Flahault, A; Hanslik, T (November 2010). "[Epidemiology of viral gastroenteritis in France and Europe]". Bulletin de l'Académie Nationale de Médecine. 194 (8): 1415–24, discussion 1424–5. doi:10.1016/S0001-4079(19)32172-7. PMID 22046706.
- Skolnik, Neil S.; Albert, Ross H., eds. (2008). Essential infectious disease topics for primary care. Totowa, NJ: Humana Press. p. 66. ISBN 978-1-58829-520-0. Archived from the original on 2015-11-28.
- "Gastroenteritis". Oxford English Dictionary 2011. Archived from the original on January 11, 2008. Retrieved January 15, 2012.
- Rudy's List of Archaic Medical Terms Archived 2007-07-09 at the Wayback Machine
- Charles E. Rosenberg (2009). The Cholera Years the United States in 1832, 1849, and 1866. Chicago: University of Chicago Press. p. 74. ISBN 978-0-226-72676-2. Archived from the original on 2015-11-09.
- Weese, JS (March 2011). "Bacterial enteritis in dogs and cats: diagnosis, therapy, and zoonotic potential". Veterinary Clinics of North America: Small Animal Practice. 41 (2): 287–309. doi:10.1016/j.cvsm.2010.12.005. PMID 21486637.
- Rousseaux, Wanda Haschek, Matthew Wallig, Colin (2009). Fundamentals of toxicologic pathology (2nd ed.). London: Academic. p. 182. ISBN 978-0-12-370469-6. Archived from the original on 2016-05-07.
- MacLachlan, N. James; Dubovi, Edward J., eds. (2009). Fenner's veterinary virology (4th ed.). Amsterdam: Elsevier Academic Press. p. 399. ISBN 978-0-12-375158-4. Archived from the original on 2015-11-25.
- Fox, James G.; et al., eds. (2002). Laboratory animal medicine (2nd ed.). Amsterdam: Academic Press. p. 649. ISBN 978-0-12-263951-7. Archived from the original on 2015-11-28.
- Zimmerman, Jeffrey; Karriker, Locke; Ramirez, Alejandro; Kent Schwartz; Gregory Stevenson (15 May 2012). Diseases of Swine (10th ed.). Chichester, West Sussex: John Wiley & Sons. p. 504. ISBN 978-0-8138-2267-9. Archived from the original on 28 November 2015.
Notes
- Dolin, Raphael; Mandell, Gerald L.; Bennett, John E., eds. (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases (7th ed.). Philadelphia: Churchill Livingstone/Elsevier. ISBN 978-0-443-06839-3.
External links
- Diarrhoea and Vomiting Caused by Gastroenteritis: Diagnosis, Assessment and Management in Children Younger than 5 Years – NICE Clinical Guidelines, No. 84.
- "Gastroenteritis". MedlinePlus. U.S. National Library of Medicine.