Tuberculosis in India
Tuberculosis in India is a major health problem, causing about 220,000 deaths every year. In 2020, the Indian government made statements to eliminate tuberculosis from the country by 2025 through its National TB Elimination Program. Interventions in this program include major investment in health care, providing supplemental nutrition credit through the Nikshay Poshan Yojana, organizing a national epidemiological survey for tuberculosis, and organizing a national campaign to tie together the Indian government and private health infrastructure for the goal of eliminating the disease.

India bears a disproportionately large burden of the world's tuberculosis rates, with World Health Organization (WHO) statistics for 2011 giving an estimated incidence figure of 2.2 million cases for India out of a global incidence of 9.6 million cases.[1]
Tuberculosis is one of India's biggest health issues, but what makes this problem even worse is the recent discovery of Totally Drug-Resistant Tuberculosis, TDR-TB. This issue of drug resistance began with MDR-TB, moved to XDR-TB and, as of 2021, has grown to embrace the most dangerous form, TDR-TB.[2][3]
The cost of this death and disease to the Indian economy between 2006 and 2014 was approximately US$1 billion.[4]
Epidemiology

Tuberculosis is one of India's major public health problems. According to World Health Organization (WHO) estimates, India has the world's largest tuberculosis epidemic.[5] In 2020, India accounted for 26% of the incident TB cases across the globe.India has incidence rate of 192 cases per 100,000 of population. India accounted for 38% of global TB deaths among HIV-negative people and for 34% of the combined total number of TB deaths in HIV-negative and HIV-positive people.Further in 2020, India accounted for 24% of global gap between estimated TB incidence and the number of people newly diagnosed with TB and reported.[6] Many research studies have investigated the effects and consequences of TDR-TB, especially in India, where social and economic development is still in progress. A report by Zarir Udwadia, originating from studies at the Hinduja Hospital in Mumbai, discusses the drug-resistant effects and results.[7] An experiment was conducted in January 2012 on four patients to test how resistant and unique the “new category” of TDR-TB is. These patients were given all the first-line drugs and second-line drugs that usually are prescribed to treat tuberculosis, and were resistant to all. As a response, the government of India appeared to stay in denial, while the WHO decided that although patterns of drug-resistance were evident, there was insufficient evidence to create a new category of TDR-TB from these results.[8]
Compared to India, Canada has about 1,600 new cases of TB every year.[9] Citing studies of TB-drug sales, the government of India now suggests the total has gone from being 2.2 million to 2.6 million people nationwide.[10] On March 24, 2019, TB Day, the Ministry of Health & Family Welfare of India notified that 2.15 million new tuberculosis patients were discovered only in 2018.[11]
In India, tuberculosis is responsible for the death of every third AIDS patient. Moreover, India accounts for about a quarter of the global tuberculosis burden.[11] The ministry reiterated their commitment to eliminating tuberculosis in the country by 2025.[11] As part of its efforts to eliminate tuberculosis, the Union Government changed the name of Revised National Tuberculosis Control Program (RNTCP) to National Tuberculosis Elimination Program (NTEP) on December 30, 2019.[12]
Cause and symptoms
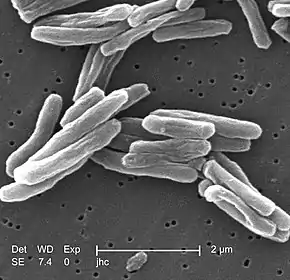
The bacterium that causes TB is called mycobacterium tuberculosis. A person can unknowingly acquire this bacteria and have it lie dormant within them, a condition known as inactive tuberculosis. Active tuberculosis begins when the bacteria starts developing, and the signs and symptoms begin to be visible. Although the TB bacteria can infect any organ (e.g., kidney, lymph nodes, bones, joints) in the body, the disease commonly occurs in the lungs.[9] Around 80% of all TB cases are related to pulmonary or lung.
Common symptoms include: coughing (that lasts longer than 3 weeks with green, yellow, or bloody sputum), weight loss, fatigue, fever, night sweats, chills, chest pain, shortness of breath, and loss of appetite.
Additional causes
Susceptibility to tuberculosis is heightened by a weak immune system. That is why babies, children, and senior adults have a higher risk of developing TB.[9] The bacterium spreads in the air sacs and passes into the lungs. Coughing, sneezing, and even talking to someone can release the mycobacterium into the air, and a person's chances of becoming infected are higher in countries where TB is common and where there is a big proportion of homeless people.[9] India, having the most TB cases of any country,[13] clearly falls into this category.
Socioeconomic Dimensions of TB
Local decreases in the incidence of tuberculosis in India correlate with improvements in social and economic determinants of health more than with access to quality treatment.[14] In India, pollution is widespread throughout the country. Pollution causes many effects in the air that people breathe, and since TB can be passed from person to person through the air, the chances of catching TB remain high in many parts of India.
Lack of infrastructure
Another major cause for the growth of TB in India has to do with its standing as a developing country. A study of Delhi slums has correlated higher scores on the Human Development Index and high proportions of one-room dwellings tend to correlate with TB at higher rates.[15] Poorly built environments, including hazards in the workplace, poor ventilation, and overcrowded homes have also been found to increase exposure to TB [14]
Lack of access to treatment
Another major reason for the high incidence of TB in India is because the majority of those infected are not able to afford the treatment drugs prescribed. “At present, only the 1.5 million patients already under the Indian government's care get free treatments for regular TB. That leaves patients who seek treatment in India's growing private sector to buy drugs for themselves, and most struggle to do that, government officials say.”[10] Although the latest phase of the state-run tuberculosis eradication program, the Revised National Tuberculosis Control Program (RNTCP), has focused on increasing access to TB care for poor people,[13] the majority of poor people still cannot access TB care financially.[16] “It is estimated that just 16% of patients with drug-resistant TB are receiving appropriate treatment”.[17] To combat this huge problem, India has begun a new program to try to provide free drugs to all those infected in the country.[10]
While RNTCP has created schemes to offer free or subsidized, high quality TB care, less than 1% of private practitioners have become fully involved.[16] This is exacerbated by a lack of education and background information which practitioners and professionals hold for prescribing drugs, or those private therapy sessions. A study conducted in Mumbai by Udwadia, Amale, Ajbani, and Rodrigues, showed that only 5 of 106 private practitioners practicing in a crowded area called Dharavi could prescribe a correct prescription for a hypothetical patient with MDR-TB.[18] Because the majority of TB cases are treated by private providers, and because the majority of poor people access informal (private) providers, the RNTCP's goals for universal access to TB care may have difficulty being met.[16]
Poor health
Poverty and a lack of financial resources are also associated with malnutrition, poor housing conditions, substance misuse, and HIV/AIDS incidence. These factors often contribute to a weakened immune system and are accordingly correlated with a higher susceptibility to TB.[14] They also tend to have a greater impact on people from high incidence countries such as India.[19] Indeed, addressing these factors may have a stronger correlation with decreased TB incidence than removing the financial burdens associated with care.[14] Yet, the RNTCP's treatment protocols do not address these social determinants of health.[14]
Treatment
Although tuberculosis is on the rise in India, treatment for it is also on the rise. To prevent spreading TB, it is important to get help quickly and to follow the treatment from your doctor through to completion. This can stop transmission of the bacteria and the appearance of antibiotic-resistant strains. Bacterial infections like tuberculosis require antibiotics for treatment and prevention, thus, commonly you will see that patients diagnosed with tuberculosis have certain pills and antibiotics carried around with them. The antibiotics most commonly used include isoniazid, rifampin, pyrazinamide, and ethambutol. It is crucial for a patient to take the medication that is prescribed by their doctor, and to continue taking it for the full course of the treatment (which may last for months or even years). This will help to ward off types of TB bacteria that are antibiotic-resistant, which take longer and are more difficult to treat.[9] In India, the majority of infections are of a type that is resistant to regular antibiotic treatment (MDR-TB, XDR-TB, TDR-TB), therefore, rather than one or two medications, a combination of different medications will be prescribed over a course of between 18 and 24 months, depending on how deep the infection is. Since the 1960s two drugs, isoniazid and rifampicin, have been the standard TB treatment.[17] In addition to antibiotics, a vaccine is available to limit the spread of bacteria after TB infection. This vaccine is generally used in countries or communities where the risk of TB infection is greater than 1% each year,[9] which includes parts of India.[17] In the past, treatment modalities in the public sector in India did have some drawbacks.[20] However, recently there has been a significant improvement in TB healthcare services in the public sector. The National TB Elimination Program (NTEP) in India has broadened its spectrum, in addition to providing free diagnostic and treatment services for drug sensistive as well as drug resistant forms of tuberculosis. The program is currently also targeting the TB Preventive therapy in vulnerable population with TB infection, who are at an increased risk of progressing to active TB disease.
70-80% of TB patients first visit the private sector, where the diagnostic and treatment services of TB are suboptimal and need to be improved.[21][22]
History
India's response to TB has changed with time and with the increasing sophistication of technology.[23] Responses to TB have evolved, from pre-independence through post-independence to the current WHO-assisted period.[23]
Following Independence, the Indian government established various regional and national TB reduction programmes.[23] The Indian government's Revised National TB Control Programme (RNTCP) started in India during 1997. The program used the WHO-recommended Directly Observed Treatment Short Course (DOTS) strategy to develop ideas and data on TB treatment. This group's initial objective was to achieve and maintain a TB treatment success rate of at least 85% in India among new patients.[24] “In 2010 the RNTCP made a major policy decision that it would change focus and adopt the concept of Universal Access to quality diagnosis and TB treatment for all TB patients”.[25] By doing so, they offered a helping hand to all people diagnosed with TB, by providing better quality services and improvement in therapy for these patients.
The contemporary response to TB includes India's participation and leadership in global TB reduction and elimination programs.[23] Treatment recommendations from Udwadia, et al. suggest that patients with TDR-TB only be treated “within the confines of government-sanctioned DOTS-Plus Programs to prevent the emergence of this untreatable form of tuberculosis”.[17] Given this conclusion by Udawadai, et al., it is considered certain, as of 2012, that the new Indian government program will insist on providing drugs free of charge to TB patients of India, for the first time ever.[10]
Society and culture
Organizations
The Tuberculosis Association of India is a voluntary organization that was set up in February 1939. It is affiliated to the government of India and is working with the TB Delhi center.[26]
Laboratories
The Revised National Tuberculosis Control Program (RNTCP) has established a network of laboratories where TB tests can be done for purposes of diagnosis and to determine whether a person has drug-resistant TB. The laboratory system comprises the National Reference Laboratories (NRLs), state level Intermediate Reference Laboratories (IRLs), Culture & Drug Susceptibility Testing (C & DST) laboratories and Designated Microscopy Centres (DMCs). Some private laboratories are also accredited as Culture & Drug Susceptibility Testing laboratories for tuberculosis (i.e. Microcare Laboratory & tuberculosis Research Centre, Surat)
Stigma
Disempowerment and stigma are often experienced by TB patients as they are disproportionately impoverished or socially marginalized.[27] The DOTS treatment regimen of the RNTCP is thought to deepen this sentiment,[28] as its close monitoring of patients can lead to stigma. To counteract disempowerment, some countries have engaged patients in the process of implementing the DOTS and in creating other treatment regimens that give more attention to their nonclinical needs. This knowledge can complement the clinical care provided by the DOTS.[29] Pro-poor strategies, including wage compensation for time lost to treatment, working with civil society organizations to link low income patients to social services, nutritional support, and offering local NGOs and committees a platform for engagement with the work done by private providers may reduce the burden of TB[30] and lead to greater patient autonomy.
Economics
Some legal advocates have argued that public interest litigation in India must be part of the TB response strategy to ensure that available resources actually fund the necessary health response.[31] India has a large burden of the world's TB, with an estimated economic cost of US$100 million lost annually due to this disease.[32]
Special populations
How Scheduled Tribes and other Adivasi are coping with TB highlights a lack of research and understanding of the health of this demographic.[33][34] There is a belief that this community is more vulnerable and has less access to treatment, but details are lacking on how TB affects tribal communities.[33][34]
References
- TB Statistics for India. (2012). TB Facts. Retrieved April 3, 2013, from http://www.tbfacts.org/tb-statistics-india.html
- Udwadia, Zarir; Vendoti, Deepesh (2013-06-01). "Totally drug-resistant tuberculosis (TDR-TB) in India: every dark cloud has a silver lining". J Epidemiol Community Health. 67 (6): 471–472. doi:10.1136/jech-2012-201640. ISSN 0143-005X. PMID 23155059. S2CID 42481569.
- Loewenberg, Samuel (2012-01-21). "India reports cases of totally drug-resistant tuberculosis". The Lancet. 379 (9812): 205. doi:10.1016/S0140-6736(12)60085-3. ISSN 0140-6736. PMID 22272391. S2CID 39443765.
- World Health Organization (2009). "Epidemiology". Global tuberculosis control: epidemiology, strategy, financing. pp. 6–33. ISBN 978-92-4-156380-2. Retrieved 14 June 2020.
- WHO. Global tuberculosis control. WHO report. WHO/HTM/TB/2006.362. Geneva: World Health Organization, 2006.
- Global Tuberculosis Report 2021. Geneva: World Health Organization. 2021. ISBN 978-92-4-003702-1. Retrieved 3 November 2021.
- Udwadia, Zarir; Vendoti, Deepesh (2013). "Totally drug-resistant tuberculosis (TDR-TB) in India: Every dark cloud has a silver lining". Journal of Epidemiology and Community Health. 67 (6): 471–472. doi:10.1136/jech-2012-201640. PMID 23155059. S2CID 42481569.
- Kanabus, Annabel. "Totally drug resistant TB - resistance to all known drugs". TBFACTS.ORG Information about Tuberculosis. Global Health Education, England. Retrieved 5 September 2021.
- Tuberculosis - Causes, Symptoms, Treatment, Diagnosis. (2013). C-Health. Retrieved April 3, 2103, from http://chealth.canoe.ca/channel_condition_info_details.asp?disease_id=231&channel_id=1020&relation_id=71085
- Anand, Geeta; McKay, Betsy (26 December 2012). "Awakening to Crisis, India Plans New Push Against TB". Wall Street Journal.
- "India records 2.15m new TB patients in 2018". The Nation. 2019-03-26. Retrieved 2019-03-27.
- AuthorTelanganaToday. "TB eradication mission renamed". Telangana Today. Retrieved 2020-01-02.
- Sachdeva, Kuldeep Singh et al. “New vision for Revised National Tuberculosis Control Programme (RNTCP): Universal access - "reaching the un-reached".” The Indian journal of medical research vol. 135,5 (2012): 690-4.
- Hargreaves, James R.; Boccia, Delia; Evans, Carlton A.; Adato, Michelle; Petticrew, Mark; Porter, John D. H. (April 2011). "The Social Determinants of Tuberculosis: From Evidence to Action". American Journal of Public Health. 101 (4): 654–662. doi:10.2105/AJPH.2010.199505. PMC 3052350. PMID 21330583.
- Chandra, Shivani; Sharma, Nandini; Joshi, Kulanand; Aggarwal, Nishi; Kannan, Anjur Tupil (17 January 2014). "Resurrecting social infrastructure as a determinant of urban tuberculosis control in Delhi, India". Health Research Policy and Systems. 12 (1): 3. doi:10.1186/1478-4505-12-3. PMC 3898563. PMID 24438431.
- Verma, Ramesh; Khanna, Pardeep; Mehta, Bharti (2013). "Revised National Tuberculosis Control Program in India: The Need to Strengthen". International Journal of Preventive Medicine. 4 (1): 1–5. PMC 3570899. PMID 23413398.
- Rowland, Katherine (2012). "Totally drug-resistant TB emerges in India". Nature. doi:10.1038/nature.2012.9797. S2CID 84692169.
- Udwadia, Z. F; Amale, R. A; Ajbani, K. K; Rodrigues, C (2011). "Totally Drug-Resistant Tuberculosis in India". Clinical Infectious Diseases. 54 (4): 579–581. doi:10.1093/cid/cir889. PMID 22190562.
- Dye, Christopher; Bourdin Trunz, Bernadette; Lönnroth, Knut; Roglic, Gojka; Williams, Brian G.; Gagneux, Sebastien (21 June 2011). "Nutrition, Diabetes and Tuberculosis in the Epidemiological Transition". PLOS ONE. 6 (6): e21161. Bibcode:2011PLoSO...621161D. doi:10.1371/journal.pone.0021161. PMC 3119681. PMID 21712992.
- Mishra, Gyanshankar; Ghorpade, S. V; Mulani, J (2014). "XDR-TB: An outcome of programmatic management of TB in India". Indian Journal of Medical Ethics. 11 (1): 47–52. doi:10.20529/IJME.2014.013. PMID 24509111.
- Mishra, Gyanshankar (2012). "Public-private mix in tuberculosis". The Lancet Infectious Diseases. 12 (12): 908–909. doi:10.1016/S1473-3099(12)70257-8. PMID 23174376. Retrieved 4 September 2021.
- Mishra, Gyanshankar; Mulani, Jasmin (2013). "Tuberculosis Prescription Practices In Private And Public Sector In India". National Journal of Integrated Research in Medicine. 4 (2): 71–78. doi:10.6084/m9.figshare.13271513. Retrieved 4 September 2021.
- Sandhu, GK (April 2011). "Tuberculosis: current situation, challenges and overview of its control programs in India". Journal of Global Infectious Diseases. 3 (2): 143–50. doi:10.4103/0974-777X.81691. PMC 3125027. PMID 21731301.
- http://www.scidev.net/tb/facts%5B%5D%5B%5D
- Coghaln, Andy (12 January 2012). "Totally drug-resistant TB at large in India". New Scientist.
- "Welcome to the Tuberculosis Association of India".
- Daftary, Amrita; Frick, Mike; Venkatesan, Nandita; Pai, Madhukar (31 October 2017). "Fighting TB stigma: we need to apply lessons learnt from HIV activism". BMJ Global Health. 2 (4): e000515. doi:10.1136/bmjgh-2017-000515. PMC 5717927. PMID 29225954.
- Achmat, Z (December 2006). "Science and social justice: the lessons of HIV/AIDS activism in the struggle to eradicate tuberculosis". The International Journal of Tuberculosis and Lung Disease. 10 (12): 1312–7. PMID 17167946.
- "Street Science: Characterizing Local Knowledge". Street Science. 2005. doi:10.7551/mitpress/6494.003.0004. ISBN 978-0-262-27080-9.
- Kamineni, Vishnu VARDHAN; Wilson, Nevin; Das, Anand; Satyanarayana, Srinath; Chadha, Sarabjit; Singh Sachdeva, Kuldeep; Singh Chauhan, Lakbir (2012). "Addressing poverty through disease control programmes: examples from Tuberculosis control in India". International Journal for Equity in Health. 11 (1): 17. doi:10.1186/1475-9276-11-17. PMC 3324374. PMID 22449205.
- McBroom, K (June 2016). "Litigation as TB Rights Advocacy: A New Delhi Case Study". Health and Human Rights. 18 (1): 69–84. PMC 5070681. PMID 27781000.
- Udwadia, Zarir F (2012). "MDR, XDR, TDR tuberculosis: Ominous progression". Thorax. 67 (4): 286–288. doi:10.1136/thoraxjnl-2012-201663. PMID 22427352.
- Rao, VG; Muniyandi, M; Bhat, J; Yadav, R; Sharma, R (January 2018). "Research on tuberculosis in tribal areas in India: A systematic review". The Indian Journal of Tuberculosis. 65 (1): 8–14. doi:10.1016/j.ijtb.2017.06.001. PMID 29332655.
- Thomas, BE; Adinarayanan, S; Manogaran, C; Swaminathan, S (May 2015). "Pulmonary tuberculosis among tribals in India: A systematic review & meta-analysis". The Indian Journal of Medical Research. 141 (5): 614–23. doi:10.4103/0971-5916.159545 (inactive 31 July 2022). PMC 4510760. PMID 26139779.
{{cite journal}}: CS1 maint: DOI inactive as of July 2022 (link)
Further consideration
- Central TB Division (March 2020). "India TB Report 2020". tbcindia.gov.in. Ministry of Health and Family Welfare.
- WHO Stop TB Department (2010). "A Brief History of Tuberculosis Control in India". World Health Organization.
External links
- Central Tuberculosis Division of the Government of India