Type 3c diabetes
Type 3c diabetes (also known as pancreatogenic diabetes) is diabetes that comes secondary to pancreatic diseases,[1] involving the exocrine and digestive functions of the pancreas.
| Type 3c diabetes | |
|---|---|
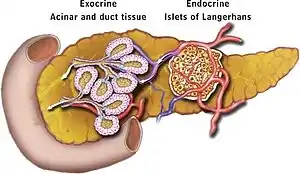 | |
| A model of the pancreas and its main locations for exocrine and endocrine functions. |
Around 5–10% of cases of diabetes in the Western world are related to pancreatic diseases. Chronic pancreatitis is most often the cause.[1][2]
Presentation
The same complications that occur for other types of diabetics (type 1 and type 2) may occur for type 3c diabetics. These include retinopathy, nephropathy, neuropathy, and cardiovascular disease. Patients with this condition are advised to follow the same risk-reduction guidelines as the other diabetics do and keep blood sugars as normal as possible to minimize any complications.
Cause
There are multiple causes. Some of which identified are:
- Pancreatic disease
- Pancreatic resection
- Chronic pancreatitis (caused by exocrine insufficiency, maldigestion, and malnutrition).[3]
- Lacking genes in the E2F group.[4]
- In 2021, Venturi reported that pancreas is able to absorb in great quantity radioactive cesium (Cs-134 and Cs-137) causing a severe and permanent pancreatitis with damage of pancreatic islands, and causing (type 3c) diabetes (pancreatogenic).[5] In fact, type 3c diabetes mellitus increased in contaminated population, particularly children and adolescents, after Fukushima and Chernobyl nuclear incidents. At the same time, worldwide pancreatic diseases, diabetes and environmental radiocesium are increasing.
Diagnosis
| Diagnostic Criteria for T3cDM |
|---|
| Major criteria (all must be fulfilled): |
|
| Minor Criteria: |
|
Management
The condition can be managed by many factors.
Lifestyle Modifications
Avoiding toxins to the body such as alcohol and smoking reduce pancreatic inflammation. Also, eating a diet rich in fiber and consuming normal amounts of fat may help. Oral pancreatic enzymes may be given. Maintaining sufficient levels of vitamin D can also reduce symptoms and help manage the disease better.
Medications
Medications such as insulin may be given in order to lower blood sugars. For not so high blood sugars, oral treatments in the form of a pill or capsule may be given.
Usually, insulin requirements are lower than in type 1 diabetes (SAID).[6] However, therapeutic challenges may arise from the fact that hypoglycaemia is a common complication, owing to the lack of alpha cells.[6]
See also
References
- Ewald, Nils; Hardt, Philip D (2013-11-14). "Diagnosis and treatment of diabetes mellitus in chronic pancreatitis". World Journal of Gastroenterology. 19 (42): 7276–7281. doi:10.3748/wjg.v19.i42.7276. ISSN 1007-9327. PMC 3831209. PMID 24259958.
- Hart, PA; Bellin, MD; Andersen, DK; Bradley, D; Cruz-Monserrate, Z; Forsmark, CE; Goodarzi, MO; Habtezion, A; Korc, M; Kudva, YC; Pandol, SJ; Yadav, D; Chari, ST; Consortium for the Study of Chronic Pancreatitis, Diabetes, and Pancreatic, Cancer(CPDPC). (November 2016). "Type 3c (pancreatogenic) diabetes mellitus secondary to chronic pancreatitis and pancreatic cancer". The Lancet. Gastroenterology & Hepatology. 1 (3): 226–237. doi:10.1016/S2468-1253(16)30106-6. PMC 5495015. PMID 28404095.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "Diabetes in Chronic Pancreatitis". Medscape. Anand R. Gupte and Chris E. Forsmark. Retrieved 2016-07-09.
- "Study shows molecular mechanism behind type 3c pancreatic diabetes". News Medical. August 29, 2012. Retrieved July 9, 2016.
- Venturi, Sebastiano (January 2021). "Cesium in Biology, Pancreatic Cancer, and Controversy in High and Low Radiation Exposure Damage—Scientific, Environmental, Geopolitical, and Economic Aspects". International Journal of Environmental Research and Public Health. 18 (17): 8934. doi:10.3390/ijerph18178934. PMC 8431133. PMID 34501532.
 Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License.
Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License. - Quast, Daniel Robert; Breuer, Thomas Georg Karl; Nauck, Michael Albrecht; Janot-Matuschek, Monika; Uhl, Waldemar; Meier, Juris Jendrik (April 2021). "Insulinbedarf und Glukosehomöostase bei Menschen nach partieller und totaler Pankreatektomie im Vergleich zu Menschen mit anderen Diabetesformen". Diabetologie und Stoffwechsel. 16 (2): 130–140. doi:10.1055/a-1344-0323. S2CID 233938736.