Trigeminal neuralgia
Trigeminal neuralgia (TN or TGN), also called Fothergill disease, tic douloureux, or trifacial neuralgia is a long-term pain disorder that affects the trigeminal nerve,[7][1] the nerve responsible for sensation in the face and motor functions such as biting and chewing. It is a form of neuropathic pain.[8] There are two main types: typical and atypical trigeminal neuralgia.[1] The typical form results in episodes of severe, sudden, shock-like pain in one side of the face that lasts for seconds to a few minutes.[1] Groups of these episodes can occur over a few hours.[1] The atypical form results in a constant burning pain that is less severe.[1] Episodes may be triggered by any touch to the face.[1] Both forms may occur in the same person.[1] It is regarded as one of the most painful disorders known to medicine, and often results in depression.[5]
| Trigeminal neuralgia | |
|---|---|
| Other names | Tic douloureux,[1] prosopalgia,[2] Fothergill's disease,[3] suicide disease[4] |
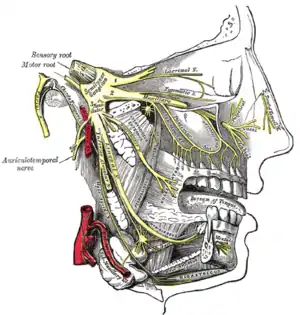 | |
| The trigeminal nerve and its three major divisions (shown in yellow): the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). | |
| Specialty | Neurology |
| Symptoms | Typical: episodes of severe, sudden, shock-like pain in one side of the face that lasts for seconds to minutes[1] Atypical: constant burning pain[1] |
| Complications | Depression[5] |
| Usual onset | > 50 years old[1] |
| Types | Typical and atypical trigeminal neuralgia[1] |
| Causes | Believed to be due to problems with myelin of trigeminal nerve[1][6] |
| Diagnostic method | Based on symptoms[1] |
| Differential diagnosis | Postherpetic neuralgia[1] |
| Treatment | Medication, surgery[1] |
| Medication | Carbamazepine, oxcarbazepine[6] |
| Prognosis | 80% improve with initial treatment[6] |
| Frequency | 1 in 8,000 people per year[1] |
The exact cause is unknown, but believed to involve loss of the myelin of the trigeminal nerve.[1][6] This might occur due to compression from a blood vessel as the nerve exits the brain stem, multiple sclerosis, stroke, or trauma.[1] Less common causes include a tumor or arteriovenous malformation.[1] It is a type of nerve pain.[1] Diagnosis is typically based on the symptoms, after ruling out other possible causes such as postherpetic neuralgia.[8][1]
Treatment includes medication or surgery.[1] The anticonvulsant carbamazepine or oxcarbazepine is usually the initial treatment, and is effective in about 90% of people.[8] Side effects are frequently experienced that necessitate drug withdrawal in as many as 23% of patients.[8] Other options include lamotrigine, baclofen, gabapentin, amitriptyline and pimozide.[6][1] Opioids are not usually effective in the typical form.[1] In those who do not improve or become resistant to other measures, a number of types of surgery may be tried.[6]
It is estimated that 1 in 8,000 people per year develop trigeminal neuralgia.[1] It usually begins in people over 50 years old, but can occur at any age.[1] Women are more commonly affected than men.[1] The condition was first described in detail in 1773 by John Fothergill.[9]
Signs and symptoms
This disorder is characterized by episodes of severe facial pain along the trigeminal nerve divisions. The trigeminal nerve is a paired cranial nerve that has three major branches: the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3). One, two, or all three branches of the nerve may be affected. Trigeminal neuralgia most commonly involves the middle branch (the maxillary nerve or V2) and lower branch (mandibular nerve or V3) of the trigeminal nerve.[10]
An individual attack usually lasts from a few seconds to several minutes or hours, but these can repeat for hours with very short intervals between attacks. In other instances, only 4–10 attacks are experienced daily. The episodes of intense pain may occur paroxysmally. To describe the pain sensation, people often describe a trigger area on the face so sensitive that touching or even air currents can trigger an episode; however, in many people, the pain is generated spontaneously without any apparent stimulation. It affects lifestyle as it can be triggered by common activities such as eating, talking, shaving and brushing teeth. The wind, chewing, and talking can aggravate the condition in many patients. The attacks are said, by those affected, to feel like stabbing electric shocks, burning, sharp, pressing, crushing, exploding or shooting pain that becomes intractable.[8]
The pain also tends to occur in cycles with remissions lasting months or even years. Pain attacks are known to worsen in frequency or severity over time, in some people. Pain may migrate to other branches over time but in some people remains very stable.[11]
Bilateral (occurring on both sides) trigeminal neuralgia is very rare except for trigeminal neuralgia caused by multiple sclerosis (MS). This normally indicates problems with both trigeminal nerves, since one nerve serves the left side of the face and the other serves the right side. Occasional reports of bilateral trigeminal neuralgia reflect successive episodes of unilateral (only one side) pain switching the side of the face rather than pain occurring simultaneously on both sides.[12]
Rapid spreading of the pain, bilateral involvement or simultaneous participation with other major nerve trunks (such as Painful Tic Convulsif of nerves V & VII or occurrence of symptoms in the V and IX nerves) may suggest a systemic cause. Systemic causes could include multiple sclerosis or expanding cranial tumors.[13]
The severity of the pain makes it difficult to wash the face, shave, and perform good oral hygiene. The pain has a significant impact on activities of daily living especially as those affected live in fear of when they are going to get their next attack of pain and how severe it will be. It can lead to severe depression and anxiety.[14]
However, not all people will have the symptoms described above; there are variants of TN, one of which is atypical trigeminal neuralgia ("trigeminal neuralgia, type 2" or trigeminal neuralgia with concomitant pain),[15] based on a recent classification of facial pain.[16] In these instances there is also a more prolonged lower severity background pain that can be present for over 50% of the time and is described more as a burning or prickling, rather than a shock.
Trigeminal pain can also occur after an attack of herpes zoster. Post-herpetic neuralgia has the same manifestations as in other parts of the body. Herpes zoster oticus typically presents with inability to move many facial muscles, pain in the ear, taste loss on the front of the tongue, dry eyes and mouth, and a vesicular rash. Less than 1% of varicella zoster infections involve the facial nerve and result in this occurring.[17]
Trigeminal deafferentation pain (TDP), also termed anesthesia dolorosa, or colloquially as phantom face pain, is from intentional damage to a trigeminal nerve following attempts to surgically fix a nerve problem. This pain is usually constant with a burning sensation and numbness. TDP is very difficult to treat as further surgeries are usually ineffective and possibly detrimental to the person.[18]
Causes
The trigeminal nerve is a mixed cranial nerve responsible for sensory data such as tactition (pressure), thermoception (temperature), and nociception (pain) originating from the face above the jawline; it is also responsible for the motor function of the muscles of mastication, the muscles involved in chewing but not facial expression.[19]
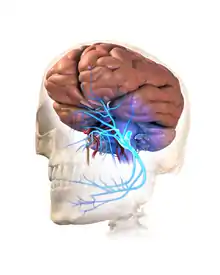
Several theories exist to explain the possible causes of this pain syndrome. It was once believed that the nerve was compressed in the opening from the inside to the outside of the skull; but leading research indicates that it is an enlarged or lengthened blood vessel – most commonly the superior cerebellar artery – compressing or throbbing against the microvasculature of the trigeminal nerve near its connection with the pons.[20] Such a compression can injure the nerve's protective myelin sheath and cause erratic and hyperactive functioning of the nerve. This can lead to pain attacks at the slightest stimulation of any area served by the nerve as well as hinder the nerve's ability to shut off the pain signals after the stimulation ends. This type of injury may rarely be caused by an aneurysm (an outpouching of a blood vessel); by an AVM (arteriovenous malformation);[21] by a tumor; such as an arachnoid cyst or meningioma in the cerebellopontine angle;[22] or by a traumatic event, such as a car accident.[23]
Short-term peripheral compression is often painless.[5] Persistent compression results in local demyelination with no loss of axon potential continuity. Chronic nerve entrapment results in demyelination primarily, with progressive axonal degeneration subsequently.[5] It is, "therefore widely accepted that trigeminal neuralgia is associated with demyelination of axons in the Gasserian ganglion, the dorsal root, or both."[24] It has been suggested that this compression may be related to an aberrant branch of the superior cerebellar artery that lies on the trigeminal nerve.[24] Further causes, besides an aneurysm, multiple sclerosis or cerebellopontine angle tumor, include: a posterior fossa tumor, any other expanding lesion or even brainstem diseases from strokes.[24]
Trigeminal neuralgia is found in 3–4% of people with multiple sclerosis, according to data from seven studies.[25][26] It has been theorized that this is due to damage to the spinal trigeminal complex.[27] Trigeminal pain has a similar presentation in patients with and without MS.[28]
Postherpetic neuralgia, which occurs after shingles, may cause similar symptoms if the trigeminal nerve is damaged, called Ramsay Hunt syndrome type 2.
When there is no apparent structural cause, the syndrome is called idiopathic.
Diagnosis
Trigeminal neuralgia is diagnosed via the result of neurological and physical tests, as well as the individual's medical history.[1]
Management
As with many conditions without clear physical or laboratory diagnosis, TN is sometimes misdiagnosed. A person with TN will sometimes seek the help of numerous clinicians before a firm diagnosis is made.
There is evidence that points towards the need to quickly treat and diagnose TN. It is thought that the longer a patient has TN, the harder it may be to reverse the neural pathways associated with the pain.
The differential diagnosis includes temporomandibular disorder.[29] Since triggering may be caused by movements of the tongue or facial muscles, TN must be differentiated from masticatory pain that has the clinical characteristics of deep somatic rather than neuropathic pain. Masticatory pain will not be arrested by a conventional mandibular local anesthetic block.[13] One quick test a dentist might perform is a conventional inferior dental local anaesthetic block, if the pain is in this branch, as it will not arrest masticatory pain but will TN.[30]
Medical
- The anticonvulsant carbamazepine is the first line treatment; second line medications include baclofen, lamotrigine, oxcarbazepine, phenytoin, topiramate, gabapentin and pregabalin. Uncontrolled trials have suggested that clonazepam and lidocaine may be effective.[31]
- Antidepressant medications, such as amitriptyline have shown good efficacy in treating trigeminal neuralgia, especially if combined with an anti-convulsant drug such as pregabalin.[32]
- There is some evidence that duloxetine can also be used in some cases of neuropathic pain, especially in patients with major depressive disorder[33] as it is an antidepressant. However, it should, by no means, be considered a first line therapy and should only be tried by specialist advice.[34]
- There is controversy around opiate use such as morphine and oxycodone for treatment of TN, with varying evidence on its effectiveness for neuropathic pain. Generally, opioids are considered ineffective against TN and thus should not be prescribed.[35]
Surgical
Microvascular decompression provides freedom from pain in about 75% of patients presenting with drug-resistant trigeminal neuralgia.[36][37][38] While there may be pain relief after surgery, there is also a risk of adverse effects, such as facial numbness. Percutaneous radiofrequency thermorhizotomy may also be effective[39] as may stereotactic radiosurgery; however the effectiveness decreases with time.[40]
Surgical procedures can be separated into non-destructive and destructive:
Non-destructive
- Microvascular decompression – this involves a small incision behind the ear and some bone removal from the area. An incision through the meninges is made to expose the nerve. Any vascular compressions of the nerve are carefully moved and a sponge-like pad is placed between the compression and nerve, stopping unwanted pulsation and allowing myelin sheath healing.
Destructive
All destructive procedures will cause facial numbness, post relief, as well as pain relief.[37]
- Percutaneous techniques which all involve a needle or catheter entering the face up to the origin where the nerve splits into three divisions and then damaging this area, purposely, to produce numbness but also stop pain signals. These techniques are proven effective[39] especially in those where other interventions have failed or in those who are medically unfit for surgery such as the elderly.
- Balloon compression – inflation of a balloon at this point causing damage and stopping pain signals.
- Glycerol injection – deposition of a corrosive liquid called glycerol at this point causes damage to the nerve to hinder pain signals.
- Radiofrequency thermocoagulation rhizotomy – application of a heated needle to damage the nerve at this point.
- Stereotactic radiosurgery is a form of radiation therapy that focuses high-power energy on a small area of the body[41]
Support
Psychological and social support has found to play a key role in the management of chronic illnesses and chronic pain conditions, such as trigeminal neuralgia. Chronic pain can cause constant frustration to an individual as well as to those around them.[42]
History
Trigeminal neuralgia was first described by physician John Fothergill and treated surgically by John Murray Carnochan, both of whom were graduates of the University of Edinburgh Medical School. Historically TN has been called "suicide disease" due to studies by the pioneering forefather in neurosurgery Harvey Cushing involving 123 cases of TN during 1896 and 1912. Often called the "suicide disease" because of the intense pain, higher rates of suicidal ideation in patients with severe migraines, and links to higher rates of depression, anxiety, and sleep disorders, trigeminal neuralgia is pain that spreads over the face and down the neck, triggered by even the slightest breath of wind across the face.[45][46][4][47]
Society and culture
Some individuals of note with TN include:
- Four-time British Prime Minister William Gladstone is believed to have had the disease.[48]
- Entrepreneur and author Melissa Seymour was diagnosed with TN in 2009 and underwent microvascular decompression surgery in a well documented case covered by magazines and newspapers which helped to raise public awareness of the illness in Australia. Seymour was subsequently made a Patron of the Trigeminal Neuralgia Association of Australia.[49]
- Salman Khan, an Indian film star, was diagnosed with TN in 2011. He underwent surgery in the US.[50]
- All-Ireland winning Gaelic footballer Christy Toye was diagnosed with the condition in 2013. He spent five months in his bedroom at home, returned for the 2014 season and lined out in another All-Ireland final with his team.[51]
- Jim Fitzpatrick – former Member of Parliament (MP) for Poplar and Limehouse – disclosed he had trigeminal neuralgia before undergoing neurosurgery. He has openly discussed his condition at parliamentary meetings and is a prominent figure in the TNA UK charity.[52]
- Jefferson Davis – President of the Confederate States of America[53]
- Charles Sanders Peirce – American philosopher, scientist and father of pragmatism.[54]
- Gloria Steinem – American feminist, journalist, and social and political activist[55]
- Anneli van Rooyen, Afrikaans singer-songwriter popular during the 1980s and 1990s, was diagnosed with atypical trigeminal neuralgia in 2004. During surgical therapy directed at alleviating the condition performed in 2007, Van Rooyen had permanent nerve damage, resulting in her near-complete retirement from performing.[56]
- H.R., singer of hardcore punk band Bad Brains[57]
- Aneeta Prem, British author, human rights campaigner, magistrate and the founder and president of Freedom Charity. Aneeta's experience of bilateral TN began in 2010, with severe pain and resulting sleep deprivation. Her condition remained undiagnosed until 2017. MVD Surgery to ameliorate the pain on the right-hand side was performed at UCHL in December 2019.[58]
- Travis Barker, drummer of rock band Blink-182[59]
See also
- Cluster headache
- Trigeminal trophic syndrome
References
- "Trigeminal Neuralgia Fact Sheet". NINDS. National Institutes of Health. 17 March 2020. Retrieved 5 April 2021.
- Hackley, CE (1869). A text-book of practical medicine. D. Appleton & Co. p. 292. Retrieved 2011-08-01.
prosopalgia.
- Bagheri, SC; et al. (December 1, 2004). "Diagnosis and treatment of patients with trigeminal neuralgia". Journal of the American Dental Association. 135 (12): 1713–7. doi:10.14219/jada.archive.2004.0124. PMID 15646605. Archived from the original on July 11, 2012. Retrieved 2011-08-01.
- Adams, H; Pendleton, C; Latimer, K; Cohen-Gadol, AA; Carson, BS; Quinones-Hinojosa, A (May 2011). "Harvey Cushing's case series of trigeminal neuralgia at the Johns Hopkins Hospital: a surgeon's quest to advance the treatment of the 'suicide disease'". Acta Neurochirurgica. 153 (5): 1043–50. doi:10.1007/s00701-011-0975-8. PMID 21409517. S2CID 28245294.
- Okeson, JP (2005). "6". In Lindsay Harmon (ed.). Bell's orofacial pains: the clinical management of orofacial pain. Quintessence Publishing Co, Inc. p. 114. ISBN 0-86715-439-X. Archived from the original on 2014-01-12.
- Obermann, Mark (2010-03-01). "Treatment options in trigeminal neuralgia". Therapeutic Advances in Neurological Disorders. 3 (2): 107–115. doi:10.1177/1756285609359317. ISSN 1756-2856. PMC 3002644. PMID 21179603.
- "Trigeminal Neuralgia".
- Cruccu, Giorgio; Di Stefano, Giulia; Truini, Andrea (2020-08-20). Ropper, Allan H. (ed.). "Trigeminal Neuralgia". New England Journal of Medicine. 383 (8): 754–762. doi:10.1056/NEJMra1914484. ISSN 0028-4793. PMID 32813951. S2CID 221201036.
- Prasad, S; Galetta, S (March 2009). "Trigeminal neuralgia: historical notes and current concepts". The Neurologist. 15 (2): 87–94. doi:10.1097/nrl.0b013e3181775ac3. PMID 19276786. S2CID 23500191.
- "Trigeminal Neuralgia and Hemifacial Spasm" (PDF). UF Health Shands Hospital. November 2012. Retrieved 5 April 2021.
- Bayer DB, Stenger TG (1979). "Trigeminal neuralgia: an overview". Oral Surg Oral Med Oral Pathol. 48 (5): 393–9. doi:10.1016/0030-4220(79)90064-1. PMID 226915.
- Cruccu, Giorgio; Finnerup, Nanna B.; Jensen, Troels S.; Scholz, Joachim; Sindou, Marc; Svensson, Peter; Treede, Rolf-Detlef; Zakrzewska, Joanna M.; Nurmikko, Turo (2016). "Trigeminal neuralgia". Neurology. 87 (2): 220–228. doi:10.1212/WNL.0000000000002840. PMC 4940067. PMID 27306631.
- Okeson, JP (2005). "17". In Lindsay Harmon (ed.). Bell's orofacial pains: the clinical management of orofacial pain. Quintessence Publishing Co, Inc. p. 453. ISBN 0-86715-439-X. Archived from the original on 2014-01-12.
- Smith, Jared G.; Elias, Leigh-Ann; Yilmaz, Zehra; Barker, Sarah; Shah, Kunal; Shah, Sajni; Renton, Tara (2013). "The Psychosocial and Affective Burden of Posttraumatic Stress Neuropathy Following Injuries to the Trigeminal Nerve". Journal of Orofacial Pain. 27 (4): 293–303. doi:10.11607/jop.1056. ISSN 1064-6655. PMID 24171179.
- "Neurological surgery: facial pain". Oregon Health & Science University. Archived from the original on 2004-08-12. Retrieved 2011-08-01.
- Burchiel KJ (2003). "A new classification for facial pain". Neurosurgery. 53 (5): 1164–7. doi:10.1227/01.NEU.0000088806.11659.D8. PMID 14580284. S2CID 33538452.
- Feller, L.; Khammissa, R. A.; Fourie, J.; Bouckaert, M.; Lemmer, J. (2017). "Postherpetic Neuralgia and Trigeminal Neuralgia". Pain Research and Treatment. 2017: 1–6. doi:10.1155/2017/1681765. PMC 5735631. PMID 29359044.
- "Anesthesia Dolorosa". 14 April 2021.
- Pazhaniappan, Nandhaa (15 August 2020). "The Trigeminal Nerve (CN V)". TeachMeAnatomy. Retrieved 5 April 2021.
- Nurmikko, T. J.; Eldridge, P. R (2009). "Trigeminal neuralgia—pathophysiology, diagnosis and current treatment". Pain. 87: 165–166. doi:10.1093/bja/87.1.117. PMID 11460800.
- Singh, Navneet; Bharatha, Aditya; O'Kelly, Cian; Wallace, M. Christopher; Goldstein, Warren; Willinsky, Robert A.; Aviv, Richard I.; Symons, Sean P. (2014). "Intrinsic Arteriovenous Malformation of the Trigeminal Nerve". Canadian Journal of Neurological Sciences. 37 (5): 681–683. doi:10.1017/S0317167100010891. ISSN 0317-1671.
- Babu R, Murali R (1991). "Arachnoid cyst of the cerebellopontine angle manifesting as contralateral trigeminal neuralgia: case report". Neurosurgery. 28 (6): 886–7. doi:10.1097/00006123-199106000-00018. PMID 2067614.
- Croft, Stephen M. Foreman, Arthur C. (2002). Whiplash injuries : the cervical acceleration/deceleration syndrome (3rd ed.). Baltimore: Williams & Wilkins. p. 481. ISBN 9780781726818. Archived from the original on 2017-03-14.
- Okeson, JP (2005). "6". In Lindsay Harmon (ed.). Bell's orofacial pains: the clinical management of orofacial pain. Quintessence Publishing Co, Inc. p. 115. ISBN 0-86715-439-X. Archived from the original on 2014-01-12.
- Foley P, Vesterinen H, Laird B, et al. (2013). "Prevalence and natural history of pain in adults with multiple sclerosis: Systematic review and meta-analysis". Pain. 154 (5): 632–42. doi:10.1016/j.pain.2012.12.002. PMID 23318126. S2CID 25807525.
- De Santi, L; Annunziata, P (February 2012). "Symptomatic cranial neuralgias in multiple sclerosis: Clinical features and treatment". Clinical Neurology and Neurosurgery. 114 (2): 101–7. doi:10.1016/j.clineuro.2011.10.044. PMID 22130044. S2CID 3402581.
- Cruccu G, Biasiotta A, Di Rezze S, et al. (2009). "Trigeminal neuralgia and pain related to multiple sclerosis". Pain. 143 (3): 186–91. doi:10.1016/j.pain.2008.12.026. PMID 19171430. S2CID 24353039.
- De Simone, R.; Marano, E.; Brescia Morra, V.; Ranieri, A.; Ripa, P.; Esposito, M.; Vacca, G.; Bonavita, V. (2005). "A clinical comparison of trigeminal neuralgic pain in patients with and without underlying multiple sclerosis". Neurological Sciences. 26 (S2): s150–s151. doi:10.1007/s10072-005-0431-8. ISSN 1590-1874. PMID 15926016. S2CID 23024675.
- Drangsholt, M; Truelove, EL (2001). "Trigeminal neuralgia mistaken as temporomandibular disorder". J Evid Base Dent Pract. 1 (1): 41–50. doi:10.1067/med.2001.116846.
- Cherian, Anusha. "Dr". MedScape. Archived from the original on 26 October 2015. Retrieved 20 November 2015.
- Sindrup, SH; Jensen, TS (2002). "Pharmacotherapy of trigeminal neuralgia". Clin J Pain. 18 (1): 22–7. doi:10.1097/00002508-200201000-00004. PMID 11803299. S2CID 24407923.
- Lawal, Ahmed; et al. (September 2012). "Management of Trigeminal Neuralgia using Amitriptyline and Pregablin combination Therapy". African Journal of Biomedical Research. 15 (1): 201–203. Archived from the original on 2016-08-22.
- Hsu, CC; et al. (Apr 2014). "Rapid Management of Trigeminal Neuralgia and Comorbid Major Depressive Disorder With Duloxetine". Annals of Pharmacotherapy. 48 (8): 1090–1092. doi:10.1177/1060028014532789. PMID 24788987. S2CID 38592913.
- Lunn, Michael P. T.; Hughes, Richard A. C.; Wiffen, Philip J. (2014-01-03). "Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia". The Cochrane Database of Systematic Reviews (1): CD007115. doi:10.1002/14651858.CD007115.pub3. ISSN 1469-493X. PMID 24385423.
- Zakrzewska, J. M.; Linskey, M. E. (17 February 2014). "Trigeminal neuralgia" (PDF). BMJ. 348 (feb17 9): g474. doi:10.1136/bmj.g474. PMID 24534115. S2CID 45305211. Archived (PDF) from the original on 20 December 2016.
- Holste K, Chan AY, Rolston JD, Englot DJ (February 2020). "Pain Outcomes Following Microvascular Decompression for Drug-Resistant Trigeminal Neuralgia: A Systematic Review and Meta-Analysis". Neurosurgery. 86 (2): 182–190. doi:10.1093/neuros/nyz075. PMC 8253302. PMID 30892607.
- Zakrzewska, JM; Akram, H (Sep 7, 2011). "Neurosurgical interventions for the treatment of classical trigeminal neuralgia". Cochrane Database of Systematic Reviews. 9 (9): CD007312. doi:10.1002/14651858.CD007312.pub2. PMC 8981212. PMID 21901707.
- 2015 review of treatment of TN Archived 2015-11-10 at the Wayback Machine
- Sindou, M; Tatli, M (April 2009). "[Treatment of trigeminal neuralgia with thermorhizotomy]". Neuro-Chirurgie. 55 (2): 203–10. doi:10.1016/j.neuchi.2009.01.015. PMID 19303114.
- Dhople, AA; Adams, JR; Maggio, WW; Naqvi, SA; Regine, WF; Kwok, Y (August 2009). "Long-term outcomes of Gamma Knife radiosurgery for classic trigeminal neuralgia: implications of treatment and critical review of the literature. Clinical article". Journal of Neurosurgery. 111 (2): 351–8. doi:10.3171/2009.2.JNS08977. PMID 19326987.
- Yi-Bin, Chen. "Stereotactic radiosurgery – Cyber Knife". MedLine Plus. Archived from the original on 21 November 2015. Retrieved 20 November 2015.
- Molitor, Nancy. "Dr". American Psychological Association. APA. Archived from the original on 26 June 2015. Retrieved 27 June 2015.
- Williams, Christopher; Dellon, A.; Rosson, Gedge (5 March 2009). "Management of Chronic Facial Pain". Craniomaxillofacial Trauma and Reconstruction. 2 (2): 067–076. doi:10.1055/s-0029-1202593. PMC 3052669. PMID 22110799.
- "Facial Neuralgia Resources". Trigeminal Neuralgia Resources / Facial Neuralgia Resources. Archived from the original on 8 July 2013. Retrieved 8 May 2013.
- Adams, H.; Pendleton, C.; Latimer, K.; Cohen-Gadol, A. A.; Carson, B. S.; Quinones-Hinojosa, A. (2011). "Harvey Cushing's case series of trigeminal neuralgia at the Johns Hopkins Hospital: A surgeon's quest to advance the treatment of the 'suicide disease'". Acta Neurochirurgica. 153 (5): 1043–1050. doi:10.1007/s00701-011-0975-8. PMID 21409517. S2CID 28245294.
- "Why Trigeminal Neuralgia is Considered the "Suicide Disease" | Arizona Pain". 26 September 2021.
- Prasad, S; Galetta, S (2009). "Trigeminal Neuralgia Historical Notes and Current Concept". Neurologist. 15 (2): 87–94. doi:10.1097/NRL.0b013e3181775ac3. PMID 19276786. S2CID 23500191.
- Sack, James J. (December 2014). "William Gladstone: New Studies and Perspectives. Edited by Roland Quinault, Roger Swift, and Ruth Clayton Windscheffel.Farnham: Ashgate, 2012. Pp. xviii+350. $134.95". The Journal of Modern History. 86 (4): 904–905. doi:10.1086/678722.
- "Melissa Seymour: My perfect life is over". Womansday.ninemsn.com.au. 2009-06-18. Archived from the original on 2009-12-14. Retrieved 2013-10-09.
- "Salman suffering from the suicide disease". www.hindustantimes.com. Hindustan Times. 2011-08-24. Archived from the original on 2014-07-15. Retrieved 2014-06-18.
- Foley, Alan (16 September 2014). "Serious illness meant Christy Toye didn't play in 2013 but now he's set for All-Ireland final: The Donegal player has experienced a remarkable revival". The Score. Archived from the original on 4 October 2014. Retrieved 16 September 2014.
- "MP urges greater awareness of trigeminal neuralgia". BBC – Democracy Live. BBC. 2010-07-27. Archived from the original on 21 November 2015. Retrieved 20 November 2015.
- "U.S. Senate: Jefferson Davis' Farewell". Archived from the original on 2011-03-01. Retrieved 2011-06-09.
- Joseph Brent, Charles Sanders Peirce: A Life, Bloomington: Indiana University Press, 1993, p. 39–40
- Gorney, Cynthia (November–December 1995). "Gloria". Mother Jones. Archived from the original on July 29, 2016. Retrieved July 1, 2016.
- "Anneli van Rooyen's road to recovery". 2011-08-26. Archived from the original on 2017-03-05. Retrieved 2016-09-12.
- Music, Guardian (2017-02-03). "Hardcore legend HR of Bad Brains to undergo brain surgery". The Guardian. Archived from the original on 2017-03-02. Retrieved 2017-03-02.
- "The latest news from TNA UK". 2020-06-01. Retrieved 2020-09-23.
- "Blink 182 Drummer Travis Barker Uses CBD to Treat Rare Condition: "I Love CBD"". vaporvanity. February 5, 2019. Retrieved 2021-02-11.
