Amitriptyline
Amitriptyline, sold under the brand name Elavil among others, is a tricyclic antidepressant primarily used to treat cyclic vomiting syndrome (CVS), major depressive disorder and a variety of pain syndromes from neuropathic pain to fibromyalgia to migraine and tension headaches.[10] Due to the frequency and prominence of side effects, amitriptyline is generally considered a second-line therapy for these indications.[11][12][13][14]
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌæmɪˈtrɪptɪliːn/[1] |
| Trade names | Elavil, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682388 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, intramuscular injection |
| Drug class | Tricyclic antidepressant (TCA) |
| ATC code |
|
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 45%[3]-53%[4] |
| Protein binding | 96%[5] |
| Metabolism | Liver (CYP2D6, CYP2C19, CYP3A4)[6][4][7] |
| Metabolites | nortriptyline, (E)-10-hydroxynortriptyline |
| Elimination half-life | 21 hours[3] |
| Excretion | Urine: 12-80% after 48 hours;[8] feces: not studied |
| Identifiers | |
IUPAC name
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.038 |
| Chemical and physical data | |
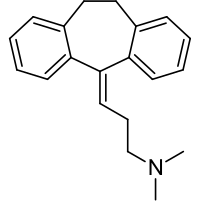
| Formula | C20H23N |
| Molar mass | 277.411 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 197.5 °C (387.5 °F) [9] |
| |
| |
| (verify) | |
The most common side effects are dry mouth, drowsiness, dizziness, constipation, and weight gain. Of note is sexual dysfunction, observed primarily in males. Glaucoma, liver toxicity and abnormal heart rhythms are rare but serious side effects. Blood levels of amitriptyline vary significantly from one person to another,[15] and amitriptyline interacts with many other medications potentially aggravating its side effects.
Amitriptyline was discovered in the late 1950s by scientists at Merck and approved by the US Food and Drug Administration (FDA) in 1961.[16] It is on the World Health Organization's List of Essential Medicines.[17] It is available as a generic medication.[18] In 2020, it was the 81st most commonly prescribed medication in the United States, with more than 9 million prescriptions.[19][20]
Medical uses
Amitriptyline is indicated for the treatment of major depressive disorder and neuropathic pain and for the prevention of migraine and chronic tension headache. It can be used for the treatment of nocturnal enuresis in children older than 6 after other treatments have failed.[10]
Depression
Amitriptyline is effective for depression,[21] but it is rarely used as a first-line antidepressant due to its higher toxicity in overdose and generally poorer tolerability.[22] It can be tried for depression as a second-line therapy, after the failure of other treatments.[11] For treatment-resistant adolescent depression[23] or for cancer-related depression[24] amitriptyline is no better than placebo. It is sometimes used for the treatment of depression in Parkinson's disease,[25] but supporting evidence for that is lacking.[26]
Pain
Amitriptyline alleviates painful diabetic neuropathy. It is recommended by a variety of guidelines as a first or second line treatment.[12] It is as effective for this indication as gabapentin or pregabalin but less well tolerated.[27]
Low doses of amitriptyline moderately improve sleep disturbances and reduce pain and fatigue associated with fibromyalgia.[28] It is recommended for fibromyalgia accompanied by depression by Association of the Scientific Medical Societies in Germany[28] and as a second-line option for fibromyalgia, with exercise being the first line option, by European League Against Rheumatism.[13] Combinations of amitriptyline and fluoxetine or melatonin may reduce fibromyalgia pain better than either medication alone.[29]
There is some (low-quality) evidence that amitriptyline may reduce pain in cancer patients. It is recommended only as a second line therapy for non-chemotherapy-induced neuropathic or mixed neuropathic pain, if opioids did not provide the desired effect.[30]
Moderate evidence exists in favor of amitriptyline use for atypical facial pain.[31] Amitriptyline is ineffective for HIV-associated neuropathy.[27]
Headache
Amitriptyline is probably effective for the prevention of periodic migraine in adults. Amitriptyline is similar in efficacy to venlafaxine and topiramate but carries a higher burden of adverse effects than topiramate.[14] For many patients, even very small doses of amitriptyline are helpful, which may allow for minimization of side effects.[32] Amitriptyline is not significantly different from placebo when used for the prevention of migraine in children.[33]
Amitriptyline may reduce the frequency and duration of chronic tension headache, but it is associated with worse adverse effects than mirtazapine. Overall, amitriptyline is recommended for tension headache prophylaxis, along with lifestyle advice, which should include avoidance of analgesia and caffeine.[34]
Other indications
Amitriptyline is effective for the treatment of irritable bowel syndrome; however, because of its side effects, it should be reserved for select patients for whom other agents do not work.[35] There is insufficient evidence to support its use for abdominal pain in children with functional gastrointestinal disorders.[36]
Tricyclic antidepressants decrease the frequency, severity, and duration of cyclic vomiting syndrome episodes. Amitriptyline, as the most commonly used of them, is recommended as a first-line agent for its therapy.[37]
Amitriptyline may improve pain and urgency intensity associated with bladder pain syndrome and can be used in the management of this syndrome.[38][39] Amitriptyline can be used in the treatment of nocturnal enuresis in children. However, its effect is not sustained after the treatment ends. Alarm therapy gives better short- and long-term results.[40]
In the US, amitriptyline is commonly used in children with ADHD as an adjunct to stimulant medications without any evidence or guideline supporting this practice.[41] Many physicians in the UK (and the US also) commonly prescribe amitriptyline for insomnia;[42] however, Cochrane reviewers were not able to find any randomized controlled studies that would support or refute this practice.[43]
Contraindications and precautions
The known contraindications of amitriptyline are:[10]
- History of myocardial infarction
- History of arrhythmias, particularly any degree of heart block
- Coronary artery disease
- Porphyria
- Severe liver disease (such as cirrhosis)
- Being under six years of age
- Patients who are taking monoamine oxidase inhibitors (MAOIs) or have taken them within the last 14 days
Amitriptyline should be used with caution in patients with epilepsy, impaired liver function, pheochromocytoma, urinary retention, prostate enlargement, hyperthyroidism, and pyloric stenosis.[10]
In patients with the rare condition of shallow anterior chamber of eyeball and narrow anterior chamber angle, amitriptyline may provoke attacks of acute glaucoma due to dilation of the pupil. It may aggravate psychosis, if used for depression with schizophrenia, or precipitate the switch to mania in those with bipolar disorder.[10]
CYP2D6 poor metabolizers should avoid amitriptyline due to increased side effects. If it is necessary to use it, half dose is recommended.[44] Amitriptyline can be used during pregnancy and lactation, in the cases when SSRI do not work.[45]
Side effects
The most frequent side effects, occurring in 20% or more of users, are dry mouth, drowsiness, dizziness, constipation, and weight gain (on average 1.8 kg[46]).[21] Other common side effects (in 10% or more) are vision problems (amblyopia, blurred vision), tachycardia, increased appetite, tremor, fatigue/asthenia/feeling slowed down, and dyspepsia.[21]
A literature review about abnormal movements and amitriptyline found that this drug is associated with various movement disorders, particularly dyskinesia, dystonia, and myoclonus. Stuttering and restless legs syndrome are some of the less common associations.[47]
A less common side effect of amitriptyline is urination problems (8.7%).[48]
Amitriptyline-associated sexual dysfunction (occurring at a frequency of 6.9%) seems to be mostly confined to males with depression and is expressed predominantly as erectile dysfunction and low libido disorder, with lesser frequency of ejaculatory and orgasmic problems. The rate of sexual dysfunction in males treated for indications other than depression and in females is not significantly different from placebo.[49]
Liver tests abnormalities occur in 10-12% of patients on amitriptyline, but are usually mild, asymptomatic and transient,[50] with consistently elevated alanine transaminase in 3% of all patients.[51][52] The increases of the enzymes above the 3-fold threshold of liver toxicity are uncommon, and cases of clinically apparent liver toxicity are rare;[50] nevertheless, amitriptyline is placed in the group of antidepressants with greater risks of hepatic toxicity.[51]
Amitriptyline prolongs the QT interval.[53] This prolongation is relatively small at therapeutic doses[54] but becomes severe in overdose.[55]
Overdose
The symptoms and the treatment of an overdose are largely the same as for the other TCAs, including the presentation of serotonin syndrome and adverse cardiac effects. The British National Formulary notes that amitriptyline can be particularly dangerous in overdose,[56] thus it and other TCAs are no longer recommended as first-line therapy for depression. The treatment of overdose is mostly supportive as no specific antidote for amitriptyline overdose is available. Activated charcoal may reduce absorption if given within 1–2 hours of ingestion. If the affected person is unconscious or has an impaired gag reflex, a nasogastric tube may be used to deliver the activated charcoal into the stomach. ECG monitoring for cardiac conduction abnormalities is essential and if one is found close monitoring of cardiac function is advised. Body temperature should be regulated with measures such as heating blankets if necessary. Cardiac monitoring is advised for at least five days after the overdose. Benzodiazepines are recommended to control seizures. Dialysis is of no use due to the high degree of protein binding with amitriptyline.[5]
Interactions
Since amitriptyline and its active metabolite nortriptyline are primarily metabolized by cytochromes CYP2D6 and CYP2C19 (see Amitriptyline#Pharmacology), the inhibitors of these enzymes are expected to exhibit pharmacokinetic interactions with amitriptyline. According to the prescribing information, the interaction with CYP2D6 inhibitors may increase the plasma level of amitriptyline.[10] However, the results in the other literature are inconsistent:[6] the co-administration of amitriptyline with a potent CYP2D6 inhibitor paroxetine does increase the plasma levels of amitriptyline two-fold and of the main active metabolite nortriptyline 1.5-fold,[57] but combination with less potent CYP2D6 inhibitors thioridazine or levomepromazine does not affect the levels of amitriptyline and increases nortriptyline by about 1.5-fold;[58] a moderate CYP2D6 inhibitor fluoxetine does not seem to have a significant effect on the levels of amitriptyline or nortriptyline.[59][60] A case of clinically significant interaction with potent CYP2D6 inhibitor terbinafine has been reported.[61]
A potent inhibitor of CYP2C19 and other cytochromes fluvoxamine increases the level of amitriptyline two-fold while slightly decreasing the level of nortriptyline.[59] Similar changes occur with a moderate inhibitor of CYP2C19 and other cytochromes cimetidine: amitriptyline level increases by about 70%, while nortriptyline decreases by 50%.[62] CYP3A4 inhibitor ketoconazole elevates amitriptyline level by about a quarter.[7] On the other hand, cytochrome P450 inducers such as carbamazepine and St. John's Wort decrease the levels of both amitriptyline and nortriptyline[58][63]
Oral contraceptives may increase the blood level of amitriptyline by as high as 90%.[64] Valproate moderately increases the levels of amitriptyline and nortriptyline through an unclear mechanism.[65]
The prescribing information warns that the combination of amitriptyline with monoamine oxidase inhibitors may cause potentially lethal serotonin syndrome;[10] however, this has been disputed.[66] The prescribing information cautions that some patients may experience a large increase in amitriptyline concentration in the presence of topiramate.[67] However, other literature states that there is little or no interaction: in a pharmacokinetic study topiramate only increased the level of amitriptyline by 20% and nortriptyline by 33%.[68]
Amitriptiline counteracts the antihypertensive action of guanethidine.[5][69] When given with amitriptyline, other anticholinergic agents may result in hyperpyrexia or paralytic ileus.[67] Co-administration of amitriptyline and disulfiram is not recommended due to the potential for the development of toxic delirium.[5][70] Amitriptyline causes an unusual type of interaction with the anticoagulant phenprocoumon during which great fluctuations of the prothrombin time have been observed.[71]
Pharmacology
Pharmacodynamics
| Site | AMI | NTI | Species | Ref |
|---|---|---|---|---|
| SERT | 2.8–36 | 15–279 | Human | [73][74] |
| NET | 19–102 | 1.8–21 | Human | [73][74] |
| DAT | 3,250 | 1,140 | Human | [73] |
| 5-HT1A | 450–1,800 | 294 | Human | [75][76] |
| 5-HT1B | 840 | ND | Rat | [77] |
| 5-HT2A | 18–23 | 41 | Human | [75][76] |
| 5-HT2B | 174 | ND | Human | [78] |
| 5-HT2C | 4-8 | 8.5 | Rat | [79][80] |
| 5-HT3 | 430 | 1,400 | Rat | [81] |
| 5-HT6 | 65–141 | 148 | Human/rat | [82][83][84] |
| 5-HT7 | 92.8–123 | ND | Rat | [85] |
| α1A | 6.5–25 | 18–37 | Human | [86][87] |
| α1B | 600–1700 | 850–1300 | Human | [86][87] |
| α1D | 560 | 1500 | Human | [87] |
| α2 | 114–690 | 2,030 | Human | [74][75] |
| α2A | 88 | ND | Human | [88] |
| α2B | >1000 | ND | Human | [88] |
| α2C | 120 | ND | Human | [88] |
| β | >10,000 | >10,000 | Rat | [89][80] |
| D1 | 89 | 210 (rat) | Human/rat | [90][80] |
| D2 | 196–1,460 | 2,570 | Human | [75][90] |
| D3 | 206 | ND | Human | [90] |
| D4 | ND | ND | ND | ND |
| D5 | 170 | ND | Human | [90] |
| H1 | 0.5–1.1 | 3.0–15 | Human | [90][91][92] |
| H2 | 66 | 646 | Human | [91] |
| H3 | 75,900;>1000 | 45,700 | Human | [90][91] |
| H4 | 34–26,300 | 6,920 | Human | [91][93] |
| M1 | 11.0–14.7 | 40 | Human | [94][95] |
| M2 | 11.8 | 110 | Human | [94] |
| M3 | 12.8–39 | 50 | Human | [94][95] |
| M4 | 7.2 | 84 | Human | [94] |
| M5 | 15.7–24 | 97 | Human | [94][95] |
| σ1 | 287-300 | 2,000 | Guinea pig/rat | [96][97] |
| hERG | 3,260 | 31,600 | Human | [98][99] |
| PARP1 | 1650 | ND | Human | [100] |
| TrkA | 3,000 (agonist) | ND | Human | [101] |
| TrkB | 14,000 (agonist) | ND | Human | [101] |
| Values are Ki (nM), unless otherwise noted. The smaller the value, the more strongly the drug binds to the site. | ||||
Amitriptyline inhibits serotonin transporter (SERT) and norepinephrine transporter (NET). It is metabolized to nortriptyline, a stronger norepinephrine reuptake inhibitor, further augmenting amitriptyline's effects on norepinephrine reuptake (see the Table on the right).
Amitriptyline additionally acts as a potent inhibitor of the serotonin 5-HT2A, 5-HT2C, the α1A-adrenergic, the histamine H1 and the M1-M5 muscarinic acetylcholine receptors (see the Table on the right).
Amitriptyline is a non-selective blocker of multiple ion channels, in particular, voltage-gated sodium channels Nav1.3, Nav1.5, Nav1.6, Nav1.7, and Nav1.8,[102][103][104] voltage-gated potassium channels Kv7.2/ Kv7.3,[105] Kv7.1, Kv7.1/KCNE1,[106] and hERG.[98]
Mechanism of action
Inhibition of serotonin and norepinephrine transporters by amitriptyline results in interference with neuronal reuptake of serotonin and norepinephrine. Since the reuptake process is important physiologically in terminating transmitting activity, this action may potentiate or prolong activity of serotonergic and adrenergic neurons and is believed to underlie the antidepressant activity of amitriptyline.[67]
Inhibition of norepinephrine reuptake leading to increased concentration of norepinephrine in the posterior grey column of the spinal cord appears to be mostly responsible for the analgesic action of amitriptyline. Increased level of norepinephrine increases the basal activity of alpha-2 adrenergic receptors, which mediate an analgesic effect by increasing gamma-aminobutyric acid transmission among spinal interneurons. The blocking effect of amitriptyline on sodium channels may also contribute to its efficacy in pain conditions.[4]
Pharmacokinetics
Amitriptyline is readily absorbed from the gastrointestinal tract (90–95%).[4] Absorption is gradual with the peak concentration in blood plasma reached after about 4 hours.[3] Extensive metabolism on the first pass through the liver leads to average bioavailability of about 50% (45%[3]-53%[4]). Amitriptyline is metabolized mostly by CYP2C19 into nortriptyline and by CYP2D6 leading to a variety of hydroxylated metabolites, with the principal one among them being (E)-10-hydroxynortriptyline[6] (see metabolism scheme),[4] and to a lesser degree, by CYP3A4.[7]
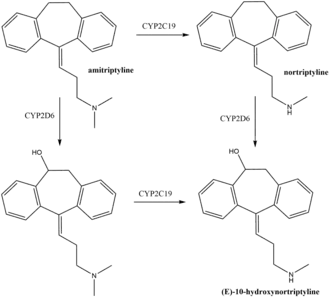
Nortriptyline, the main active metabolite of amitriptyline, is an antidepressant on its own right. Nortriptyline reaches 10% higher level in the blood plasma than the parent drug amitriptyline and 40% greater area under the curve, and its action is an important part of the overall action of amitriptyline.[3][6]
Another active metabolite is (E)-10-hydroxynortriptyline, which is a norepinephrine uptake inhibitor four times weaker than nortriptyline. (E)-10-hydroxynortiptyline blood level is comparable to that of nortriptyline, but its cerebrospinal fluid level, which is a close proxy of the brain concentration of a drug, is twice higher than nortriptyline's. Based on this, (E)-10-hydroxynortriptyline was suggested to significantly contribute to antidepressant effects of amitriptyline.[107]
Blood levels of amitriptyline and nortriptyline and pharmacokinetics of amitriptyline in general, with clearance difference of up to 10-fold, vary widely between individuals.[108] Variability of the area under the curve in steady state is also high, which makes a slow upward titration of the dose necessary.[15]
In the blood, amitriptyline is 96% bound to plasma proteins; nortriptyline is 93–95% bound, and (E)-10-hydroxynortiptyline is about 60% bound.[5][109][107] Amitriptyline has an elimination half life of 21 hours,[3] nortriptyline - 23–31 hours,[110] and (E)-10-hydroxynortiptyline - 8–10 hours.[107] Within 48 hours, 12-80% of amitriptyline is eliminated in the urine, mostly as metabolites.[8] 2% of the unchanged drug is excreted in the urine.[111] Elimination in the feces, apparently, have not been studied.
Therapeutic levels of amitriptyline range from 75 to 175 ng/mL (270–631 nM),[112] or 80–250 ng/mL of both amitriptyline and its metabolite nortriptyline.[113]
Pharmacogenetics
Since amitriptyline is primarily metabolized by CYP2D6 and CYP2C19, genetic variations within the genes coding for these enzymes can affect its metabolism, leading to changes in the concentrations of the drug in the body.[114] Increased concentrations of amitriptyline may increase the risk for side effects, including anticholinergic and nervous system adverse effects, while decreased concentrations may reduce the drug's efficacy.[115][116][117][118]
Individuals can be categorized into different types of CYP2D6 or CYP2C19 metabolizers depending on which genetic variations they carry. These metabolizer types include poor, intermediate, extensive, and ultrarapid metabolizers. Most individuals (about 77–92%) are extensive metabolizers,[44] and have "normal" metabolism of amitriptyline. Poor and intermediate metabolizers have reduced metabolism of the drug as compared to extensive metabolizers; patients with these metabolizer types may have an increased probability of experiencing side effects. Ultrarapid metabolizers use amitriptyline much faster than extensive metabolizers; patients with this metabolizer type may have a greater chance of experiencing pharmacological failure.[115][116][44][118]
The Clinical Pharmacogenetics Implementation Consortium recommends avoiding amitriptyline in patients who are CYP2D6 ultrarapid or poor metabolizers, due to the risk for a lack of efficacy and side effects, respectively. The consortium also recommends considering an alternative drug not metabolized by CYP2C19 in patients who are CYP2C19 ultrarapid metabolizers. A reduction in starting dose is recommended for patients who are CYP2D6 intermediate metabolizers and CYP2C19 poor metabolizers. If use of amitriptyline is warranted, therapeutic drug monitoring is recommended to guide dose adjustments.[44] The Dutch Pharmacogenetics Working Group also recommends selecting an alternative drug or monitoring plasma concentrations of amitriptyline in patients who are CYP2D6 poor or ultrarapid metabolizers, and selecting an alternative drug or reducing initial dose in patients who are CYP2D6 intermediate metabolizers.[119]
Chemistry
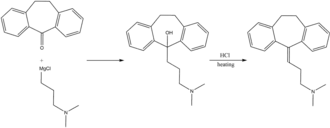
Amitriptyline is a highly lipophilic molecule having an octanol-water partition coefficient (pH 7.4) of 3.0,[120] while the log P of the free base was reported as 4.92.[121] Solubility of the free base amitriptyline in water is 14 mg/L.[122] Amitriptyline is prepared by reacting dibenzosuberone with 3-(dimethylamino)propylmagnesium chloride and then heating the resulting intermediate product with hydrochloric acid to eliminate water.[4]
History
Amitriptyline was first developed by the American pharmaceutical company Merck in the late 1950s. In 1958, Merck approached a number of clinical investigators proposing to conduct clinical trials of amitriptyline for schizophrenia. One of these researchers, Frank Ayd, instead, suggested using amitriptyline for depression. Ayd treated 130 patients and, in 1960, reported that amitriptyline had antidepressant properties similar to another, and the only known at the time, tricyclic antidepressant imipramine.[123] Following this, the US Food and Drug Administration approved amitriptyline for depression in 1961.[16]
In Europe, due to a quirk of the patent law at the time allowing patents only on the chemical synthesis but not on the drug itself, Roche and Lundbeck were able to independently develop and market amitriptyline in the early 1960s.[124]
According to research by the historian of psychopharmacology David Healy, amitriptyline became a much bigger selling drug than its precursor imipramine because of two factors. First, amitriptyline has much stronger anxiolytic effect. Second, Merck conducted a marketing campaign raising clinicians' awareness of depression as a clinical entity.[124][123]
Society and culture

English folk singer Nick Drake died from an overdose of Tryptizol in 1974.[125]
Senteni Masango, wife of Swaziland King Mswati, died on 6 April 2018 after committing suicide by overdosing on amytriptyline capsules.[126]
In the 2021 film The Many Saints of Newark, amitriptyline (referred to by the brand name Elavil) is part of the plot line of the movie.[127]
Generic names
Amitriptyline is the English and French generic name of the drug and its INN, BAN, and DCF, while amitriptyline hydrochloride is its USAN, USP, BANM, and JAN.[128][129][130][131] Its generic name in Spanish and Italian and its DCIT are amitriptilina, in German is Amitriptylin, and in Latin is amitriptylinum.[129][131] The embonate salt is known as amitriptyline embonate, which is its BANM, or as amitriptyline pamoate unofficially.[129]
Prescription trends
Between 1998 and 2017, along with imipramine, amitriptyline was the most commonly prescribed first antidepressant for children aged 5-11 years in England. It was also the most prescribed antidepressant (along with fluoxetine) for 12 to 17 year olds. [132]
Research
The few randomized controlled trials investigating amitriptyline efficacy in eating disorder have been discouraging.[133]
References
- "Amitriptyline". Oxford Dictionary. Archived from the original on 14 July 2014. Retrieved 6 January 2021 – via Lexico.com.
- "Amitriptyline Use During Pregnancy". Drugs.com. 2 September 2020. Archived from the original on 9 November 2020. Retrieved 13 September 2020.
- Schulz P, Dick P, Blaschke TF, Hollister L (1985). "Discrepancies between pharmacokinetic studies of amitriptyline". Clin Pharmacokinet. 10 (3): 257–68. doi:10.2165/00003088-198510030-00005. PMID 3893842. S2CID 41881790.
- McClure EW, Daniels RN (February 2021). "Classics in Chemical Neuroscience: Amitriptyline". ACS Chem Neurosci. 12 (3): 354–362. doi:10.1021/acschemneuro.0c00467. PMID 33438398. S2CID 231596860.
- "Endep Amitriptyline hydrochloride" (PDF). TGA eBusiness Services. Alphapharm Pty Limited. 10 December 2012. Archived from the original on 13 August 2017. Retrieved 1 December 2013.
- Breyer-Pfaff U (October 2004). "The metabolic fate of amitriptyline, nortriptyline and amitriptylinoxide in man". Drug Metab Rev. 36 (3–4): 723–46. doi:10.1081/dmr-200033482. PMID 15554244. S2CID 25565048.
- Venkatakrishnan K, Schmider J, Harmatz JS, Ehrenberg BL, von Moltke LL, Graf JA, Mertzanis P, Corbett KE, Rodriguez MC, Shader RI, Greenblatt DJ (October 2001). "Relative contribution of CYP3A to amitriptyline clearance in humans: in vitro and in vivo studies". J Clin Pharmacol. 41 (10): 1043–54. doi:10.1177/00912700122012634. PMID 11583471. S2CID 27146286.
- Schulz P, Balant-Gorgia AE, Kubli A, Gertsch-Genet C, Garrone G (1983). "Elimination and pharmacological effects following single oral doses of 50 and 75 mg of amitriptyline in man". Arch Psychiatr Nervenkr (1970). 233 (6): 449–55. doi:10.1007/BF00342785. PMID 6667101. S2CID 20844722.
- Blessel KW, Rudy BC, Senkowski BZ (1974). "Amitriptyline Hydrochloride". Analytical Profiles of Drug Substances. 3: 127–148. doi:10.1016/S0099-5428(08)60066-0. ISBN 9780122608032.
- "Amitriptyline Tablets BP 50mg – Summary of Product Characteristics (SPC)". electronic Medicines Compendium. Actavis UK Ltd. 24 March 2013. Archived from the original on 3 December 2013. Retrieved 1 December 2013.
- Hitchings A, Lonsdale D, Burrage D, Baker E (2015). Top 100 drugs : clinical pharmacology and practical prescribing. p. 50. ISBN 978-0-7020-5516-4.
- Alam U, Sloan G, Tesfaye S (March 2020). "Treating Pain in Diabetic Neuropathy: Current and Developmental Drugs". Drugs. 80 (4): 363–384. doi:10.1007/s40265-020-01259-2. PMID 32040849. S2CID 211074023.
- Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Fluß E, Choy E, Kosek E, Amris K, Branco J, Dincer F, Leino-Arjas P, Longley K, McCarthy GM, Makri S, Perrot S, Sarzi-Puttini P, Taylor A, Jones GT (February 2017). "EULAR revised recommendations for the management of fibromyalgia". Ann Rheum Dis. 76 (2): 318–328. doi:10.1136/annrheumdis-2016-209724. PMID 27377815.
- Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E (April 2012). "Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society". Neurology. 78 (17): 1337–45. doi:10.1212/WNL.0b013e3182535d20. PMC 3335452. PMID 22529202.
- Tfelt-Hansen P, Ågesen FN, Pavbro A, Tfelt-Hansen J (May 2017). "Pharmacokinetic Variability of Drugs Used for Prophylactic Treatment of Migraine". CNS Drugs. 31 (5): 389–403. doi:10.1007/s40263-017-0430-3. PMID 28405886. S2CID 23560743.
- Fangmann P, Assion HJ, Juckel G, González CA, López-Muñoz F (February 2008). "Half a century of antidepressant drugs: on the clinical introduction of monoamine oxidase inhibitors, tricyclics, and tetracyclics. Part II: tricyclics and tetracyclics". Journal of Clinical Psychopharmacology. 28 (1): 1–4. doi:10.1097/jcp.0b013e3181627b60. PMID 18204333. S2CID 31018835.
- World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. 2021. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- "Amitriptyline Hydrochloride". Drugs.com. The American Society of Health-System Pharmacists. Archived from the original on 24 September 2014. Retrieved 25 September 2014.
- "The Top 300 of 2020". ClinCalc.com. Retrieved 7 October 2022.
- "Amitriptyline - Drug Usage Statistics". ClinCalc.com. Retrieved 7 October 2022.
- Leucht C, Huhn M, Leucht S (December 2012). "Amitriptyline versus placebo for major depressive disorder". Cochrane Database Syst Rev. 12: CD009138. doi:10.1002/14651858.CD009138.pub2. PMID 23235671.
- Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- Zhou X, Michael KD, Liu Y, Del Giovane C, Qin B, Cohen D, Gentile S, Xie P (November 2014). "Systematic review of management for treatment-resistant depression in adolescents". BMC Psychiatry. 14: 340. doi:10.1186/s12888-014-0340-6. PMC 4254264. PMID 25433401.
- Riblet N, Larson R, Watts BV, Holtzheimer P (2014). "Reevaluating the role of antidepressants in cancer-related depression: a systematic review and meta-analysis". Gen Hosp Psychiatry. 36 (5): 466–73. doi:10.1016/j.genhosppsych.2014.05.010. PMID 24950919.
- "Parkinson's disease". merckmanuals.com. Merck Sharp & Dohme Corp. August 2007. Archived from the original on 18 November 2013. Retrieved 22 December 2013.
- Seppi K, Weintraub D, Coelho M, Perez-Lloret S, Fox SH, Katzenschlager R, Hametner EM, Poewe W, Rascol O, Goetz CG, Sampaio C (October 2011). "The Movement Disorder Society Evidence-Based Medicine Review Update: Treatments for the non-motor symptoms of Parkinson's disease". Mov Disord. 26 (Suppl 3): S42–80. doi:10.1002/mds.23884. PMC 4020145. PMID 22021174.
- Liampas A, Rekatsina M, Vadalouca A, Paladini A, Varrassi G, Zis P (November 2020). "Pharmacological Management of Painful Peripheral Neuropathies: A Systematic Review". Pain Ther. 10 (1): 55–68. doi:10.1007/s40122-020-00210-3. ISSN 2193-8237. PMC 8119529. PMID 33145709.
- Sommer C, Alten R, Bär KJ, Bernateck M, Brückle W, Friedel E, Henningsen P, Petzke F, Tölle T, Üçeyler N, Winkelmann A, Häuser W (June 2017). "[Drug therapy of fibromyalgia syndrome : Updated guidelines 2017 and overview of systematic review articles]". Schmerz (in German). 31 (3): 274–284. doi:10.1007/s00482-017-0207-0. PMID 28493231.
- Thorpe J, Shum B, Moore RA, Wiffen PJ, Gilron I (February 2018). "Combination pharmacotherapy for the treatment of fibromyalgia in adults". Cochrane Database Syst Rev. 2: CD010585. doi:10.1002/14651858.CD010585.pub2. PMC 6491103. PMID 29457627.
- van den Beuken-van Everdingen MH, de Graeff A, Jongen JL, Dijkstra D, Mostovaya I, Vissers KC (March 2017). "Pharmacological Treatment of Pain in Cancer Patients: The Role of Adjuvant Analgesics, a Systematic Review". Pain Pract. 17 (3): 409–419. doi:10.1111/papr.12459. PMID 27207115. S2CID 37418010.
- Do TM, Unis GD, Kattar N, Ananth A, McCoul ED (October 2020). "Neuromodulators for Atypical Facial Pain and Neuralgias: A Systematic Review and Meta-Analysis". Laryngoscope. 131 (6): 1235–1253. doi:10.1002/lary.29162. PMID 33037835. S2CID 222256076.
- Loder E, Rizzoli P (November 2018). "Pharmacologic Prevention of Migraine: A Narrative Review of the State of the Art in 2018". Headache. 58 (Suppl 3): 218–229. doi:10.1111/head.13375. PMID 30137671. S2CID 52071815.
- Oskoui M, Pringsheim T, Billinghurst L, Potrebic S, Gersz EM, Gloss D, Holler-Managan Y, Leininger E, Licking N, Mack K, Powers SW, Sowell M, Victorio MC, Yonker M, Zanitsch H, Hershey AD (September 2019). "Practice guideline update summary: Pharmacologic treatment for pediatric migraine prevention: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology and the American Headache Society". Neurology. 93 (11): 500–509. doi:10.1212/WNL.0000000000008105. PMC 6746206. PMID 31413170.
- Ghadiri-Sani M, Silver N (February 2016). "Headache (chronic tension-type)". BMJ Clin Evid. 2016. PMC 4747324. PMID 26859719.
- Trinkley KE, Nahata MC (2014). "Medication management of irritable bowel syndrome". Digestion. 89 (4): 253–67. doi:10.1159/000362405. PMID 24992947.
- de Bruijn CM, Rexwinkel R, Gordon M, Benninga M, Tabbers MM (February 2021). "Antidepressants for functional abdominal pain disorders in children and adolescents". The Cochrane Database of Systematic Reviews. 2 (3): CD008013. doi:10.1002/14651858.CD008013.pub3. PMC 8094232. PMID 33560523.
- Venkatesan T, Levinthal DJ, Tarbell SE, Jaradeh SS, Hasler WL, Issenman RM, Adams KA, Sarosiek I, Stave CD, Sharaf RN, Sultan S, Li BU (June 2019). "Guidelines on management of cyclic vomiting syndrome in adults by the American Neurogastroenterology and Motility Society and the Cyclic Vomiting Syndrome Association". Neurogastroenterol Motil. 31 (Suppl 2): e13604. doi:10.1111/nmo.13604. PMC 6899751. PMID 31241819.
- Giusto LL, Zahner PM, Shoskes DA (July 2018). "An evaluation of the pharmacotherapy for interstitial cystitis". Expert Opin Pharmacother. 19 (10): 1097–1108. doi:10.1080/14656566.2018.1491968. PMID 29972328. S2CID 49674883.
- Colemeadow J, Sahai A, Malde S (2020). "Clinical Management of Bladder Pain Syndrome/Interstitial Cystitis: A Review on Current Recommendations and Emerging Treatment Options". Res Rep Urol. 12: 331–343. doi:10.2147/RRU.S238746. PMC 7455607. PMID 32904438.
- Caldwell PH, Sureshkumar P, Wong WC (January 2016). "Tricyclic and related drugs for nocturnal enuresis in children". Cochrane Database Syst Rev. 2016 (1): CD002117. doi:10.1002/14651858.CD002117.pub2. PMC 8741207. PMID 26789925.
- Klein T, Woo TM, Panther S, Odom-Maryon T, Daratha K (2019). "Somnolence-Producing Agents: A 5-Year Study of Prescribing for Medicaid-Insured Children With Attention Deficit Hyperactivity Disorder". J Pediatr Health Care. 33 (3): e1–e8. doi:10.1016/j.pedhc.2018.10.002. PMID 30630642. S2CID 58577978.
- Everitt H, McDermott L, Leydon G, Yules H, Baldwin D, Little P (February 2014). "GPs' management strategies for patients with insomnia: a survey and qualitative interview study". Br J Gen Pract. 64 (619): e112–9. doi:10.3399/bjgp14X677176. PMC 3905408. PMID 24567616.
- Everitt H, Baldwin DS, Stuart B, Lipinska G, Mayers A, Malizia AL, Manson CC, Wilson S (May 2018). "Antidepressants for insomnia in adults". Cochrane Database Syst Rev. 2018 (5): CD010753. doi:10.1002/14651858.CD010753.pub2. PMC 6494576. PMID 29761479.
- Hicks JK, Swen JJ, Thorn CF, Sangkuhl K, Kharasch ED, Ellingrod VL, Skaar TC, Müller DJ, Gaedigk A, Stingl JC (May 2013). "Clinical Pharmacogenetics Implementation Consortium guideline for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants". Clin Pharmacol Ther. 93 (5): 402–8. doi:10.1038/clpt.2013.2. PMC 3689226. PMID 23486447.
- Nielsen RE, Damkier P (June 2012). "Pharmacological treatment of unipolar depression during pregnancy and breast-feeding--a clinical overview". Nord J Psychiatry. 66 (3): 159–66. doi:10.3109/08039488.2011.650198. PMID 22283766. S2CID 11327135.
- Domecq JP, Prutsky G, Leppin A, Sonbol MB, Altayar O, Undavalli C, Wang Z, Elraiyah T, Brito JP, Mauck KF, Lababidi MH, Prokop LJ, Asi N, Wei J, Fidahussein S, Montori VM, Murad MH (February 2015). "Clinical review: Drugs commonly associated with weight change: a systematic review and meta-analysis". J Clin Endocrinol Metab. 100 (2): 363–70. doi:10.1210/jc.2014-3421. PMC 5393509. PMID 25590213.
- Rissardo JP, Caprara AL (April 2020). "The Link Between Amitriptyline and Movement Disorders: Clinical Profile and Outcome". Annals of the Academy of Medicine, Singapore. 49 (4): 236–251. doi:10.47102/annals-acadmed.sg.202023. PMID 32419008. S2CID 218679271.
- Leucht C, Huhn M, Leucht S (December 2012). "Amitriptyline versus placebo for major depressive disorder". The Cochrane Database of Systematic Reviews. Wiley. 12: CD009138. doi:10.1002/14651858.cd009138.pub2. PMID 23235671.
- Chen LW, Chen MY, Lian ZP, Lin HS, Chien CC, Yin HL, Chu YH, Chen KY (March 2018). "Amitriptyline and Sexual Function: A Systematic Review Updated for Sexual Health Practice". Am J Mens Health. 12 (2): 370–379. doi:10.1177/1557988317734519. PMC 5818113. PMID 29019272.
- Amitriptyline. National Institute of Diabetes and Digestive and Kidney Diseases. 6 January 2012. PMID 31643729. Archived from the original on 21 January 2022. Retrieved 6 January 2021 – via PubMed.
- Voican CS, Corruble E, Naveau S, Perlemuter G (April 2014). "Antidepressant-induced liver injury: a review for clinicians". Am J Psychiatry. 171 (4): 404–15. doi:10.1176/appi.ajp.2013.13050709. PMID 24362450.
- HOLMBERG MB, JANSSON (1962). "A study of blood count and serum transaminase in prolonged treatment with amitriptyline". J New Drugs. 2 (6): 361–5. doi:10.1177/009127006200200606. PMID 13961401.
- Zemrak WR, Kenna GA (June 2008). "Association of antipsychotic and antidepressant drugs with Q-T interval prolongation". American Journal of Health-System Pharmacy. 65 (11): 1029–38. doi:10.2146/ajhp070279. PMID 18499875. Archived from the original on 21 December 2016.
- Hefner G, Hahn M, Hohner M, Roll SC, Klimke A, Hiemke C (January 2019). "QTc Time Correlates with Amitriptyline and Venlafaxine Serum Levels in Elderly Psychiatric Inpatients". Pharmacopsychiatry. 52 (1): 38–43. doi:10.1055/s-0044-102009. PMID 29466824.
- Campleman SL, Brent J, Pizon AF, Shulman J, Wax P, Manini AF (December 2020). "Drug-specific risk of severe QT prolongation following acute drug overdose". Clin Toxicol (Phila). 58 (12): 1326–1334. doi:10.1080/15563650.2020.1746330. PMC 7541562. PMID 32252558.
- Joint Formulary Committee (2013). British National Formulary (BNF) (65th ed.). London, UK: Pharmaceutical Press. ISBN 978-0-85711-084-8.
- Leucht S, Hackl HJ, Steimer W, Angersbach D, Zimmer R (January 2000). "Effect of adjunctive paroxetine on serum levels and side-effects of tricyclic antidepressants in depressive inpatients". Psychopharmacology (Berl). 147 (4): 378–83. doi:10.1007/s002130050006. PMID 10672631. S2CID 22476829.
- Jerling M, Bertilsson L, Sjöqvist F (February 1994). "The use of therapeutic drug monitoring data to document kinetic drug interactions: an example with amitriptyline and nortriptyline". Ther Drug Monit. 16 (1): 1–12. doi:10.1097/00007691-199402000-00001. PMID 7909176. S2CID 1428027.
- Vandel S, Bertschy G, Baumann P, Bouquet S, Bonin B, Francois T, Sechter D, Bizouard P (June 1995). "Fluvoxamine and fluoxetine: interaction studies with amitriptyline, clomipramine and neuroleptics in phenotyped patients". Pharmacol Res. 31 (6): 347–53. doi:10.1016/1043-6618(95)80088-3. PMID 8685072.
- Vandel S, Bertschy G, Bonin B, Nezelof S, François TH, Vandel B, Sechter D, Bizouard P (1992). "Tricyclic antidepressant plasma levels after fluoxetine addition". Neuropsychobiology. 25 (4): 202–7. doi:10.1159/000118838. PMID 1454161.
- Castberg I, Helle J, Aamo TO (October 2005). "Prolonged pharmacokinetic drug interaction between terbinafine and amitriptyline". Ther Drug Monit. 27 (5): 680–2. doi:10.1097/01.ftd.0000175910.68539.33. PMID 16175144.
- Curry SH, DeVane CL, Wolfe MM (1985). "Cimetidine interaction with amitriptyline". Eur J Clin Pharmacol. 29 (4): 429–33. doi:10.1007/BF00613457. PMID 3912187. S2CID 25430195.
- Johne A, Schmider J, Brockmöller J, Stadelmann AM, Störmer E, Bauer S, Scholler G, Langheinrich M, Roots I (February 2002). "Decreased plasma levels of amitriptyline and its metabolites on comedication with an extract from St. John's wort ( Hypericum perforatum )". J Clin Psychopharmacol. 22 (1): 46–54. doi:10.1097/00004714-200202000-00008. PMID 11799342. S2CID 25670895.
- Berry-Bibee EN, Kim MJ, Simmons KB, Tepper NK, Riley HE, Pagano HP, Curtis KM (December 2016). "Drug interactions between hormonal contraceptives and psychotropic drugs: a systematic review". Contraception. 94 (6): 650–667. doi:10.1016/j.contraception.2016.07.011. PMID 27444984.
- Wong SL, Cavanaugh J, Shi H, Awni WM, Granneman GR (July 1996). "Effects of divalproex sodium on amitriptyline and nortriptyline pharmacokinetics". Clin Pharmacol Ther. 60 (1): 48–53. doi:10.1016/S0009-9236(96)90166-6. PMID 8689811. S2CID 37720622.
- Gillman PK (June 2006). "A review of serotonin toxicity data: implications for the mechanisms of antidepressant drug action". Biol Psychiatry. 59 (11): 1046–51. doi:10.1016/j.biopsych.2005.11.016. PMID 16460699. S2CID 12179122.
- "DailyMed - AMITRIPTYLINE HYDROCHLORIDE tablet, film coated". Archived from the original on 25 January 2021. Retrieved 2 February 2021.
- Bialer M, Doose DR, Murthy B, Curtin C, Wang SS, Twyman RE, Schwabe S (2004). "Pharmacokinetic interactions of topiramate". Clin Pharmacokinet. 43 (12): 763–80. doi:10.2165/00003088-200443120-00001. PMID 15355124. S2CID 10427097.
- Meyer JF, McAllister CK, Goldberg LI (August 1970). "Insidious and prolonged antagonism of guanethidine by amitriptyline". JAMA. 213 (9): 1487–8. doi:10.1001/jama.1970.03170350053016. PMID 5468457.
- Maany I, Hayashida M, Pfeffer SL, Kron RE (June 1982). "Possible toxic interaction between disulfiram and amitriptyline". Arch Gen Psychiatry. 39 (6): 743–4. doi:10.1001/archpsyc.1982.04290060083018. PMID 7092508.
- "CHAPTER 132 ORAL ANTICOAGULATION | Free Medical Textbook". 9 February 2012. Archived from the original on 27 September 2020. Retrieved 2 February 2021.
- Roth BL, Driscol J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Archived from the original on 27 August 2021. Retrieved 14 August 2017.
- Tatsumi M, Groshan K, Blakely RD, Richelson E (1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". Eur. J. Pharmacol. 340 (2–3): 249–58. doi:10.1016/s0014-2999(97)01393-9. PMID 9537821.
- Owens MJ, Morgan WN, Plott SJ, Nemeroff CB (1997). "Neurotransmitter receptor and transporter binding profile of antidepressants and their metabolites". J. Pharmacol. Exp. Ther. 283 (3): 1305–22. PMID 9400006.
- Cusack B, Nelson A, Richelson E (1994). "Binding of antidepressants to human brain receptors: focus on newer generation compounds". Psychopharmacology. 114 (4): 559–65. doi:10.1007/bf02244985. PMID 7855217. S2CID 21236268.
- Peroutka SJ (1988). "Antimigraine drug interactions with serotonin receptor subtypes in human brain". Ann. Neurol. 23 (5): 500–4. doi:10.1002/ana.410230512. PMID 2898916. S2CID 41570165.
- Peroutka SJ (1986). "Pharmacological differentiation and characterization of 5-HT1A, 5-HT1B, and 5-HT1C binding sites in rat frontal cortex". J. Neurochem. 47 (2): 529–40. doi:10.1111/j.1471-4159.1986.tb04532.x. PMID 2942638. S2CID 25108290.
- Schmuck K, Ullmer C, Kalkman HO, Probst A, Lubbert H (1996). "Activation of meningeal 5-HT2B receptors: an early step in the generation of migraine headache?". Eur. J. Neurosci. 8 (5): 959–67. doi:10.1111/j.1460-9568.1996.tb01583.x. PMID 8743744. S2CID 19578349.
- Pälvimäki EP, Roth BL, Majasuo H, Laakso A, Kuoppamäki M, Syvälahti E, Hietala J (1996). "Interactions of selective serotonin reuptake inhibitors with the serotonin 5-HT2c receptor". Psychopharmacology. 126 (3): 234–40. doi:10.1007/bf02246453. PMID 8876023. S2CID 24889381.
- Sánchez C, Hyttel J (August 1999). "Comparison of the effects of antidepressants and their metabolites on reuptake of biogenic amines and on receptor binding". Cell Mol Neurobiol. 19 (4): 467–89. doi:10.1023/a:1006986824213. PMID 10379421. S2CID 19490821.
- Schmidt AW, Hurt SD, Peroutka SJ (1989). "'[3H]quipazine' degradation products label 5-HT uptake sites". Eur. J. Pharmacol. 171 (1): 141–3. doi:10.1016/0014-2999(89)90439-1. PMID 2533080.
- Kohen R, Metcalf MA, Khan N, Druck T, Huebner K, Lachowicz JE, Meltzer HY, Sibley DR, Roth BL, Hamblin MW (1996). "Cloning, characterization, and chromosomal localization of a human 5-HT6 serotonin receptor". J. Neurochem. 66 (1): 47–56. doi:10.1046/j.1471-4159.1996.66010047.x. PMID 8522988. S2CID 35874409.
- Hirst WD, Abrahamsen B, Blaney FE, Calver AR, Aloj L, Price GW, Medhurst AD (2003). "Differences in the central nervous system distribution and pharmacology of the mouse 5-hydroxytryptamine-6 receptor compared with rat and human receptors investigated by radioligand binding, site-directed mutagenesis, and molecular modeling". Mol. Pharmacol. 64 (6): 1295–308. doi:10.1124/mol.64.6.1295. PMID 14645659. S2CID 33743899.
- Monsma FJ, Shen Y, Ward RP, Hamblin MW, Sibley DR (1993). "Cloning and expression of a novel serotonin receptor with high affinity for tricyclic psychotropic drugs". Mol. Pharmacol. 43 (3): 320–7. PMID 7680751.
- Shen Y, Monsma FJ, Metcalf MA, Jose PA, Hamblin MW, Sibley DR (1993). "Molecular cloning and expression of a 5-hydroxytryptamine7 serotonin receptor subtype". J. Biol. Chem. 268 (24): 18200–4. doi:10.1016/S0021-9258(17)46830-X. PMID 8394362.
- Nojimoto FD, Mueller A, Hebeler-Barbosa F, Akinaga J, Lima V, Kiguti LR, Pupo AS (2010). "The tricyclic antidepressants amitriptyline, nortriptyline and imipramine are weak antagonists of human and rat alpha1B-adrenoceptors". Neuropharmacology. 59 (1–2): 49–57. doi:10.1016/j.neuropharm.2010.03.015. PMID 20363235. S2CID 207225294.
- Proudman RG, Pupo AS, Baker JG (August 2020). "The affinity and selectivity of α-adrenoceptor antagonists, antidepressants, and antipsychotics for the human α1A, α1B, and α1D-adrenoceptors". Pharmacol Res Perspect. 8 (4): e00602. doi:10.1002/prp2.602. PMC 7327383. PMID 32608144.
- Fallarero A, Pohjanoksa K, Wissel G, Parkkisenniemi-Kinnunen UM, Xhaard H, Scheinin M, Vuorela P (December 2012). "High-throughput screening with a miniaturized radioligand competition assay identifies new modulators of human α2-adrenoceptors". Eur J Pharm Sci. 47 (5): 941–51. doi:10.1016/j.ejps.2012.08.021. PMID 22982401.
- Bylund DB, Snyder SH (1976). "Beta adrenergic receptor binding in membrane preparations from mammalian brain". Mol. Pharmacol. 12 (4): 568–80. PMID 8699.
- von Coburg Y, Kottke T, Weizel L, Ligneau X, Stark H (2009). "Potential utility of histamine H3 receptor antagonist pharmacophore in antipsychotics". Bioorg. Med. Chem. Lett. 19 (2): 538–42. doi:10.1016/j.bmcl.2008.09.012. PMID 19091563.
- Appl H, Holzammer T, Dove S, Haen E, Strasser A, Seifert R (February 2012). "Interactions of recombinant human histamine H1, H2, H3, and H4 receptors with 34 antidepressants and antipsychotics". Naunyn Schmiedebergs Arch. Pharmacol. 385 (2): 145–70. doi:10.1007/s00210-011-0704-0. PMID 22033803. S2CID 14274150.
- Ghoneim OM, Legere JA, Golbraikh A, Tropsha A, Booth RG (2006). "Novel ligands for the human histamine H1 receptor: synthesis, pharmacology, and comparative molecular field analysis studies of 2-dimethylamino-5-(6)-phenyl-1,2,3,4-tetrahydronaphthalenes". Bioorg. Med. Chem. 14 (19): 6640–58. doi:10.1016/j.bmc.2006.05.077. PMID 16782354.
- Nguyen T, Shapiro DA, George SR, Setola V, Lee DK, Cheng R, Rauser L, Lee SP, Lynch KR, Roth BL, O'Dowd BF (2001). "Discovery of a novel member of the histamine receptor family". Mol. Pharmacol. 59 (3): 427–33. doi:10.1124/mol.59.3.427. PMID 11179435. Archived from the original on 27 August 2021. Retrieved 11 December 2019.
- Stanton T, Bolden-Watson C, Cusack B, Richelson E (1993). "Antagonism of the five cloned human muscarinic cholinergic receptors expressed in CHO-K1 cells by antidepressants and antihistaminics". Biochem. Pharmacol. 45 (11): 2352–4. doi:10.1016/0006-2952(93)90211-e. PMID 8100134.
- Bymaster FP, Nelson DL, DeLapp NW, Falcone JF, Eckols K, Truex LL, Foreman MM, Lucaites VL, Calligaro DO (1999). "Antagonism by olanzapine of dopamine D1, serotonin2, muscarinic, histamine H1 and alpha 1-adrenergic receptors in vitro". Schizophr. Res. 37 (1): 107–22. doi:10.1016/s0920-9964(98)00146-7. PMID 10227113. S2CID 19891653.
- Weber E, Sonders M, Quarum M, McLean S, Pou S, Keana JF (1986). "1,3-Di(2-[5-3H]tolyl)guanidine: a selective ligand that labels sigma-type receptors for psychotomimetic opiates and antipsychotic drugs". Proc. Natl. Acad. Sci. U.S.A. 83 (22): 8784–8. Bibcode:1986PNAS...83.8784W. doi:10.1073/pnas.83.22.8784. PMC 387016. PMID 2877462.
- Werling LL, Keller A, Frank JG, Nuwayhid SJ (October 2007). "A comparison of the binding profiles of dextromethorphan, memantine, fluoxetine and amitriptyline: treatment of involuntary emotional expression disorder". Exp Neurol. 207 (2): 248–57. doi:10.1016/j.expneurol.2007.06.013. PMID 17689532. S2CID 38476281.
- Jo SH, Youm JB, Lee CO, Earm YE, Ho WK (April 2000). "Blockade of the HERG human cardiac K(+) channel by the antidepressant drug amitriptyline". Br J Pharmacol. 129 (7): 1474–80. doi:10.1038/sj.bjp.0703222. PMC 1571977. PMID 10742304.
- Yamakawa Y, Furutani K, Inanobe A, Ohno Y, Kurachi Y (February 2012). "Pharmacophore modeling for hERG channel facilitation". Biochem Biophys Res Commun. 418 (1): 161–6. doi:10.1016/j.bbrc.2011.12.153. PMID 22244872.
- Fu L, Wang S, Wang X, Wang P, Zheng Y, Yao D, et al. (December 2016). "Crystal structure-based discovery of a novel synthesized PARP1 inhibitor (OL-1) with apoptosis-inducing mechanisms in triple-negative breast cancer". Scientific Reports. 6 (1): 3. doi:10.1038/s41598-016-0007-2. PMC 5431371. PMID 28442756.
- Jang SW, Liu X, Chan CB, Weinshenker D, Hall RA, Xiao G, Ye K (June 2009). "Amitriptyline is a TrkA and TrkB receptor agonist that promotes TrkA/TrkB heterodimerization and has potent neurotrophic activity". Chemistry & Biology. 16 (6): 644–56. doi:10.1016/j.chembiol.2009.05.010. PMC 2844702. PMID 19549602.
- Horishita T, Yanagihara N, Ueno S, Okura D, Horishita R, Minami T, Ogata Y, Sudo Y, Uezono Y, Sata T, Kawasaki T (December 2017). "Antidepressants inhibit Nav1.3, Nav1.7, and Nav1.8 neuronal voltage-gated sodium channels more potently than Nav1.2 and Nav1.6 channels expressed in Xenopus oocytes". Naunyn Schmiedebergs Arch Pharmacol. 390 (12): 1255–1270. doi:10.1007/s00210-017-1424-x. PMID 28905186. S2CID 23385313.
- Atkin TA, Maher CM, Gerlach AC, Gay BC, Antonio BM, Santos SC, Padilla KM, Rader J, Krafte DS, Fox MA, Stewart GR, Petrovski S, Devinsky O, Might M, Petrou S, Goldstein DB (April 2018). "A comprehensive approach to identifying repurposed drugs to treat SCN8A epilepsy". Epilepsia. 59 (4): 802–813. doi:10.1111/epi.14037. PMID 29574705. S2CID 4478321.
- Nau C, Seaver M, Wang SY, Wang GK (March 2000). "Block of human heart hH1 sodium channels by amitriptyline". J Pharmacol Exp Ther. 292 (3): 1015–23. PMID 10688618.
- Punke MA, Friederich P (May 2007). "Amitriptyline is a potent blocker of human Kv1.1 and Kv7.2/7.3 channels". Anesthesia and Analgesia. 104 (5): 1256–1264. doi:10.1213/01.ane.0000260310.63117.a2. PMID 17456683. S2CID 21924741. Archived from the original on 27 August 2021. Retrieved 15 October 2009.
- Villatoro-Gómez K, Pacheco-Rojas DO, Moreno-Galindo EG, Navarro-Polanco RA, Tristani-Firouzi M, Gazgalis D, Cui M, Sánchez-Chapula JA, Ferrer T (June 2018). "Molecular determinants of Kv7.1/KCNE1 channel inhibition by amitriptyline". Biochem Pharmacol. 152: 264–271. doi:10.1016/j.bcp.2018.03.016. PMID 29621539. S2CID 4929937.
- Nordin C, Bertilsson L (January 1995). "Active hydroxymetabolites of antidepressants. Emphasis on E-10-hydroxy-nortriptyline". Clin Pharmacokinet. 28 (1): 26–40. doi:10.2165/00003088-199528010-00004. PMID 7712660. S2CID 38046048.
- Bryson HM, Wilde MI (June 1996). "Amitriptyline. A review of its pharmacological properties and therapeutic use in chronic pain states". Drugs Aging. 8 (6): 459–76. doi:10.2165/00002512-199608060-00008. PMID 8736630.
- "Pamelor, Aventyl (nortriptyline) dosing, indications, interactions, adverse effects, and more". Medscape Reference. WebMD. Archived from the original on 3 December 2013. Retrieved 2 December 2013.
- Dawlilng S, Lynn K, Rosser R, Braithwaite R (July 1981). "The pharmacokinetics of nortriptyline in patients with chronic renal failure". Br J Clin Pharmacol. 12 (1): 39–45. doi:10.1111/j.1365-2125.1981.tb01852.x. PMC 1401753. PMID 7248140.
- "Amitriptyline". drugbank.ca. Archived from the original on 30 January 2019. Retrieved 29 January 2019.
- Sadock BJ, Sadock VA (2008). Kaplan & Sadock's Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins. pp. 18–. ISBN 978-0-7817-8746-8. Archived from the original on 8 July 2017.
- Orsulak PJ (September 1989). "Therapeutic monitoring of antidepressant drugs: guidelines updated". Therapeutic Drug Monitoring. 11 (5): 497–507. doi:10.1097/00007691-198909000-00002. PMID 2683251.
- Rudorfer MV, Potter WZ (1999). "Metabolism of tricyclic antidepressants". Cell Mol Neurobiol. 19 (3): 373–409. doi:10.1023/A:1006949816036. PMID 10319193. S2CID 7940406.
- Stingl JC, Brockmoller J, Viviani R (2013). "Genetic variability of drug-metabolizing enzymes: the dual impact on psychiatric therapy and regulation of brain function". Mol Psychiatry. 18 (3): 273–87. doi:10.1038/mp.2012.42. PMID 22565785. S2CID 20888081.
- Kirchheiner J, Seeringer A (2007). "Clinical implications of pharmacogenetics of cytochrome P450 drug metabolizing enzymes". Biochim Biophys Acta. 1770 (3): 489–94. doi:10.1016/j.bbagen.2006.09.019. PMID 17113714.
- Hicks JK, Swen JJ, Thorn CF, Sangkuhl K, Kharasch ED, Ellingrod VL, Skaar TC, Muller DJ, Gaedigk A, Stingl JC (2013). "Clinical Pharmacogenetics Implementation Consortium Guideline for CYP2D6 and CYP2C19 Genotypes and Dosing of Tricyclic Antidepressants" (PDF). Clinical Pharmacology & Therapeutics. 93 (5): 402–8. doi:10.1038/clpt.2013.2. PMC 3689226. PMID 23486447. Archived from the original on 27 August 2021. Retrieved 4 November 2018.
- Dean L (2017). "Amitriptyline Therapy and CYP2D6 and CYP2C19 Genotype". In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520380. Bookshelf ID: NBK425165. Archived from the original on 26 October 2020. Retrieved 6 February 2020.
- Swen JJ, Nijenhuis M, de Boer A, Grandia L, Maitland-van der Zee AH, Mulder H, Rongen GA, van Schaik RH, Schalekamp T, Touw DJ, van der Weide J, Wilffert B, Deneer VH, Guchelaar HJ (2011). "Pharmacogenetics: from bench to byte—an update of guidelines". Clinical Pharmacology & Therapeutics. 89 (5): 662–73. doi:10.1038/clpt.2011.34. PMID 21412232. S2CID 2475005.
- The Pharmaceutical Codex. 1994. Principles and practice of pharmaceutics, 12th edn. Pharmaceutical press
- Hansch C, Leo A, Hoekman D. 1995. Exploring QSAR.Hydrophobic, electronic and steric constants. Washington, DC: American Chemical Society.
- Box KJ, Völgyi G, Baka E, Stuart M, Takács-Novák K, Comer JE (June 2006). "Equilibrium versus kinetic measurements of aqueous solubility, and the ability of compounds to supersaturate in solution--a validation study". J Pharm Sci. 95 (6): 1298–307. doi:10.1002/jps.20613. PMID 16552741.
- Healy D (1997). The Antidepressant Era. Harvard University Press. pp. 74–76. ISBN 0674039572.
- Healy D (1999). The Psychopharmacologists II. Arnold. pp. 565–566. ISBN 1860360106.
- Brown, M., "Nick Drake: the fragile genius" Archived 11 March 2018 at the Wayback Machine, The Daily Telegraph, 25 November 2014.
- "Swaziland King Mswati's Eighth Wife, Senteni Masango Commits Suicide". parentsafrica.com; Parents Magazine. 8 April 2018. Archived from the original on 28 August 2021. Retrieved 28 August 2021.
- Press J (10 January 2021). "The Sopranos Fan's Guide to The Many Saints of Newark". Vanity Fair. Archived from the original on 1 October 2021. Retrieved 10 January 2021.
Livia is already troubled enough in the yesteryear of Many Saints that her doctor wants to prescribe her the antidepressant Elavil, but she rejects it. "I'm not a drug addict!" she sneers. Tony pores over the Elavil pamphlet with great interest and even schemes with Dickie Moltisanti to get his suffering mother to take it: "It could make her happy."
- Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 889–. ISBN 978-1-4757-2085-3. Archived from the original on 8 September 2017.
- Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 48–. ISBN 978-3-88763-075-1.
- Morton IK, Hall JM (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 15–. ISBN 978-94-011-4439-1. Archived from the original on 15 February 2017.
- "Amitriptyline". Drugs.com. Archived from the original on 13 August 2017. Retrieved 13 August 2017.
- Jack RH, Hollis C, Coupland C, Morriss R, Knaggs RD, Butler D, et al. (July 2020). Hellner C (ed.). "Incidence and prevalence of primary care antidepressant prescribing in children and young people in England, 1998-2017: A population-based cohort study". PLoS Medicine. 17 (7): e1003215. doi:10.1371/journal.pmed.1003215. PMC 7375537. PMID 32697803.
- Flament MF, Bissada H, Spettigue W (March 2012). "Evidence-based pharmacotherapy of eating disorders". International Journal of Neuropsychopharmacology. 15 (2): 189–207. doi:10.1017/S1461145711000381. PMID 21414249.
Further reading
- Dean L (March 2017). "Amitriptyline Therapy and CYP2D6 and CYP2C19 Genotype". In Pratt VM, McLeod HL, Rubinstein WS, et al. (eds.). Medical Genetics Summaries. National Center for Biotechnology Information (NCBI). PMID 28520380.