Alcohol and cancer

Alcoholic beverages were classified as a Group 1 carcinogen by the International Agency for Research on Cancer (IARC) in 1988 and are attributed to 740,000 cases of cancer in 2020 or 4.1% of new cancer cases.[1][2] Heavy drinking consisting of 15 or more drinks per week for men or 8 or more drinks per week for women beverages/week contributed the most to cancer incident compared with moderate drinking. The rate of alcohol related cases is 3:1 in males compared with females, especially in oesophageal, and liver cancers.[1] Breast cancer is also related to alcohol consumption in women.[1] IARC additionally classifies alcoholic beverage consumption as a cause of oesophagus, liver, female breast, colon, oral cavity, rectum, pharynx and laryngeal cancers and as a probable cause of pancreatic cancer.[2]
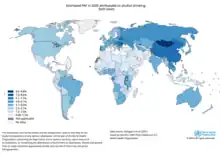
3.6% of all cancer cases and 3.5% of cancer deaths worldwide are attributable to consumption of alcohol (specifically, acetaldehyde a derivative of ethanol).[3]
Alcohol is thought to cause cancer through three main mechanisms:
- DNA methylation[3]
- Oxidative stress
- Hormonal alteration
as well as secondary mechanisms of Liver cirrhosis, Microbiome Dysbiosis, reduced immune system function, Retinoid metabolism, Increased levels of inflammation, 1-Carbon metabolism and disruption of folate absorption.[4]
Some nations have introduced alcohol packaging warning messages that inform consumers about alcohol and cancer.
The alcohol industry has tried to actively mislead the public about the risk of cancer due to alcohol consumption, in addition to campaigning to remove laws that require alcoholic beverages to have cancer warning labels.
Epidemiology of alcohol-related cancers
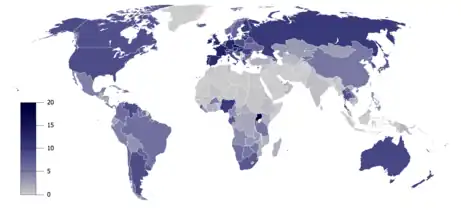
Global Prevalence of Cancer Diagnoses Attributed to Alcohol Consumption
In 2020, approximately 740,000 cases of alcohol-related cancers were identified globally[6][7] with
- 58% of cases (430,000) residing in Asia
- 25% of cases (180,000) residing in Europe
- 8% of cases (60,000) residing in North America
- 5% of cases (39,000) residing in Latin America and the Caribbean
- 3% of cases (23,000) residing in Africa
- 1% of cases (7,000) residing in regions termed "other."
More than three-quarters of the 740,000 cases were in men.[8]
United States
In the United States of America, alcohol-related cancer rates were highest in the following states: Delaware, Colorado, the Washington, D.C., New Hampshire, and Alaska.[9] Conversely, alcohol-related cancer rates were lowest in the following states: Kentucky, Arizona, Oklahoma, West Virginia, and Utah.[9]
From 2013 to 2016, approximately 19,000 (4%) cancer-related deaths in the United States were attributed to alcohol consumption each year, with breast cancer and esophageal cancer deaths being the most common in women and men respectively.[10][11]
An estimated 3.2% of cancer deaths in United States were attributed to alcohol consumption. The distribution of mortality by state were consistent with the distribution of incident cases.[9]
Europe
Approximately 10% and 3% of cancer diagnoses in European men and women respectively are attributed to alcohol consumption.[12]
Europe: A 2011 study found that one in 10 of all cancers in men and one in 33 in women were caused by past or current alcohol intake.[13][14]
Australia
Australia: A 2009 study found that 2,100 Australians die from alcohol-related cancer each year.[15]
Alcohol as a carcinogen and cocarcinogen
The International Agency for Research on Cancer (Centre International de Recherche sur le Cancer) of the World Health Organization has classified alcohol as a Group 1 carcinogen, similar to arsenic, benzene, and asbestos. Its evaluation states, "There is sufficient evidence for the carcinogenicity of alcoholic beverages in humans. …Alcoholic beverages are carcinogenic to humans (Group 1)."[16] After more epidemiological evidence connecting alcohol and cancers became available the IARC reconvened in 2007. Based on epidemiological studies which revealed cancer risk was independent of the type of alcohol and animal studies which showed increased cancer risk with exposure to ethanol alone, the group determined that the ethanol in alcoholic beverages was carcinogenic to humans. Alcohol was determined to increase the risk of developing breast cancer, liver cancer, colorectal cancer, esophageal cancers, pharyngeal cancer, laryngeal cancer, and oral cancer. In 2009, the group determined that acetaldehyde which is a metabolite of ethanol is also carcinogenic to humans.[17] As of 2021, the 15th report of the US National Toxicology Program (NTP) classifies the consumption of alcoholic beverages as "known to be a human carcinogen" while acetaldehyde is classified as "reasonably anticipated to be a human carcinogen".[18]
Mechanisms
Acetaldehyde
Acetaldehyde is a byproduct of ethanol breakdown in the liver, metabolized by Alcohol dehydrogenase (ADH), Cytochrome P-450 2E1 and bacterial catalases.[4][19] The liver then normally eliminates 99% of the acetaldehyde. ALDH2 converts Acetaldehyde into acetate which is a byproduct that can be excreted through the liver. Those with ADH1B*1 have higher rates of conversion of ethanol into Acetaldehyde while, people with ALDH2*2 have a slower conversion rate of acetaldehyde to acetate causing faster build up of acetaldehyde concentrations.[20] 28-45% of east asian populations carry the ALDH2*2 allele.[4] An average liver can process 7 grams of ethanol per hour. For example, it takes 12 hours to eliminate the ethanol in a bottle of wine, giving 12 hours or more of acetaldehyde exposure.
The Acetaldehyde motif can bind DNA to alter its physical shape or block repair and synthesis mechanisms to induce mutations, breaks and exchanges .[4][20] Acetaldehyde and Ethanol both inhibit S-adenosyl-L-methiodine (SAMe) synthesis which is a methyl group transferase.[21]
DNA Methylation
DNA Methylation is the addition of a methyl group to the carbon-5 of nucleotides. the most common methylation site is onto a cystine preceding guanine nucleotides.[21] This methylation is catalyzed by DNA methyltransferase enzymes taking a methyl group from SAMe. Heavy alcohol consumption is thought to cause epigenetic changes by decreasing the availability of SAMe thereby changing the methylation pattern of DNA causing hypo or hypermethylation resulting in alteration of DNA transcription.[21]
Oxidative Stress
Oxidative stress and ROS accumulation is a major player in cancer growth. the metabolism of ethanol by CYP450 2E1 into acetaldehyde has a byproduct of ROS. The presence of ROS in the cellular environment causes lipid peroxidation which can lead to exocyclic adducts.[20] ROS in a tumor microenvironment can also act as an intercellular signal leading to up-regulation of vascular endothelial growth factors and monocyte chemotactic protein-1.[20] The accumulation of iron is also found to correlate to alcohol consumption which leads to higher levels of peroxidation and resulting oxidative damage.[22]
Hormonal regulation
High levels of hormones in serum have been associated with heavy alcohol use. Especially Oesterogen and estradiol which can increase transcriptional activity in ER+ cells which promote cell proliferation.[23][4][24] Those in pre-menopause using progestin contraceptives have some compensation for the high levels of estradiol, though after menopause those with heavy alcohol consumption have higher risk for breast cancer and estrogen dependent cancers.[24][22]
Other mechanisms
Additional mechanisms contribute to cancer risk with alcohol consumption. It is thought that heavy alcohol consumption can cause a decrease in folic acid availability which can decrease the availability of nucleotides for DNA repair.[21] Additionally ethanol can decrease the conversion of homocysteine to methionine which is an essential amino acid that is part of the formation of SAMe.[21][22]
Increased inflammation due to alcohol consumption can increase various cytokine formations especially NF-κB which is a transcription factor.[4]
Additionally Alcohol usage is associated with lower Vitamin A levels which causes a reduction in retinoid conversion and signaling.[4][19][22]
Individuals who both smoke and drink are at a much higher risk of developing mouth, tracheal, and esophageal cancer. Ethanol is thought to potentially be a solvent for carcinogenic factors in smoking.[23] Research has shown their risk of developing these cancers is 35 times higher than in individuals who neither smoke nor drink. This evidence may suggest that there is a cocarcinogenic interaction between alcohol and tobacco-related carcinogens.[25][26]
Individuals who both smoke and drink are at a much higher risk of developing mouth, tracheal, and esophageal cancer. Ethanol is thought to potentially be a solvent for carcinogenic factors in smoking.[23] Research has shown their risk of developing these cancers is 35 times higher than in individuals who neither smoke nor drink. This evidence may suggest that there is a cocarcinogenic interaction between alcohol and tobacco-related carcinogens.[25][26]
Local carcinogenic effect of ethanol
The risk of cancer associated with alcohol consumption is higher in tissues in closest contact on ingestion of alcohol, such as the oral cavity, pharynx and esophagus. This is explained by the fact that ethanol is a proven mutagen and in addition, metabolite of ethanol (acetaldehyde) produced in the liver is highly carcinogenic, thus explaining both local (mouth, throat, esophageal cancers) as well as distant (skin, liver, breast) cancers. It is well known that ethanol causes cell death at the concentrations present in alcoholic beverages. Few cells survive a one-hour exposure to 5–10% ethanol or a 15-second exposure to 30–40% ethanol in cell culture, where surviving cells might undergo genomic changes leading to carcinogenesis. But recent evidence suggests that the cytotoxic effect of ethanol on the cells lining the oral cavity, pharynx and esophagus activates the division of the stem cells located in deeper layers of the mucosa to replace the dead cells. Every time stem cells divide, they become exposed to unavoidable errors associated with cell division (e.g., mutations arising during DNA replication and chromosomal alterations occurring during mitosis) and also become highly vulnerable to the genotoxic activity of DNA-damaging agents (e.g., acetaldehyde and tobacco carcinogens). Alcohol consumption probably increases the risk of developing cancer of the oral cavity, pharynx and esophagus by promoting the accumulation of cell divisions in the stem cells that maintain these tissues in homeostasis. Because the cytotoxic activity of ethanol is concentration-dependent, the risk of these cancers will not only increase with increasing amounts of ethanol, but also with increasing concentrations; an ounce of whisky is probably more carcinogenic when taken undiluted than when taken mixed with non-alcoholic beverages. The local cytotoxic effect of ethanol may also explain the known synergistic effect of alcohol and tobacco use on the risk of these cancers.[27]
Epithelial-mesenchymal transition
A study found that alcohol stimulates the epithelial-mesenchymal transition (EMT), in which ordinary cancer cells change into a more aggressive form and begin to spread throughout the body.[28][29]
Effect of alcohol on the progress of cancer when established
A study of the influence of alcohol intake on tumor growth of hepatocellular carcinoma (HCC) in patients with type C cirrhosis, found that alcohol influenced tumor volume doubling time (TVDT).[30]
A study of chick embryos suggests that alcohol stimulates their tumor growth by fueling the production of a growth factor that stimulates blood vessel development in tumors.[31] A 2006 study in mice showed moderate drinking resulted in larger and stronger tumors via a process known as angiogenesis.[32][33]
A study where high amounts of alcohol were given to mice suggests that it accelerates their cancer growth by speeding up the loss of body fat and depressing immune activity.[34]
Genetic variation and cancer risk
Since acetaldehyde produced from the metabolism of alcohol plays a role in the carcinogenicity induced by alcohol consumption, mutations in the enzymes involved in the production of acetaldehyde can lead to increased cancer risk. These enzymes included Cytochrome P450 2E1 and alcohol dehydrogenase.[35] A study found that "the ADH1C*1 allele and genotype ADH1C*1/1 were significantly more frequent in patients with alcohol-related cancers…"[36] A European study has found two gene variants which offer "significant" protection against mouth and throat cancers.[37] Alcohol is a known porphyrinogenic chemical. Several European studies have linked the inherited hepatic porphyrias with a predisposition to hepatocellular carcinoma. Typical risk factors for HCC need not be present with the acute hepatic porphyrias, specifically acute intermittent porphyria, variegate porphyria and hereditary coproporphyria. Porphyria cutanea tarda is also associated with HCC, but with typical risk factors including evidence of hepatotropic viruses, hemochromatosis and alcoholic cirrhosis. Tyrosinemia Type I, an inherited disorder in tyrosine metabolism impacting the second enzyme in the heme metabolic pathway is associated with a high risk of developing HCC in younger populations, including children.[38]
Risk factor for specific cancers
Moderate consumption increases risk
A 2022 study from the Seoul National University Hospital, over more than 4.5 million of people, who were screened over 7 years, found that[39]
- those who increased alcohol consumption had a higher cancer risk (including, but not limited to, alcohol-related cancers) than those who kept the same level of alcohol intake;
- the risk increased "regardless of the baseline drinking level"; notably, non-drinkers who became mild or moderate drinkers also had a risk increase.
In the specific case of increasing from no alcohol intake to moderate drinking, "a high incidence of stomach, liver, gallbladder and lung cancer, multiple myeloma and leukemia" was found.[39]
The study also had some limitations. For example, the participants were all registered at the South Korean National Health Insurance Service, but the study did not take into account alcohol metabolism diseases which are commonly found in East Asia.[39] The participants were not younger than 40.[39] No data was available to account for positive lifestyle and behaviors held during the screening, that may have influenced the cancer risk, nor for the participants' drinking habits that preceded the screening.[39]
A prior study found that, "Increasing but moderate alcohol consumption in women was determined to be associated with an increased risk of cancers of the oral cavity and pharynx, esophagus, larynx, rectum, breast, and liver…".[40]
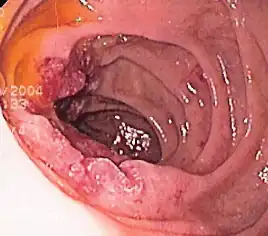
Cancers of the mouth, esophagus, pharynx, and larynx
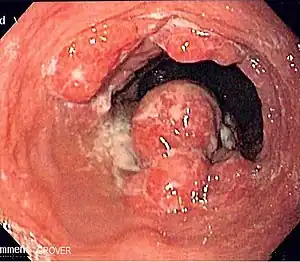
Alcohol consumption at any quantity is a risk factor for cancers of the mouth, esophagus, pharynx and larynx. The U.S. National Cancer Institute states "Drinking alcohol increases the risk of cancers of the mouth, esophagus, pharynx, larynx, and liver in men and women, … In general, risks increases above baseline with any alcohol intake (mild; <2 glass of wine per week) and increases significantly with moderate alcohol intake (one glass of wine per day) with highest risk in those with greater than 7 glasses of wine per week. (A drink is defined as 12 ounces of regular beer, 5 ounces of wine, or 1.5 ounces of 80-proof liquor.) … Also, using alcohol with tobacco is riskier than using either one alone, because it further increases the chances of getting cancers of the mouth, throat, and esophagus."[41] The federal government's Dietary Guidelines for Americans 2010 defines moderate alcohol drinking as up to one drink per day for women and up to two drinks per day for men. Heavy alcohol drinking is defined as having more than three drinks on any day or more than seven drinks per week for women and more than four drinks on any day or more than 14 drinks per week for men.
The International Head and Neck Cancer Epidemiology (INHANCE) Consortium co-ordinated a meta-study on the issue.[42] A study looking at laryngeal cancer and beverage type concluded, "This study thus indicates that in the Italian population characterized by frequent wine consumption, wine is the beverage most strongly related to the risk of laryngeal cancer."[43]
A review of the epidemiological literature published from 1966 to 2006 concluded that:
- The risk of esophageal cancer nearly doubled in the first two years following alcohol cessation, a sharp increase that may be due to the fact that some people only stop drinking when they are already experiencing disease symptoms. However, risk then decreased rapidly and significantly after longer periods of abstention.
- Risk of head and neck cancer only reduced significantly after 10 years of cessation.
- After more than 20 years of alcohol cessation, the risks for both cancers were similar to those seen in people who never drank alcohol.[44][45]
A study concluded that for every additional drink regularly consumed per day, the incidence of oral cavity and pharynx cancers increases by 1 per 1000. The incidence of cancers of the esophagus and larynx increase by 0.7 per 1000.[40]
A 2008 study suggests that acetaldehyde (a breakdown product of alcohol) is implicated in oral cancer.[46][47]
Breast cancer
Alcohol is a risk factor for breast cancer in women.[48][49][50][51][52]
A woman drinking an average of two units of alcohol per day has an 8% higher risk of developing breast cancer than a woman who drinks an average of one unit of alcohol per day.[53] A study concluded that for every additional drink regularly consumed per day, the incidence of breast cancer increases by 11 per 1000.[40] Approximately 6% (between 3.2% and 8.8%) of breast cancers reported in the UK each year could be prevented if drinking was reduced to a very low level (i.e. less than 1 unit/week).[53] Moderate to heavy consumption of alcoholic beverages (at least three to four drinks per week) is associated with a 1.3-fold increased risk of the recurrence of breast cancer. Further, consumption of alcohol at any quantity is associated with significantly increased risk of relapse in breast cancer survivors.[54][55]
Colorectal cancer
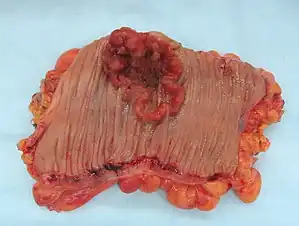
Drinking may be a cause of earlier onset of colorectal cancer.[56] The evidence that alcohol is a cause of bowel cancer is convincing in men and probable in women.[57]
The National Institutes of Health,[58] the National Cancer Institute,[59] Cancer Research,[60] the American Cancer Society,[61] the Mayo Clinic,[62] and the Colorectal Cancer Coalition,[63] American Society of Clinical Oncology[64] and the Memorial Sloan-Kettering Cancer Center[65] list alcohol as a risk factor.
A WCRF panel report finds the evidence "convincing" that alcoholic drinks increase the risk of colorectal cancer in men at consumption levels above 30 grams of absolute alcohol daily.[66] The National Cancer Institute states, "Heavy alcohol use may also increase the risk of colorectal cancer"[67]
A 2011 meta-analysis found that alcohol consumption was associated with an increased risk of colorectal cancer.[68]
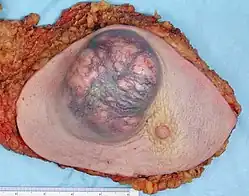
Liver cancer

Alcohol is a risk factor for liver cancer, through cirrhosis.[69][70][71] "Cirrhosis results from scar formation within the liver, most commonly due to chronic alcohol use."[72]
"Approximately 5 percent of people with cirrhosis develop liver cancer. Cirrhosis is a disease that develops when liver cells are replaced with scar tissue after damage from alcohol abuse, …"[73]
The NIAAA reports that "Prolonged, heavy drinking has been associated in many cases with primary liver cancer." However, it is liver cirrhosis, whether caused by alcohol or another factor, that is thought to induce the cancer."[74][75]
"The chances of getting liver cancer increase markedly with five or more drinks per day" (NCI).
A study concluded that for every additional drink regularly consumed per day, the incidence of liver cancer increases by 0.7 per 1000.[40]
In the United States, liver cancer is relatively uncommon, affecting approximately 2 people per 100,000, but excessive alcohol consumption is linked to as many as 36% of these cases by some investigators.[25][76] "Overall, 61% of HCC were attributable to HCV [hepatitis C virus], 13% to HBV [hepatitis B virus], and 18% to heavy alcohol drinking."[77] A study in the province of Brescia, northern Italy concluded, "On the basis of population attributable risks (AR), heavy alcohol intake seems to be the single most relevant cause of HCC in this area (AR: 45%), followed by HCV (AR: 36%), and HBV (AR: 22%) infection."[78]
Lung cancer
Alcohol intake of more than 2 drinks per day is associated with a small increased risk of lung cancer.[79] Commenting on a study by Freudenheim et al., R. Curtis Ellison MD writes, "This study, like others, suggests a weak, positive association between consuming larger amounts of alcohol (>2 drinks a day) and lung cancer risk."[80] However, studies on the relationship between alcohol consumption and lung cancer have yielded conflicting results. Studies are typically impacted by confounding due to factors like smoking which is one of the most significant risk factors for the development of lung cancer. The association of alcohol consumption with lung cancer is unclear.[81]
Skin cancer
Results from the European Prospective Investigation into Cancer and nutrition (EPIC) cohort indicated a positive association between alcohol consumption and skin cancer. Baseline alcohol intake as well as lifetime alcohol consumption were associated with an increased risk of the development of squamous cell carcinoma, basal cell carcinoma, and melanoma in men. There was also an increased risk of these skin cancers in women, but the association wasn't as strong as that seen in men.[82] Any alcohol intake is associated with the development of malignant melanoma.[83]
Stomach cancer
"Statistically significant increases in risk also existed for cancers of the stomach, colon, rectum, liver, female breast, and ovaries."[84]
"While alcohol has been extensively studied as a cause of stomach cancer there is no conclusive evidence that it increases risk. However, results from at least three studies suggest that heavy alcohol consumption may increase the risk of stomach cancer in heavy smokers."[85][86][87][88]
A Taiwanese study concluded, "…cigarette smoking may play the most harmful role in the initial development of gastric cancer, and that drinking alcohol may promote the process."[85]
A Norwegian study found that, "No statistically significant associations between various degrees of exposure to alcohol and risk of gastric cancer was revealed, but combined high use of cigarettes (>20/day) and alcohol (>5 occasions/14 days) increased the risk of noncardia gastric cancer nearly 5-fold (HR = 4.90 [95% CI = 1.90–12.62]), compared to nonusers."[87]
Consumption of 50g or more per day increases risk
Endometrial cancer

Alcohol has been identified as a risk factor for endometrial cancer.[89] Data however, on the association of alcohol intake and endometrial cancer is conflicting. Where data exists for an association low to moderate intake of alcohol, (less than two drinks per day) is not associated with an increased risk but an association has been suggested for higher alcohol intake.[90][91] "Our results suggest that only alcohol consumption equivalent to 2 or more drinks per day increases risk of endometrial cancer in postmenopausal women."[92] "In conclusion, our results suggest that low alcohol consumption (up to one drink per day) is unlikely to substantially influence risk of endometrial cancer."[93]
Gallbladder cancer
Alcohol has been suggested as a risk factor for gallbladder cancer.[94] Evidence suggests that a high intake of alcohol is associated with gallbladder cancer.[95][96] Men may be at a higher risk of alcohol-related gallbladder cancer than women.[97]
Ovarian cancer
"Thus, the results of this study suggest that relatively elevated alcohol intake (of the order of 40 g per day or more) may cause a modest increase of epithelial ovarian cancer risk.".[98] "Associations were also found between alcohol consumption and cancers of the ovary and prostate, but only for 50 g and 100 g a day."[99] "Statistically significant increases in risk also existed for cancers of the stomach, colon, rectum, liver, female breast, and ovaries."[84]
"Thus, this pooled analysis does not provide support for an association between moderate alcohol intake and ovarian cancer risk."[100]
Prostate cancer
"Data from the Health Professionals Follow-Up Study showed only a weak association between overall alcohol intake and prostate cancer risk, and no association at all between red wine intake and prostate cancer risk."[101]
A meta-analysis published in 2001 found a small but significant increased risk for men drinking more than 50 g/day of alcohol, with a slightly higher risk for men consuming more than 100 g/day.[102] Since that analysis, cohort studies in America have found increased risks for men drinking moderate amounts of spirits, and for 'binge drinkers,[103] but moderate consumption of beer or wine has not been linked to an increased risk.[104][105][106]
Alcohol consumption of 50 g and 100 g per day is also associated with cancers of the ovary and prostate.[99] However, one study concludes, that moderate alcohol consumption increases the risk of prostate cancer. Liquor, but not wine or beer, consumption was positively associated with prostate cancer."[104]
The Fred Hutchinson Cancer Research Center found that men who consumed four or more glasses of red wine per week had a 50 percent reduction in the risk of developing prostate cancer. They "found no significant effects – positive nor negative – associated with the consumption of beer or hard liquor and no consistent risk reduction with white wine, which suggests that there must be a beneficial compound in red wine that other types of alcohol lack. That compound … may be an antioxidant called resveratrol, which is abundant in the skins of red grapes.".[105][107]
A meta analysis of studies published in 2009 found that consumption of only 2 standard drinks per day increased the cancer risk by 20%.[108][109]
Small intestine cancer
A study of small intestine cancer patients reported that alcohol consumption was associated with adenocarcinomas and malignant carcinoid tumors.[110]
"In men and women combined, a significant 3-fold increased risk in heavy drinkers (80+g ethanol/day) relative to more moderate drinkers and non-drinkers was observed."[111]
"Alcohol and tobacco consumption did not increase the risk of adenocarcinoma of the small intestine. … While the present data are inconsistent with a major effect of tobacco or alcohol, a moderate association between these factors and small bowel cancer may have been obscured by the play of chance."[112]
Evidence is mixed
Leukemia
Intake of alcohol during pregnancy has been associated with childhood leukemia.[113] A review published by the National Cancer Institute placed maternal alcohol consumption during pregnancy in the category of "suggestive" but concluded that the risk was not important.[114]
- Acute Lymphocytic Leukemia (ALL)
For ALL in children, maternal alcohol consumption during pregnancy is "unlikely to be an important risk factor for ALL"[114]
- Acute myeloid leukemia (AML)
A study concluded, "In conclusion, even though our study did not show a clear association between alcohol intake and leukemia risk, some of the patterns of the risk estimates (a possible J-shaped dose-response curve between alcohol intake and ALL, AML, and CLL risks, and the positive association between alcohol and CML), may be suggestive."[115]
- Childhood AML
"Three studies have reported an increased risk (approximately 1.5-2 fold) in mothers who drank alcoholic beverages during pregnancy. These associations have been particularly apparent in children diagnosed younger than three years of age.".[114] "Maternal alcohol consumption during pregnancy increases the risk of infant leukemia, especially AML."[116]
- Acute non-lymphocytic leukemia (ANLL)
A study found that intrauterine exposure to alcohol doubled the risk for childhood ANLL.[117]
- Chronic Lymphocytic Leukemia (CLL)
A study concluded, "In conclusion, even though our study did not show a clear association between alcohol intake and leukemia risk, some of the patterns of the risk estimates (a possible J-shaped dose-response curve between alcohol intake and ALL, AML, and CLL risks, and the positive association between alcohol and CML), may be suggestive."[115]
- Chronic myeloid leukemia (CML)
A population-based case-control study in Italy found a non-significant positive association between drinking and CML.[115]
- Hairy cell leukemia
A study concluded, "There was no association found for cigarette smoking, alcohol or coffee consumption and hairy cell leukemia."[118]
Multiple myeloma (MM)
Alcohol has been suggested as a possible cause of multiple myeloma,[119] although a study found no association between MM in a comparison study between drinkers and non-drinkers.[120]
Pancreatic cancer
Whilst the association between alcohol abuse and pancreatitis is well established the association between alcohol consumption and pancreatic cancer is less clear. Overall the evidence suggests a slightly increased risk of pancreatic cancer with chronic heavy alcohol consumption but the evidence remains conflicting with a number of studies finding no association.,[121][122] but no increased risk for people consuming up to 30g of alcohol a day[123]
Overall, the association is consistently weak and the majority of studies have found no association.[25][123][124] Although drinking alcohol excessively is a major cause of chronic pancreatitis, which in turn predisposes to pancreatic cancer, chronic pancreatitis associated with alcohol consumption is less frequently a precursor for pancreatic cancer than other types of chronic pancreatitis.[125]
Some studies suggest a relationship,[126] the risk increasing with increasing amount of alcohol intake.[127][128] The risk is greatest in heavy drinkers,[121][122][129] mostly on the order of four or more drinks per day.[130] There appears to be no increased risk for people consuming up to 30g of alcohol a day,[123][131][132] which is approximately 2 alcoholic beverages/day,[132] so most people who take alcohol do so at a level that "is probably not a risk factor for pancreatic cancer".[122] A pooled analysis concluded, "Our findings are consistent with a modest increase in risk of pancreatic cancer with consumption of 30 or more grams of alcohol per day".[132]
Several studies caution that their findings could be due to confounding factors.[121][133] Even if a link exists, it "could be due to the contents of some alcoholic beverages"[134] other than the alcohol itself. One Dutch study even found that drinkers of white wine had lower risk.[135]
"About 7 out of 10 cases of chronic pancreatitis are due to long term heavy drinking. Chronic pancreatitis is a known risk factor for cancer of the pancreas. But chronic pancreatitis that is due to alcohol doesn't increase risk as much as other types of chronic pancreatitis. So if there is a link with alcohol and pancreatic cancer risk, it is only very slight."[125]
"Our findings indicate that alcohol drinking at the levels typically consumed by the general population of the United States is probably not a risk factor for pancreatic cancer. Our data suggest, however, that heavy alcohol drinking may be related to pancreatic cancer risk."[122]
"Relative risks of pancreatic cancer increased with the amount of alcohol consumed (Ptrend = 0.11) after adjustment for age, smoking status, and pack-years of smoking."[136]
"Alcoholics had only a modest 40% excess risk of pancreatic cancer … The excess risk for pancreatic cancer among alcoholics is small and could conceivably be attributed to confounding by smoking."[121]
"It was shown that the relative risk of cancer of the pancreas increases with fat and alcohol intakes, … Alcohol may be not directly involved in the aetiology of cancer of the pancreas: its effect could be due to the contents of some alcoholic beverages."[137]
"When compared with data from non-drinkers, the cumulative lifetime consumption of all types of alcohol in grams of ethanol… beer, spirits, red wine and fortified wine was not related to risk. The consumption of white wine was inversely associated with risk…. The uniformly reduced risk estimates for the lifetime number of drinks of white wine were based on small numbers…."[138]
"For the most part, consumption of total alcohol, wine, liquor and beer was not associated with pancreatic cancer."[139]
"Data from these two large cohorts do not support any overall association between coffee intake or alcohol intake and risk of pancreatic cancer."[123]
"Our findings are consistent with a modest increase in risk of pancreatic cancer with consumption of 30 or more grams of alcohol per day."[140]
Not suspected to increase risk
This section lists cancers where alcohol is not listed as a risk factor and where papers have been published.
Childhood astrocytoma
A study concluded that foetal exposure to alcohol is not associated with childhood astrocytoma.[141]
Bile duct cancer
A review of the literature found that there is no association between alcohol use and bile duct cancer.[142]
Bladder cancer
"Epidemiological data on alcohol drinking and bladder cancer are suggestive of no association, although findings were not always consistent. For both habits, an explanation of the moderate increase in risk observed in some investigations might be attributed to residual confounding by smoking, or to an association between alcohol, coffee, and yet unidentified risk factors for bladder cancer."[143]
Cervical cancer
A study concluded "that alcoholic women are at high risk for in situ and invasive cervical cancer" but attributed this to indirect, lifestyle-related reasons.[144]
Ductal carcinoma in situ (DCIS) breast cancer
"DCIS patients and control subjects did not differ with respect to oral contraceptive use, hormone replacement therapy, alcohol consumption or smoking history, or breast self-examination. Associations for LCIS were similar."[145]
Ependymoma
A review of the basic literature[146] found that consumption of beer was associated with increased risk in one study[147] but not in another[148]
Intraocular and uveal melanomas
A study found no association between alcohol and uveal melanoma.[149]
Nasopharynageal cancer / Nasopharyngeal carcinoma (NPC)
A systematic review found evidence that light drinking may decrease the risk of nasopharyngeal carcinoma whereas high intake of alcohol may increase the risk.[150]
Neuroblastoma
A few studies have indicated an increased risk of neuroblastoma with use of alcohol during pregnancy.[151]
Salivary gland cancer (SGC)
Alcohol use is associated with an increased risk of salivary gland cancer.[152]
Testicular cancer
A review concluded that "There is no firm evidence of a causal relation between behavior risks [tobacco, alcohol and diet] and testicular cancer."[153]
Thyroid cancer
A 2009 review found that alcohol intake does not affect the risk of developing thyroid cancer.[154] However, a 2009 study of 490,000 men and women concluded that alcohol may reduce the risk of thyroid cancer.[155] A 2009 study of 1,280,296 women in the United Kingdom concluded, "The decreased risk for thyroid cancer that we find to be associated with alcohol intake is consistent with results from some studies, although a meta-analysis of 10 case–control studies and two other cohort studies reported no statistically significant associations."[156]
Vaginal cancer
A Danish study found that "Abstinence from alcohol consumption was associated with low risk for both VV-SCCvagina and VV-SCCvulva in our study."[157]
A study concluded that alcoholic women are at high risk for cancer of the vagina.[144] In both studies, indirect, lifestyle-related reasons were cited.
Vulvar cancer
One study reported "No consistent association emerged between milk, meat, liver, alcohol and coffee consumption and risk of vulvar cancer."[158] A Danish study found the reverse, that alcohol consumption is significantly associated with VV-SCCvagina and VV-SCCvulva cancer.[157] A Swedish study concluded that alcoholic women are at no higher risk for cancer of the vulva.[144]
Might reduce risk
Hodgkin's lymphoma (HL)
A study concluded, "The results of this large-scale European study … suggested a protective effect of alcohol on development of NHL for men and in non-Mediterranean countries."[159] A population based case-control study in Germany found that alcohol reduced the risk of HL for both men and women but more so for men, whose risk was lowered by 53%.[160]
A population-based case-control study in Italy reported a protective effect of alcohol consumption on risk of HL among non-smokers.[120] Analysis of data from a series of case-control studies in Northern Italy revealed a modest positive effect of alcohol on lowering risk of HL among both smokers and non-smokers.[161]
A study considering more than 1 million American women found that increasing levels of alcohol consumption were associated with a decreased risk of Hodgkin's Lymphoma.[40]
Kidney cancer (Renal cell carcinoma) (RCC)
"Moderate alcohol consumption was associated with a lower risk of renal cell cancer among both women and men in this pooled analysis"[162] "This pooled analysis found an inverse association between alcohol drinking and RCC. Risks continued to decrease even above eight drinks per day (i.e. >100 g/day) of alcohol intake, with no apparent levelling in risk."[163]
A study concluded, "Results from our prospective cohort study of middle-aged and elderly women indicate that moderate alcohol consumption may be associated with decreased risk of RCC."[164] Researchers who conducted a study in Iowa reported that "In this population-based case-control investigation, we report further evidence that alcohol consumption decreases the risk of RCC among women but not among men. Our ability to show that the association remains after multivariate adjustment for several new confounding factors (i.e., diet, physical activity, and family history) strengthens support for a true association.[165]
Another study found no relationship between alcohol consumption and risk of kidney cancer among either men or women.[166]
A Finnish study concluded, "These data suggest that alcohol consumption is associated with decreased risk of RCC in male smokers. Because most of the risk reductions were seen at the highest quartile of alcohol intake and alcohol is a risk factor for a number of cancers particularly among smokers, these data should be interpreted with caution."[167] "Our data suggest an inverse association between alcohol intake and risk of renal cell cancer…"[168] Compared with nondrinkers, men who drank one or more drinks per day had a 31% lower risk of kidney cancer among 161,126 Hawaii-Los Angeles Multiethnic Cohort participants.[169]
A study considering more than 1 million American women found that increasing levels of alcohol consumption were associated with a decreased risk of renal cancer.[40]
Non-Hodgkin lymphoma (NHL)
A study concluded, "People who drink alcoholic beverages might have a lower risk of NHL than those who do not, and this risk might vary by NHL subtype."[170] "Compared with nondrinkers, alcohol consumers had a lower risk for non-Hodgkin's lymphoma overall … and for its main subtypes."[171] A study concluded, "Nonusers of alcohol had an elevated NHL risk compared with users…"[172]
Some studies have found a protective effect on NHL of drinking some forms of alcoholic beverage or in some demographic groups. A study of men in the US found that consumption of wine, but not beer or spirits, was associated with a reduced NHL risk[173] and a large European study found a protective effect of alcohol among men and in non-Mediterranean countries.."[174] A study of older women in Iowa found alcohol to reduce the risk of NHL and the amount of alcohol consumed, rather than the type of alcoholic beverages, appeared to be the main determinant in reducing risk."[175] A possible mechanism has been suggested.[176]
Some studies have not found a protective effect from drinking. British research found no association between frequency of drinking and NHL[177] and research in Sweden found that total beer, wine, or liquor intake was not associated with any major subtype of NHL examined, apart from an association between high wine consumption and increased risk of chronic lymphocytic leukemia.."[178]
One study of NHL patients concluded, "Our findings strongly encourage physicians to advise NHL patients to stop smoking and diminish alcohol consumption to obtain improvements in the course of NHL."[179]
A study considering more than 1 million American women found that increasing levels of alcohol consumption were associated with a decreased risk of non-Hodgkin lymphoma.[40]
Recommended maximum alcohol intake
As outlined above, there is no recommended alcohol intake with respect to cancer risk alone as it varies with each individual cancer. See Recommended maximum intake of alcoholic beverages for a list of governments' guidances on alcohol intake which, for a healthy man, range from 140–280g per week.
One meta-analysis suggests that risks of cancers may start below the recommended levels. "Risk increased significantly for drinkers, compared with non-drinkers, beginning at an intake of 25 g (< 2 standard drinks) per day for the following: cancers of the oral cavity and pharynx (relative risk, RR, 1.9), esophagus (RR 1.4), larynx (RR 1.4), breast (RR 1.3), liver (RR 1.2), colon (RR 1.1), and rectum (RR 1.1)"[180][181]
World Cancer Research Fund recommends that people aim to limit consumption to less than two drinks a day for a man and less than one drink a day for a woman. It defines a "drink" as containing about 10–15 grams of ethanol.[182]
Alcohol industry manipulation of the science on alcohol and cancer
A study published in 2017 has found that front organisations set up by the world's leading alcohol companies are actively misleading the public about the risk of cancer due to alcohol consumption. The study drew parallels with the long-standing activities of the tobacco industry. It also claimed that there was a particular focus on misleading women drinkers, because much of the misinformation about cancer produced by these companies was found to be focused on breast cancer.[183]
The alcohol industry around the world has also campaigned to remove laws that require alcoholic beverages to have cancer warning labels.[184]
A 2019 survey conducted by the American Institute for Cancer Research (AICR) showed that only 45% of Americans were aware of the associated risk of cancer due to alcohol consumption, up from 39% in 2017.[185] The AICR believes that alcohol-related advertisements about the healthy cardiovascular benefits of modest alcohol overshadow messages about the increased cancer risks.[185]
References
- 1 2 3 Rumgay, Harriet; Shield, Kevin; Charvat, Hadrien; Ferrari, Pietro; Sornpaisarn, Bundit; Obot, Isidore; Islami, Farhad; Lemmens, Valery E. P. P.; Rehm, Jürgen; Soerjomataram, Isabelle (1 August 2021). "Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study". The Lancet Oncology. 22 (8): 1071–1080. doi:10.1016/S1470-2045(21)00279-5. ISSN 1470-2045. PMC 8324483. PMID 34270924.
- 1 2 "IARC: Home". www.iarc.who.int. Archived from the original on 25 September 2022. Retrieved 12 September 2022.
- 1 2 Varela-Rey, Marta; Woodhoo, Ashwin; Martinez-Chantar, Maria-Luz; Mato, José M.; Lu, Shelly C. (2013). "Alcohol, DNA methylation, and cancer". Alcohol Research: Current Reviews. 35 (1): 25–35. ISSN 2168-3492. PMC 3860423. PMID 24313162.
- 1 2 3 4 5 6 7 Rumgay, Harriet; Murphy, Neil; Ferrari, Pietro; Soerjomataram, Isabelle (2021). "Alcohol and Cancer: Epidemiology and Biological Mechanisms". Nutrients. 13 (9): 3173. doi:10.3390/nu13093173. ISSN 2072-6643. PMC 8470184. PMID 34579050.
- ↑ Global Status Report on Alcohol 2004 (PDF). Geneva: World Health Organization. 2004. pp. 11–12. ISBN 978-92-4-156272-0.
- ↑ Rumgay, Harriet; Shield, Kevin; Charvat, Hadrien; Ferrari, Pietro; Sornpaisarn, Bundit; Obot, Isidore; Islami, Farhad; Lemmens, Valery E. P. P.; Rehm, Jürgen; Soerjomataram, Isabelle (1 August 2021). "Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study". The Lancet Oncology. 22 (8): 1071–1080. doi:10.1016/S1470-2045(21)00279-5. ISSN 1470-2045. PMC 8324483. PMID 34270924.
- ↑ "Cancer and Alcohol". gco.iarc.fr. Archived from the original on 23 September 2022. Retrieved 14 September 2022.
- ↑ "Report Details Alcohol's Global Cancer Burden - NCI". www.cancer.gov. 12 August 2021. Archived from the original on 14 September 2022. Retrieved 14 September 2022.
- 1 2 3 Goding Sauer, Ann; Fedewa, Stacey A.; Bandi, Priti; Minihan, Adair K.; Stoklosa, Michal; Drope, Jeffrey; Gapstur, Susan M.; Jemal, Ahmedin; Islami, Farhad (1 April 2021). "Proportion of cancer cases and deaths attributable to alcohol consumption by US state, 2013-2016". Cancer Epidemiology. 71 (Pt A): 101893. doi:10.1016/j.canep.2021.101893. ISSN 1877-7821. PMID 33477084. S2CID 231680583.
- ↑ Goding Sauer, Ann; Fedewa, Stacey A.; Bandi, Priti; Minihan, Adair K.; Stoklosa, Michal; Drope, Jeffrey; Gapstur, Susan M.; Jemal, Ahmedin; Islami, Farhad (1 April 2021). "Proportion of cancer cases and deaths attributable to alcohol consumption by US state, 2013-2016". Cancer Epidemiology. 71 (Pt A): 101893. doi:10.1016/j.canep.2021.101893. ISSN 1877-7821. PMID 33477084. S2CID 231680583.
- ↑ Nelson, David E.; Jarman, Dwayne W.; Rehm, Jürgen; Greenfield, Thomas K.; Rey, Grégoire; Kerr, William C.; Miller, Paige; Shield, Kevin D.; Ye, Yu; Naimi, Timothy S. (April 2013). "Alcohol-Attributable Cancer Deaths and Years of Potential Life Lost in the United States". American Journal of Public Health. 103 (4): 641–648. doi:10.2105/AJPH.2012.301199. ISSN 0090-0036. PMC 3673233. PMID 23409916.
- ↑ Scoccianti, Chiara; Cecchini, Michele; Anderson, Annie S.; Berrino, Franco; Boutron-Ruault, Marie-Christine; Espina, Carolina; Key, Timothy J.; Leitzmann, Michael; Norat, Teresa; Powers, Hilary; Wiseman, Martin; Romieu, Isabelle (1 December 2016). "European Code against Cancer 4th Edition: Alcohol drinking and cancer". Cancer Epidemiology. 45: 181–188. doi:10.1016/j.canep.2016.09.011. ISSN 1877-7821. PMID 27816465. Archived from the original on 14 September 2022. Retrieved 25 September 2022.
- ↑ Drinking over recommended limit 'raises cancer risk' Archived 17 May 2011 at the Wayback Machine. BBC. 8 April 2011
- ↑ Schutze, M.; Boeing, H.; Pischon, T.; Rehm, J.; Kehoe, T.; Gmel, G.; Olsen, A.; Tjonneland, A. M.; Dahm, C. C.; Overvad, K.; Clavel-Chapelon, F.; Boutron-Ruault, M.-C.; Trichopoulou, A.; Benetou, V.; Zylis, D.; Kaaks, R.; Rohrmann, S.; Palli, D.; Berrino, F.; Tumino, R.; Vineis, P.; Rodriguez, L.; Agudo, A.; Sanchez, M.-J.; Dorronsoro, M.; Chirlaque, M.-D.; Barricarte, A.; Peeters, P. H.; Van Gils, C. H.; et al. (2011). "Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study". BMJ. 342: d1584. doi:10.1136/bmj.d1584. PMC 3072472. PMID 21474525.
- ↑ Study bolsters alcohol-cancer link Archived 23 November 2010 at the Wayback Machine ABC News 24 August 2009
- ↑ Alcohol drinking. Lyon: World Health Organization, International Agency for Research on Cancer. 1988. ISBN 978-92-832-1244-7. p8
- ↑ Brooks, Philip J. (2011), Zakhari, Samir; Vasiliou, Vasilis; Guo, Q. Max (eds.), "Alcohol as a Human Carcinogen", Alcohol and Cancer, New York, NY: Springer New York, pp. 1–4, doi:10.1007/978-1-4614-0040-0_1, ISBN 978-1-4614-0039-4, archived from the original on 29 September 2022, retrieved 12 September 2022
- ↑ National Toxicology Program (NTP). "15th Report on Carcinogens". doi:10.22427/ntp-other-1003. S2CID 245412518.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Pöschl G, Seitz HK (2004). "Alcohol and cancer". Alcohol and Alcoholism. 39 (3): 155–65. doi:10.1093/alcalc/agh057. PMID 15082451.
- 1 2 3 4 Seitz, Helmut K.; Becker, Peter (2007). "Alcohol Metabolism and Cancer Risk". Alcohol Research & Health. 30 (1): 38–47. ISSN 1535-7414. PMC 3860434. PMID 17718399.
- 1 2 3 4 5 Varela-Rey, Marta; Woodhoo, Ashwin; Martinez-Chantar, Maria-Luz; Mato, José M.; Lu, Shelly C. (2013). "Alcohol, DNA Methylation, and Cancer". Alcohol Research: Current Reviews. 35 (1): 25–35. ISSN 2168-3492. PMC 3860423. PMID 24313162.
- 1 2 3 4 Purohit V, Khalsa J, Serrano J (April 2005). "Mechanisms of alcohol-associated cancers: introduction and summary of the symposium". Alcohol. 35 (3): 155–60. doi:10.1016/j.alcohol.2005.05.001. PMID 16054976. Archived from the original on 11 December 2021. Retrieved 25 September 2022.
- 1 2 3 Boffetta P, Hashibe M (February 2006). "Alcohol and cancer". The Lancet Oncology. 7 (2): 149–156. doi:10.1016/S1470-2045(06)70577-0. PMID 16455479. Archived from the original on 23 May 2013. Retrieved 25 September 2022.
- 1 2 Shield, Kevin D.; Soerjomataram, Isabelle; Rehm, Jürgen (2016). "Alcohol Use and Breast Cancer: A Critical Review". Alcoholism: Clinical and Experimental Research. 40 (6): 1166–1181. doi:10.1111/acer.13071. PMID 27130687. Archived from the original on 14 September 2022. Retrieved 25 September 2022.
- 1 2 3 4 "Alcohol and Cancer". Alcohol Alert. 21. 1993. Archived from the original on 23 December 2005. Retrieved 25 September 2022.
- 1 2 Blot WJ, McLaughlin JK, Winn DM, et al. (1 June 1988). "Smoking and drinking in relation to oral and pharyngeal cancer". Cancer Research. 48 (11): 3282–7. PMID 3365707. Archived from the original on 7 July 2012. Retrieved 25 September 2022.
- ↑ Lopez-Lazaro M (October 2016). "A local mechanism by which alcohol consumption causes cancer" (PDF). Oral Oncology. 62: 149–152. doi:10.1016/j.oraloncology.2016.10.001. hdl:11441/52478. PMID 27720397. Archived from the original on 29 September 2022. Retrieved 25 September 2022.
- ↑ Rush University Medical Center Alcohol Activates Cellular Changes That Make Tumor Cells Spread Archived 11 June 2016 at the Wayback Machine 26 October 2009
- ↑ Forsyth CB, Tang Y, Shaikh M, Zhang L, Keshavarzian A (January 2010). "Alcohol stimulates activation of Snail, epidermal growth factor receptor signaling, and biomarkers of epithelial-mesenchymal transition in colon and breast cancer cells". Alcohol. Clin. Exp. Res. 34 (1): 19–31. doi:10.1111/j.1530-0277.2009.01061.x. PMC 3689303. PMID 19860811.
- ↑ Matsuhashi T, Yamada N, Shinzawa H, Takahashi T (June 1996). "Effect of alcohol on tumor growth of hepatocellular carcinoma with type C cirrhosis". Internal Medicine. 35 (6): 443–8. doi:10.2169/internalmedicine.35.443. PMID 8835593.
In conclusion we found that alcohol intake was closely related to the tumor growth of HCC in patients with type C cirrhosis.
- ↑ Gu JW, Bailey AP, Sartin A, Makey I, Brady AL (January 2005). "Ethanol stimulates tumor progression and expression of vascular endothelial growth factor in chick embryos". Cancer. 103 (2): 422–31. doi:10.1002/cncr.20781. PMID 15597382. S2CID 17578583.
- ↑ "Equivalent of 2–4 Drinks Daily Fuels Blood Vessel Growth, Encourages Cancer Tumors in Mice" (Press release). American Physiological Society. 3 April 2006. Archived from the original on 29 June 2006. Retrieved 26 June 2009.
- ↑ Tan W, Bailey AP, Shparago M, et al. (August 2007). "Chronic alcohol consumption stimulates VEGF expression, tumor angiogenesis and progression of melanoma in mice". Cancer Biology & Therapy. 6 (8): 1211–7. doi:10.4161/cbt.6.8.4383. PMID 17660711. Archived from the original on 24 April 2020. Retrieved 25 September 2022.

- ↑ Núñez NP, Carter PA, Meadows GG (May 2002). "Alcohol consumption promotes body weight loss in melanoma-bearing mice". Alcoholism: Clinical and Experimental Research. 26 (5): 617–26. doi:10.1111/j.1530-0277.2002.tb02583.x. PMID 12045469.
- ↑ Pöschl, Gudrun; Stickel, Felix; Wang, Xiang D.; Seitz, Helmut K. (February 2004). "Alcohol and cancer: genetic and nutritional aspects". Proceedings of the Nutrition Society. 63 (1): 65–71. doi:10.1079/PNS2003323. ISSN 0029-6651. PMID 15070439. S2CID 7130931. Archived from the original on 29 September 2022. Retrieved 25 September 2022.
- ↑ Homann N, Stickel F, König IR, et al. (April 2006). "Alcohol dehydrogenase 1C*1 allele is a genetic marker for alcohol-associated cancer in heavy drinkers". International Journal of Cancer. 118 (8): 1998–2002. doi:10.1002/ijc.21583. PMID 16287084. S2CID 11716548.
- ↑ "Clues to alcohol cancer mystery". BBC News. 25 May 2008. Archived from the original on 12 February 2009. Retrieved 29 June 2009.
- ↑ "Oculocutaneous tyrosinemia/tyrosine aminotransferase deficiency", Atlas of Inherited Metabolic Diseases 3E, CRC Press, 30 December 2011, pp. 164–170, doi:10.1201/b15310-23, ISBN 978-1-4441-1225-2
- 1 2 3 4 5 "Increased alcohol use linked with higher risk of cancer in new study". CNN. Archived from the original on 7 September 2022. Retrieved 25 September 2022.
- 1 2 3 4 5 6 7 Allen NE, Beral V, Casabonne D, et al. (March 2009). "Moderate alcohol intake and cancer incidence in women". Journal of the National Cancer Institute. 101 (5): 296–305. doi:10.1093/jnci/djn514. PMID 19244173.
- ↑ "Alcohol Consumption". Cancer Trends Progress Report – 2007 Update. National Cancer Institute. December 2007. Archived from the original on 1 May 2019. Retrieved 29 June 2009.
- ↑ "Research Projects: Pooled analysis investigating the effects of beer, wine and liquor consumption on the risk of head and neck cancers". The International Head and Neck Cancer Epidemiology Consortium. Archived from the original on 11 December 2008. Retrieved 29 June 2009.
- ↑ Garavello W, Bosetti C, Gallus S, et al. (February 2006). "Type of alcoholic beverage and the risk of laryngeal cancer". European Journal of Cancer Prevention. 15 (1): 69–73. doi:10.1097/01.cej.0000186641.19872.04. PMID 16374233. S2CID 29247309.
- ↑ "Alcohol and cancer: is drinking the new smoking?" (Press release). Centre for Addiction and Mental Health. 26 September 2007. Archived from the original on 7 September 2008. Retrieved 29 June 2009.
- ↑ "Alcohol And Cancer: Is Drinking The New Smoking?" (Press release). Centre for Addiction and Mental Health, Science Daily. 28 September 2007. Archived from the original on 11 December 2021. Retrieved 29 June 2009.
- ↑ Warnakulasuriya S, Parkkila S, Nagao T, et al. (2007). "Demonstration of ethanol-induced protein adducts in oral leukoplakia (pre-cancer) and cancer". Journal of Oral Pathology & Medicine. 37 (3): 157–165. doi:10.1111/j.1600-0714.2007.00605.x. PMID 18251940.
- ↑ Alcohol and oral cancer research breakthrough Archived 2 May 2009 at the Wayback Machine
- ↑ "What Are the Risk Factors for Breast Cancer?". American Cancer Society. 31 May 2009. Archived from the original on 29 April 2009. Retrieved 29 June 2009.
- ↑ "What You Need To Know About Breast Cancer". National Cancer Institute. Archived from the original on 5 October 2014. Retrieved 25 September 2022.
- ↑ "Definite breast cancer risks". CancerHelp UK. Cancer Research UK. 30 August 2017. Archived from the original on 11 February 2009. Retrieved 25 September 2022.
- ↑ "Guide to Breast Cancer" (PDF). American Society of Clinical Oncology. 2008. p. 6. Archived from the original (PDF) on 2 September 2009. Retrieved 29 June 2009.
- ↑ Room, R; Babor, T; Rehm, J (2005). "Alcohol and public health". The Lancet. 365 (9458): 519–30. doi:10.1016/S0140-6736(05)17870-2. PMC 5936368. PMID 15705462. S2CID 9350950.
- 1 2 Non-Technical Summary Archived 24 July 2006 at the Wayback Machine. UK Committee on Carcinogenicity of Chemicals in Food Consumer Products and the Environment (COC)
- ↑ American Association for Cancer Research Alcohol Consumption Increases Risk of Breast Cancer Recurrence 10 December 2009 Archived 1 March 2010 at the Wayback Machine
- ↑ Alcohol link to breast cancer recurrence Archived 9 February 2020 at the Wayback Machine. BBC. 11 December 2009
- ↑ Zisman AL, Nickolov A, Brand RE, Gorchow A, Roy HK (March 2006). "Associations between the age at diagnosis and location of colorectal cancer and the use of alcohol and tobacco: implications for screening". Archives of Internal Medicine. 166 (6): 629–34. doi:10.1001/archinte.166.6.629. PMID 16567601.
- ↑ "Types of cancer". World Cancer Research Fund. Archived from the original on 9 June 2009. Retrieved 29 June 2009.
- ↑ "Colorectal Cancer – Step 1: Find Out About Colorectal Cancer Risk". National Cancer Institute. Archived from the original on 22 April 2009. Retrieved 29 June 2009.
- ↑ "Colorectal Cancer Prevention". National Cancer Institute. 7 May 2009. Archived from the original on 21 April 2015. Retrieved 29 June 2009.
- ↑ "Food types and bowel cancer". Cancer Research. 19 September 2008. Archived from the original on 11 March 2009. Retrieved 29 June 2009.
- ↑ "What Are the Risk Factors for Colorectal Cancer?". American Cancer Society. 18 May 2009. Archived from the original on 19 April 2008. Retrieved 26 June 2009.
- ↑ "Colon Cancer: Risk factors". Mayo Clinic. 2 May 2008. Archived from the original on 1 October 2013. Retrieved 29 June 2009.
- ↑ "Assessing Your Risk for Colorectal Cancer". Colorectal Cancer Coalition. 9 January 2009. Archived from the original on 27 April 2009. Retrieved 29 June 2009.
- ↑ "alcohol". 3 November 2015. Archived from the original on 5 March 2016. Retrieved 25 September 2022.
- ↑ Sloan-Kettering – Colorectal Cancer: Risk Reduction
- ↑ World Cancer Research Fund; American Institute for Cancer Research (2007). Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective (PDF). Washington, D.C.: American Institute for Cancer Research. ISBN 978-0-9722522-2-5. Archived from the original (PDF) on 25 March 2009. Retrieved 29 June 2009.
- ↑ National Cancer Institute (NCI) Cancer Trends Progress Report Alcohol Consumption Archived 16 December 2012 at the Wayback Machine
- ↑ Fedirko, V.; Tramacere, I.; Bagnardi, V.; Rota, M.; Scotti, L.; Islami, F.; Negri, E.; Straif, K.; Romieu, I.; La Vecchia, C.; Boffetta, P.; Jenab, M. (9 February 2011). "Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies". Annals of Oncology. 22 (9): 1958–1972. doi:10.1093/annonc/mdq653. PMID 21307158.
- ↑ Alcohol and Cancer Risk Archived 19 July 2022 at the Wayback Machine. cancer.gov
- ↑ Liver Cancer Risk Factors Archived 16 January 2014 at the Wayback Machine. cancer.org
- ↑ Risk Factors. umgcc.or Archived 23 February 2009 at the Wayback Machine
- ↑ Liver Cancer: The Basics Archived 13 January 2016 at the Wayback Machine. oncolink.org
- ↑ Liver Cancer. utmedicalcenter.org Archived 28 July 2011 at the Wayback Machine
- ↑ Takada, Akira; Shujiro Takase; Mikihiro Tsutsumi (1992). "Alcohol and Hepatic Carcinogenesis". In Raz Yirmiya; Anna N. Taylor (eds.). Alcohol, Immunity, and Cancer. Boca Raton, Florida: CRC Press. pp. 187–209. ISBN 978-0-8493-5761-9.
- ↑ Villa, Erica; Margherita Melegari; Federico Manenti (1992). "Alcohol, Viral Hepatitis, and Hepatocellular Carcinoma". In Ronald Ross Watson (ed.). Alcohol and cancer. Boca Raton, Florida: CRC Press. pp. 151–165. ISBN 978-0-8493-7938-3. Archived from the original on 26 December 2021. Retrieved 25 September 2022.
- ↑ Duffy, S.W., and Sharples, L.D. Alcohol and cancer risk. In: Duffy, J.L., ed. Alcohol and Illness: The Epidemiological Viewpoint. Edinburgh: Edinburgh University Press, 1992. pp. 64–127.'
- ↑ Franceschi S, Montella M, Polesel J, et al. (April 2006). "Hepatitis viruses, alcohol, and tobacco in the etiology of hepatocellular carcinoma in Italy". Cancer Epidemiology, Biomarkers & Prevention. 15 (4): 683–9. doi:10.1158/1055-9965.EPI-05-0702. PMID 16614109.
- ↑ Donato F, Tagger A, Chiesa R, et al. (September 1997). "Hepatitis B and C virus infection, alcohol drinking, and hepatocellular carcinoma: a case-control study in Italy. Brescia HCC Study". Hepatology. 26 (3): 579–84. doi:10.1002/hep.510260308. PMID 9303486. S2CID 73143125.
- ↑ Freudenheim JL, Ritz J, Smith-Warner SA, et al. (1 September 2005). "Alcohol consumption and risk of lung cancer: a pooled analysis of cohort studies". The American Journal of Clinical Nutrition. 82 (3): 657–67. doi:10.1093/ajcn.82.3.657. PMID 16155281.
- ↑ Boston University Alcohol Consumption and Lung Cancer: Are They Connected? Archived 20 September 2006 at the Wayback Machine
- ↑ Fehringer, Gordon; Brenner, Darren R.; Zhang, Zuo-Feng; Lee, Yuan-Chin Amy; Matsuo, Keitaro; Ito, Hidemi; Lan, Qing; Vineis, Paolo; Johansson, Mattias; Overvad, Kim; Riboli, Elio; Trichopoulou, Antonia; Sacerdote, Carlotta; Stucker, Isabelle; Boffetta, Paolo (1 May 2017). "Alcohol and lung cancer risk among never smokers: A pooled analysis from the international lung cancer consortium and the SYNERGY study: Alcohol and lung cancer risk among never smokers". International Journal of Cancer. 140 (9): 1976–1984. doi:10.1002/ijc.30618. PMC 5356930. PMID 28120396.
- ↑ Mahamat‐Saleh, Yahya; Al‐Rahmoun, Marie; Severi, Gianluca; Ghiasvand, Reza; Veierod, Marit B.; Caini, Saverio; Palli, Domenico; Botteri, Edoardo; Sacerdote, Carlotta; Ricceri, Fulvio; Lukic, Marko; Sánchez, Maria J.; Pala, Valeria; Tumino, Rosario; Chiodini, Paolo (30 August 2022). "Baseline and lifetime alcohol consumption and risk of skin cancer in the European Prospective Investigation into Cancer and Nutrition cohort ( EPIC )". International Journal of Cancer: ijc.34253. doi:10.1002/ijc.34253. ISSN 0020-7136. PMID 36053839. S2CID 251706941.
- ↑ Millen AE, Tucker MA, Hartge P, et al. (1 June 2004). "Diet and melanoma in a case-control study". Cancer Epidemiology, Biomarkers & Prevention. 13 (6): 1042–51. doi:10.1158/1055-9965.1042.13.6. PMID 15184262. S2CID 2489716. Archived from the original on 7 July 2012. Retrieved 25 September 2022.
- 1 2 Bagnardi V, Blangiardo M, La Vecchia C, Corrao G (2001). "Alcohol consumption and the risk of cancer: a meta-analysis". Alcohol Research & Health. 25 (4): 263–70. PMC 6705703. PMID 11910703. Archived from the original on 20 June 2019. Retrieved 25 September 2022.
- 1 2 Chen MJ, Chiou YY, Wu DC, Wu SL (November 2000). "Lifestyle habits and gastric cancer in a hospital-based case-control study in Taiwan". The American Journal of Gastroenterology. 95 (11): 3242–9. doi:10.1111/j.1572-0241.2000.03260.x. PMID 11095349. S2CID 23570395.
- ↑ Inoue M, Tajima K, Hirose K, Kuroishi T, Gao CM, Kitoh T (February 1994). "Life-style and subsite of gastric cancer—joint effect of smoking and drinking habits". International Journal of Cancer. 56 (4): 494–9. doi:10.1002/ijc.2910560407. PMID 8112885. S2CID 21402545.
- 1 2 Sjödahl K, Lu Y, Nilsen TI, et al. (January 2007). "Smoking and alcohol drinking in relation to risk of gastric cancer: a population-based, prospective cohort study". International Journal of Cancer. 120 (1): 128–32. doi:10.1002/ijc.22157. PMID 17036324. S2CID 26972976.
- ↑ "Stomach Cancer risk factors". Archived from the original on 19 July 2012. Retrieved 25 September 2022.
- ↑ Tinelli A, Vergara D, Martignago R, et al. (2008). "Hormonal carcinogenesis and socio-biological development factors in endometrial cancer: a clinical review". Acta Obstet Gynecol Scand. 87 (11): 1101–13. doi:10.1080/00016340802160079. PMID 18607816. S2CID 1910334.
- ↑ UK Department of Health Review of Alcohol: Association with Endometrial Cancer p8
- ↑ Newcomb PA, Trentham-Dietz A, Storer BE (1997). "Alcohol consumption in relation to endometrial cancer risk". Cancer Epidemiology, Biomarkers & Prevention. 6 (10): 775–778. PMID 9332758. Archived from the original on 16 October 2008. Retrieved 25 September 2022.
- ↑ Setiawan VW, Monroe KR, Goodman MT, Kolonel LN, Pike MC, Henderson BE (February 2008). "Alcohol consumption and endometrial cancer risk: The Multiethnic Cohort". International Journal of Cancer. 122 (3): 634–8. doi:10.1002/ijc.23072. PMC 2667794. PMID 17764072.
- ↑ Friberg E, Wolk A (January 2009). "Long-term alcohol consumption and risk of endometrial cancer incidence: a prospective cohort study". Cancer Epidemiology, Biomarkers & Prevention. 18 (1): 355–8. doi:10.1158/1055-9965.EPI-08-0993. PMID 19124521. Archived from the original on 13 January 2016. Retrieved 25 September 2022.
- ↑ Moerman CJ, Bueno-de-Mesquita HB (1999). "The epidemiology of gallbladder cancer: lifestyle related risk factors and limited surgical possibilities for prevention". Hepatogastroenterology. 46 (27): 1533–9. PMID 10430290.
- ↑ Ji J, Couto E, Hemminki K (September 2005). "Incidence differences for gallbladder cancer between occupational groups suggest an etiological role for alcohol". International Journal of Cancer. 116 (3): 492–3. doi:10.1002/ijc.21055. PMID 15800949. S2CID 32298422.
- ↑ Pandey M, Shukla VK (August 2003). "Lifestyle, parity, menstrual and reproductive factors and risk of gallbladder cancer". European Journal of Cancer Prevention. 12 (4): 269–72. doi:10.1097/00008469-200308000-00005. PMID 12883378. S2CID 32148865.
- ↑ Yagyu K, Kikuchi S, Obata Y, et al. (February 2008). "Cigarette smoking, alcohol drinking and the risk of gallbladder cancer death: a prospective cohort study in Japan". International Journal of Cancer. 122 (4): 924–9. doi:10.1002/ijc.23159. PMID 17955487. S2CID 29223553.
- ↑ La Vecchia C, Negri E, Franceschi S, Parazzini F, Gentile A, Fasoli M (September 1992). "Alcohol and epithelial ovarian cancer". Journal of Clinical Epidemiology. 45 (9): 1025–30. doi:10.1016/0895-4356(92)90119-8. PMID 1432017.
- 1 2 Alcohol consumption and cancer risk Archived 23 December 2012 at archive.today
- ↑ Genkinger JM, Hunter DJ, Spiegelman D, et al. (March 2006). "Alcohol intake and ovarian cancer risk: a pooled analysis of 10 cohort studies". British Journal of Cancer. 94 (5): 757–62. doi:10.1038/sj.bjc.6603020. PMC 2361197. PMID 16495916.
- ↑ Yip, Ian; Heber, David; Aronson, William (1999). "Nutrition and Prostate Cancer" (PDF). Urologic Clinics of North America. 26 (2): 403–411. doi:10.1016/S0094-0143(05)70079-3. PMID 10361562. Archived from the original (PDF) on 21 May 2009.
- ↑ Bagnardi V, Blangiardo M, La Vecchia C, Corrao G (November 2001). "A meta-analysis of alcohol drinking and cancer risk". British Journal of Cancer. 85 (11): 1700–5. doi:10.1054/bjoc.2001.2140. PMC 2363992. PMID 11742491.
- ↑ Platz EA, Leitzmann MF, Rimm EB, Willett WC, Giovannucci E (March 2004). "Alcohol intake, drinking patterns, and risk of prostate cancer in a large prospective cohort study". American Journal of Epidemiology. 159 (5): 444–53. doi:10.1093/aje/kwh062. PMID 14977640.
- 1 2 Sesso HD, Paffenbarger RS, Lee IM (August 2001). "Alcohol consumption and risk of prostate cancer: The Harvard Alumni Health Study". International Journal of Epidemiology. 30 (4): 749–55. doi:10.1093/ije/30.4.749. PMID 11511598.
- 1 2 Schoonen WM, Salinas CA, Kiemeney LA, Stanford JL (January 2005). "Alcohol consumption and risk of prostate cancer in middle-aged men". International Journal of Cancer. 113 (1): 133–40. doi:10.1002/ijc.20528. PMID 15386436. S2CID 19513583.
- ↑ Cancer Research UK Prostate Cancer risk factors Archived 13 July 2012 at archive.today
- ↑ Fred Hutchinson Cancer Research Center press release A Glass of Red Wine a Day May Keep Prostate Cancer Away Archived 8 October 2011 at the Wayback Machine
- ↑ Middleton Fillmore K, Chikritzhs T, Stockwell T, Bostrom A, Pascal R (February 2009). "Alcohol use and prostate cancer: a meta-analysis". Molecular Nutrition & Food Research. 53 (2): 240–55. doi:10.1002/mnfr.200800122. PMID 19156715. S2CID 28921992.
- ↑ "Study links alcohol, prostate cancer". ABC News. 14 March 2009. Archived from the original on 20 June 2009. Retrieved 29 June 2009.
- ↑ Chen CC, Neugut AI, Rotterdam H (1 April 1994). "Risk factors for adenocarcinomas and malignant carcinoids of the small intestine: preliminary findings". Cancer Epidemiology, Biomarkers & Prevention. 3 (3): 205–7. PMID 8019367. Archived from the original on 12 July 2012. Retrieved 25 September 2022.
- ↑ Wu AH, Yu MC, Mack TM (March 1997). "Smoking, alcohol use, dietary factors and risk of small intestinal adenocarcinoma". International Journal of Cancer. 70 (5): 512–7. doi:10.1002/(SICI)1097-0215(19970304)70:5<512::AID-IJC4>3.0.CO;2-0. PMID 9052748.
- ↑ Negri E, Bosetti C, La Vecchia C, Fioretti F, Conti E, Franceschi S (July 1999). "Risk factors for adenocarcinoma of the small intestine". International Journal of Cancer. 82 (2): 171–4. doi:10.1002/(SICI)1097-0215(19990719)82:2<171::AID-IJC3>3.0.CO;2-T. PMID 10389747. S2CID 29812362.
- ↑ Infante-Rivard C, El-Zein M (2007). "Parental alcohol consumption and childhood cancers: a review". J Toxicol Environ Health B. 10 (1–2): 101–29. doi:10.1080/10937400601034597. PMID 18074306. S2CID 22394372.
- 1 2 3 Malcolm A. Smith, Lynn A. Gloeckler Ries, James G. Gurney, Julie A. Ross Archived 5 February 2013 at the Wayback Machine National Cancer Institute 34 SEER Pediatric Monograph
- 1 2 3 Gorini G, Stagnaro E, Fontana V, et al. (March 2007). "Alcohol consumption and risk of leukemia: A multicenter case-control study". Leukemia Research. 31 (3): 379–86. doi:10.1016/j.leukres.2006.07.002. PMID 16919329.
- ↑ Shu XO, Ross JA, Pendergrass TW, Reaman GH, Lampkin B, Robison LL (January 1996). "Parental alcohol consumption, cigarette smoking, and risk of infant leukemia: a Childrens Cancer Group study". Journal of the National Cancer Institute. 88 (1): 24–31. doi:10.1093/jnci/88.1.24. PMID 8847721.
- ↑ van Duijn CM, van Steensel-Moll HA, Coebergh JW, van Zanen GE (1 September 1994). "Risk factors for childhood acute non-lymphocytic leukemia: an association with maternal alcohol consumption during pregnancy?". Cancer Epidemiology, Biomarkers & Prevention. 3 (6): 457–60. PMID 8000294. Archived from the original on 23 February 2013. Retrieved 25 September 2022.
- ↑ Oleske D, Golomb HM, Farber MD, Levy PS (May 1985). "A case-control inquiry into the etiology of hairy cell leukemia". American Journal of Epidemiology. 121 (5): 675–83. doi:10.1093/aje/121.5.675. PMID 4014159. Archived from the original on 13 January 2016. Retrieved 25 September 2022.
- ↑ Kyle RA, Rajkumar SV (December 2007). "Epidemiology of the plasma-cell disorders". Best Pract Res Clin Haematol. 20 (4): 637–64. doi:10.1016/j.beha.2007.08.001. PMID 18070711.
- 1 2 Gorini G, Stagnaro E, Fontana V, et al. (January 2007). "Alcohol consumption and risk of Hodgkin's lymphoma and multiple myeloma: a multicentre case-control study". Annals of Oncology. 18 (1): 143–8. doi:10.1093/annonc/mdl352. PMID 17047000.
- 1 2 3 4 Ye W, Lagergren J, Weiderpass E, Nyrén O, Adami HO, Ekbom A (August 2002). "Alcohol abuse and the risk of pancreatic cancer". Gut. 51 (2): 236–9. doi:10.1136/gut.51.2.236. PMC 1773298. PMID 12117886.
- 1 2 3 4 Silverman DT, Brown LM, Hoover RN, et al. (1 November 1995). "Alcohol and pancreatic cancer in blacks and whites in the United States". Cancer Research. 55 (21): 4899–905. PMID 7585527.
- 1 2 3 4 Michaud DS, Giovannucci E, Willett WC, Colditz GA, Fuchs CS (2001). "Coffee and alcohol consumption and the risk of pancreatic cancer in two prospective United States cohorts". Cancer Epidemiology, Biomarkers & Prevention. 10 (5): 429–37. PMID 11352851.
- ↑ Villeneuve PJ, Johnson KC, Hanley AJ, Mao Y (February 2000). "Alcohol, tobacco and coffee consumption and the risk of pancreatic cancer: results from the Canadian Enhanced Surveillance System case-control project. Canadian Cancer Registries Epidemiology Research Group". European Journal of Cancer Prevention. 9 (1): 49–58. doi:10.1097/00008469-200002000-00007. PMID 10777010.
- 1 2 Pancreatic cancer risks and causes Archived 10 February 2009 at the Wayback Machine. Cancer Research UK
- ↑ Ahlgren JD (April 1996). "Epidemiology and risk factors in pancreatic cancer". Seminars in Oncology. 23 (2): 241–50. PMID 8623060.
- ↑ Cuzick J, Babiker AG (March 1989). "Pancreatic cancer, alcohol, diabetes mellitus and gall-bladder disease". International Journal of Cancer. 43 (3): 415–21. doi:10.1002/ijc.2910430312. PMID 2925272. S2CID 35777641.
- ↑ Harnack LJ, Anderson KE, Zheng W, Folsom AR, Sellers TA, Kushi LH (December 1997). "Smoking, alcohol, coffee, and tea intake and incidence of cancer of the exocrine pancreas: the Iowa Women's Health Study". Cancer Epidemiology, Biomarkers & Prevention. 6 (12): 1081–6. PMID 9419407.
- ↑ Schottenfeld, D. and J. Fraumeni, ed. (1996) Cancer epidemiology and prevention. 2nd ed., Oxford University Press: Oxford
- ↑ Olsen GW, Mandel JS, Gibson RW, Wattenberg LW, Schuman LM (August 1989). "A case-control study of pancreatic cancer and cigarettes, alcohol, coffee and diet". American Journal of Public Health. 79 (8): 1016–9. doi:10.2105/AJPH.79.8.1016. PMC 1349898. PMID 2751016.
- ↑ "Pancreatic cancer risk factors". Info.cancerresearchuk.org. 4 November 2008. Archived from the original on 12 July 2012. Retrieved 15 September 2009.
- 1 2 3 Genkinger JM, Spiegelman D, Anderson KE, Bergkvist L, Bernstein L, van den Brandt PA, English DR, Freudenheim JL, Fuchs CS, Giles GG, Giovannucci E, Hankinson SE, Horn-Ross PL, Leitzmann M, Männistö S, Marshall JR, McCullough ML, Miller AB, Reding DJ, Robien K, Rohan TE, Schatzkin A, Stevens VL, Stolzenberg-Solomon RZ, Verhage BA, Wolk A, Ziegler RG, Smith-Warner SA (March 2009). "Alcohol intake and pancreatic cancer risk: a pooled analysis of fourteen cohort studies". Cancer Epidemiology, Biomarkers & Prevention. 18 (3): 765–76. doi:10.1158/1055-9965.EPI-08-0880. PMC 2715951. PMID 19258474.
In summary, a weak positive association between alcohol intake during adulthood and pancreatic cancer risk was observed in the highest category of intake (≥30g/day or approximately 2 alcoholic beverages/day). Associations with alcohol intake were stronger among individuals who were normal weight. Thus, our findings are consistent with a modest increase in risk of pancreatic cancer for alcohol intakes of at least 30 grams/day.
- ↑ Zatonski WA, Boyle P, Przewozniak K, Maisonneuve P, Drosik K, Walker AM (February 1993). "Cigarette smoking, alcohol, tea and coffee consumption and pancreas cancer risk: a case-control study from Opole, Poland". International Journal of Cancer. 53 (4): 601–7. doi:10.1002/ijc.2910530413. PMID 8436433. S2CID 39084516.
- ↑ Durbec JP, Chevillotte G, Bidart JM, Berthezene P, Sarles H (April 1983). "Diet, alcohol, tobacco and risk of cancer of the pancreas: a case-control study". British Journal of Cancer. 47 (4): 463–70. doi:10.1038/bjc.1983.75. PMC 2011343. PMID 6849792.
- ↑ Bueno de Mesquita HB, Maisonneuve P, Moerman CJ, Runia S, Boyle P (February 1992). "Lifetime consumption of alcoholic beverages, tea and coffee and exocrine carcinoma of the pancreas: a population-based case-control study in The Netherlands". International Journal of Cancer. 50 (4): 514–22. doi:10.1002/ijc.2910500403. PMID 1537615. S2CID 23170705.
- ↑ Harnack LJ, Anderson KE, Zheng W, Folsom AR, Sellers TA, Kushi LH (1997). "Smoking, alcohol, coffee, and tea intake and incidence of cancer of the exocrine pancreas: the Iowa Women's Health Study". Cancer Epidemiology, Biomarkers & Prevention. 6 (12): 1081–6. PMID 9419407.
- ↑ Durbec JP, Chevillotte G, Bidart JM, Berthezene P, Sarles H (April 1983). "Diet, alcohol, tobacco and risk of cancer of the pancreas: a case-control study". British Journal of Cancer. 47 (4): 463–70. doi:10.1038/bjc.1983.75. PMC 2011343. PMID 6849792.
- ↑ Bueno de Mesquita HB, Maisonneuve P, Moerman CJ, Runia S, Boyle P (February 1992). "Lifetime consumption of alcoholic beverages, tea and coffee and exocrine carcinoma of the pancreas: a population-based case-control study in The Netherlands". International Journal of Cancer. 50 (4): 514–22. doi:10.1002/ijc.2910500403. PMID 1537615. S2CID 23170705.
- ↑ Villeneuve PJ, Johnson KC, Hanley AJ, Mao Y (February 2000). "Alcohol, tobacco and coffee consumption and the risk of pancreatic cancer: results from the Canadian Enhanced Surveillance System case-control project. Canadian Cancer Registries Epidemiology Research Group". European Journal of Cancer Prevention. 9 (1): 49–58. doi:10.1097/00008469-200002000-00007. PMID 10777010.
- ↑ Genkinger JM, Spiegelman D, Anderson KE, et al. (March 2009). "Alcohol Intake and Pancreatic Cancer Risk: A Pooled Analysis of Fourteen Cohort Studies". Cancer Epidemiology, Biomarkers & Prevention. 18 (3): 765–76. doi:10.1158/1055-9965.EPI-08-0880. PMC 2715951. PMID 19258474.
- ↑ Kuijten RR, Bunin GR, Nass CC, Meadows AT (1 May 1990). "Gestational and familial risk factors for childhood astrocytoma: results of a case-control study" (PDF). Cancer Research. 50 (9): 2608–12. PMID 2328486. Archived (PDF) from the original on 29 September 2022. Retrieved 25 September 2022.
- ↑ Ben-Menachem T (August 2007). "Risk factors for cholangiocarcinoma". Eur J Gastroenterol Hepatol. 19 (8): 615–7. doi:10.1097/MEG.0b013e328224b935. PMID 17625428. S2CID 25306939.
- ↑ Pelucchi C, La Vecchia C (February 2009). "Alcohol, coffee, and bladder cancer risk: a review of epidemiological studies". Eur. J. Cancer Prev. 18 (1): 62–8. doi:10.1097/CEJ.0b013e32830c8d44. PMID 19077567.
- 1 2 3 Weiderpass E, Ye W, Tamimi R, et al. (1 August 2001). "Alcoholism and risk for cancer of the cervix uteri, vagina, and vulva". Cancer Epidemiology, Biomarkers & Prevention. 10 (8): 899–901. PMID 11489758.
- ↑ Claus EB, Stowe M, Carter D (December 2001). "Breast carcinoma in situ: risk factors and screening patterns". Journal of the National Cancer Institute. 93 (23): 1811–7. doi:10.1093/jnci/93.23.1811. PMID 11734598. S2CID 13818666.
- ↑ Kuijten RR, Bunin GR (1 May 1993). "Risk factors for childhood brain tumors". Cancer Epidemiology, Biomarkers & Prevention. 2 (3): 277–88. PMID 8318881.
- ↑ Howe GR, Burch JD, Chiarelli AM, Risch HA, Choi BC (1989). "An exploratory case-control study of brain tumors in children". Cancer Research. 49 (15): 4349–52. PMID 2743324.
- ↑ Preston-Martin S, Yu MC, Benton B, Henderson BE (1982). "N-Nitroso compounds and childhood brain tumors: a case-control study". Cancer Research. 42 (12): 5240–5. PMID 7139628.
- ↑ Stang A, Ahrens W, Anastassiou G, Jöckel KH (December 2003). "Phenotypical characteristics, lifestyle, social class and uveal melanoma". Ophthalmic Epidemiol. 10 (5): 293–302. doi:10.1076/opep.10.5.293.17319. PMID 14566630. S2CID 1592701.
- ↑ Chen L, Gallicchio L, Boyd-Lindsley K, et al. (2009). "Alcohol Consumption and the Risk of Nasopharyngeal Carcinoma: A Systematic Review". Nutr Cancer. 61 (1): 1–15. doi:10.1080/01635580802372633. PMC 3072894. PMID 19116871.
- ↑ Heck JE, Ritz B, Hung RJ, Hashibe M, Boffetta P (March 2009). "The epidemiology of neuroblastoma: a review". Paediatr Perinat Epidemiol. 23 (2): 125–43. doi:10.1111/j.1365-3016.2008.00983.x. PMID 19159399.
- ↑ Actis AB, Eynard AR (November 2000). "Influence of environmental and nutritional factors on salivary gland tumorigenesis with a special reference to dietary lipids". Eur J Clin Nutr. 54 (11): 805–10. doi:10.1038/sj.ejcn.1601077. PMID 11114673.
- ↑ van Hemelrijck; Mieke J.J. (2007). "Tobacco, Alcohol and Dietary Consumption: Behavior Risks Associated with Testicular Cancer?". Current Urology. 1 (2): 57–63. doi:10.1159/000106534. S2CID 71608840.
- ↑ Dal Maso L, Bosetti C, La Vecchia C, Franceschi S (February 2009). "Risk factors for thyroid cancer: an epidemiological review focused on nutritional factors". Cancer Causes Control. 20 (1): 75–86. doi:10.1007/s10552-008-9219-5. PMID 18766448. S2CID 25427265.
- ↑ Meinhold, C L; Park, Y; Stolzenberg-Solomon, R Z; Hollenbeck, A R; Schatzkin, A; Berrington De Gonzalez, A (2009). "Alcohol intake and risk of thyroid cancer in the NIH-AARP Diet and Health Study". British Journal of Cancer. 101 (9): 1630–4. doi:10.1038/sj.bjc.6605337. PMC 2778506. PMID 19862001.
- ↑ Allen, Naomi E.; Beral, Valerie; Casabonne, Delphine; Sau, Kan Wan; Reeves, Gillian K.; Brown, Anna; Green, Jane (2009). "Moderate Alcohol Intake and Cancer Incidence in Women". Journal of the National Cancer Institute. 101 (5): 296–305. doi:10.1093/jnci/djn514. PMID 19244173. Archived from the original on 6 September 2010. Retrieved 25 September 2022.
- 1 2 Madsen BS, Jensen HL, van den Brule AJ, Wohlfahrt J, Frisch M (June 2008). "Risk factors for invasive squamous cell carcinoma of the vulva and vagina—population-based case-control study in Denmark". International Journal of Cancer. 122 (12): 2827–34. doi:10.1002/ijc.23446. PMID 18348142. S2CID 11542729.
- ↑ Parazzini F, Moroni S, Negri E, La Vecchia C, Dal Pino D, Cavalleri E (December 1995). "Selected food intake and risk of vulvar cancer". Cancer. 76 (11): 2291–6. doi:10.1002/1097-0142(19951201)76:11<2291::AID-CNCR2820761117>3.0.CO;2-W. PMID 8635034. S2CID 19693085.
- ↑ Besson H, Brennan P, Becker N, et al. (August 2006). "Tobacco smoking, alcohol drinking and non-Hodgkin's lymphoma: A European multicenter case-control study (Epilymph)". International Journal of Cancer. 119 (4): 901–8. doi:10.1002/ijc.21913. PMID 16557575. S2CID 41632578.
- ↑ Nieters A, Deeg E, Becker N (January 2006). "Tobacco and alcohol consumption and risk of lymphoma: results of a population-based case-control study in Germany". International Journal of Cancer. 118 (2): 422–30. doi:10.1002/ijc.21306. PMID 16080191. S2CID 9532867.
- ↑ Deandrea S, Bertuccio P, Chatenoud L, Franceschi S, Serraino D, La Vecchia C (June 2007). "Reply to 'Alcohol consumption and risk of Hodgkin's lymphoma and multiple myeloma: a multicentre case-control study' by Gorini et al". Annals of Oncology. 18 (6): 1119–21. doi:10.1093/annonc/mdm203. PMID 17586754.
- ↑ Lee JE, Hunter DJ, Spiegelman D, et al. (May 2007). "Alcohol intake and renal cell cancer in a pooled analysis of 12 prospective studies". Journal of the National Cancer Institute. 99 (10): 801–10. doi:10.1093/jnci/djk181. PMID 17505075.
- ↑ Pelucchi C, Galeone C, Montella M, et al. (May 2008). "Alcohol consumption and renal cell cancer risk in two Italian case-control studies". Annals of Oncology. 19 (5): 1003–8. doi:10.1093/annonc/mdm590. PMID 18187482.
- ↑ Rashidkhani B, Akesson A, Lindblad P, Wolk A (December 2005). "Alcohol consumption and risk of renal cell carcinoma: a prospective study of Swedish women". International Journal of Cancer. 117 (5): 848–53. doi:10.1002/ijc.21231. PMID 15957170. S2CID 38418551.
- ↑ Parker AS, Cerhan JR, Lynch CF, Ershow AG, Cantor KP (March 2002). "Gender, alcohol consumption, and renal cell carcinoma". American Journal of Epidemiology. 155 (5): 455–62. doi:10.1093/aje/155.5.455. PMID 11867357.
- ↑ Pelucchi C, La Vecchia C, Negri E, Talamini R, Franceschi S (December 2002). "Alcohol drinking and renal cell carcinoma in women and men". European Journal of Cancer Prevention. 11 (6): 543–5. doi:10.1097/00008469-200212000-00006. PMID 12457106. S2CID 45637355.
- ↑ Mahabir S, Leitzmann MF, Virtanen MJ, et al. (1 January 2005). "Prospective study of alcohol drinking and renal cell cancer risk in a cohort of finnish male smokers". Cancer Epidemiology, Biomarkers & Prevention. 14 (1): 170–5. doi:10.1158/1055-9965.170.14.1. PMID 15668492. S2CID 3141532.
- ↑ Lee JE, Giovannucci E, Smith-Warner SA, Spiegelman D, Willett WC, Curhan GC (June 2006). "Total fluid intake and use of individual beverages and risk of renal cell cancer in two large cohorts". Cancer Epidemiology, Biomarkers & Prevention. 15 (6): 1204–11. doi:10.1158/1055-9965.EPI-05-0889. PMID 16775182.
- ↑ Setiawan VW, Stram DO, Nomura AM, Kolonel LN, Henderson BE (October 2007). "Risk factors for renal cell cancer: the multiethnic cohort". American Journal of Epidemiology. 166 (8): 932–40. doi:10.1093/aje/kwm170. PMID 17656615.
- ↑ Morton LM, Zheng T, Holford TR, et al. (July 2005). "Alcohol consumption and risk of non-Hodgkin lymphoma: a pooled analysis". The Lancet Oncology. 6 (7): 469–76. doi:10.1016/S1470-2045(05)70214-X. PMID 15992695.
- ↑ Lim U, Morton LM, Subar AF, et al. (September 2007). "Alcohol, smoking, and body size in relation to incident Hodgkin's and non-Hodgkin's lymphoma risk". American Journal of Epidemiology. 166 (6): 697–708. doi:10.1093/aje/kwm122. PMID 17596266.
- ↑ Lim U, Schenk M, Kelemen LE, et al. (November 2005). "Dietary determinants of one-carbon metabolism and the risk of non-Hodgkin's lymphoma: NCI-SEER case-control study, 1998–2000". American Journal of Epidemiology. 162 (10): 953–64. doi:10.1093/aje/kwi310. PMID 16221809.
- ↑ Briggs NC, Levine RS, Bobo LD, Haliburton WP, Brann EA, Hennekens CH (September 2002). "Wine drinking and risk of non-Hodgkin's lymphoma among men in the United States: a population-based case-control study". American Journal of Epidemiology. 156 (5): 454–62. doi:10.1093/aje/kwf058. PMID 12196315.
- ↑ Besson H, Brennan P, Becker N, et al. (August 2006). "Tobacco smoking, alcohol drinking and Hodgkin's lymphoma: a European multi-centre case–control study (EPILYMPH)". British Journal of Cancer. 95 (3): 378–84. doi:10.1038/sj.bjc.6603229. PMC 2360649. PMID 16819547.
- ↑ Chiu BC, Cerhan JR, Gapstur SM, et al. (July 1999). "Alcohol consumption and non-Hodgkin lymphoma in a cohort of older women". British Journal of Cancer. 80 (9): 1476–82. doi:10.1038/sj.bjc.6690547. PMC 2363074. PMID 10424754.
- ↑ Hagner, Patrick R.; Mazan-Mamczarz, Krystyna; Dai, Bojie; Corl, Sharon; Zhao, X. Frank; Gartenhaus, Ronald B. (2009). "Alcohol consumption and decreased risk of non-Hodgkin lymphoma: Role of mTOR dysfunction". Blood. 113 (22): 5526–5535. doi:10.1182/blood-2008-11-191783. PMID 19293424.
- ↑ Willett EV, Smith AG, Dovey GJ, Morgan GJ, Parker J, Roman E (October 2004). "Tobacco and alcohol consumption and the risk of non-Hodgkin lymphoma". Cancer Causes & Control. 15 (8): 771–80. doi:10.1023/B:CACO.0000043427.77739.60. PMID 15456990. S2CID 37360569.
- ↑ Chang ET, Smedby KE, Zhang SM, et al. (December 2004). "Alcohol intake and risk of non-Hodgkin lymphoma in men and women". Cancer Causes & Control. 15 (10): 1067–76. doi:10.1007/s10552-004-2234-2. PMID 15801490. S2CID 38550648.
- ↑ Talamini R, Polesel J, Spina M, et al. (April 2008). "The impact of tobacco smoking and alcohol drinking on survival of patients with non-Hodgkin lymphoma". International Journal of Cancer. 122 (7): 1624–9. doi:10.1002/ijc.23205. PMID 18059029. S2CID 12974079.
- ↑ Alcohol and Serious Consequences: Risks Increase Even With "Moderate" Intake Archived 20 September 2006 at the Wayback Machine
- ↑ Corrao G, Bagnardi V, Zambon A, La Vecchia C (May 2004). "A meta-analysis of alcohol consumption and the risk of 15 diseases". Preventive Medicine. 38 (5): 613–9. doi:10.1016/j.ypmed.2003.11.027. PMID 15066364.
- ↑ World Cancer Research Fund, Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective, http://www.dietandcancerreport.org/ Archived 6 October 2015 at the Wayback Machine
- ↑ Petticrew M, Maani Hessari N, Knai C, Weiderpass E, et al. (2018). "How alcohol industry organisations mislead the public about alcohol and cancer". Drug and Alcohol Review. 37 (3): 293–303. doi:10.1111/dar.12596. PMID 28881410. S2CID 892691. Archived from the original on 21 April 2021. Retrieved 25 September 2022.
- ↑ Chaudhuri, Saabira (9 February 2018). "Lawmakers, Alcohol Industry Tussle Over Cancer Labels on Booze". The Wall Street Journal. Archived from the original on 21 January 2021. Retrieved 25 September 2022.
- 1 2 "2019 AICR Cancer Risk Awareness Survey" (PDF). AICR 2019 Cancer Risk Awareness Survey. 2019. Archived (PDF) from the original on 22 December 2021. Retrieved 25 September 2022.
External links
- International: International Agency for Research on Cancer home page
- International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Volume 44 Alcohol Drinking: Summary of Data Reported and Evaluation
- IARC Alcoholic beverages (Group 1) Ethanol in alcoholic beverages (Group 1) VOL.: 96 5. Summary of Data Reported
- Australia: Cancer Control Bulletin Alcohol and cancer risk
- Australia: POSITION STATEMENT: Alcohol and Cancer Prevention
- Australia: Cancer Institute NSW: Alcohol as a cause of Cancer (PDF format)
- Canada: Public Health Agency of Canada / Agence de santé publique du Canada Review of Lifestyle and Environmental Risk Factors for Breast Cancer (Contents and Introduction) PDF (full report in PDF format)
- UK: Committee on Carcinogenicity of Chemicals in Food, Consumer Products Consumption of alcoholic beverages and risk of breast cancer
- UK: Committee on Carcinogenicity of Chemicals in Food, Consumer Products Evidence for association between consumption of alcoholic beverages and breast cancer
- UK: Cancer risk of drinking Archived 3 March 2016 at the Wayback Machine
- US: National Institute on Alcohol Abuse and Alcoholism Alcohol Alert No. 21-1993 Alcohol and cancer Archived 23 December 2005 at the Wayback Machine
- US: National Cancer Institute Archived 12 March 2015 at the Wayback Machine
- US: National Toxicology Program Report on Carcinogens, Eleventh Edition Alcoholic Beverage Consumption (PDF)
- US: Ohio Department of Health Alcohol and cancer (PDF format)
- Other sites
- Toronto Cancer Prevention Coalition Alcohol Work Group Report on the Links between Alcohol and Cancer (PDF format)
- Alcohol consumption and cancer risk
- Even small amounts of alcohol increase a woman's risk of cancer Archived 11 December 2021 at the Wayback Machine
- Science and medical sites