Vaginal cancer
| Vaginal cancer | |
|---|---|
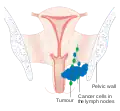 | |
| Stage 3 vaginal cancer | |
| Specialty | Oncology |
| Symptoms | Abnormal vaginal bleeding, pelvic pain, mass within the vagina, pain with urination[1][2] |
| Usual onset | 50 to 70 years of age[3] |
| Types | Squamous cell carcinoma, adenocarcinoma (including clear cell carcinoma), melanoma, sarcoma[1][4] |
| Risk factors | HPV, diethylstilbestrol, smoking, prior hysterectomy for a tumor[1][3] |
| Diagnostic method | Biopsy[5] |
| Differential diagnosis | Cervical cancer, cancer of the vulva[1] |
| Prevention | HPV vaccine, safe sex, not smoking[3] |
| Treatment | Surgery, radiation therapy, chemotherapy, immunotherapy[2] |
| Prognosis | Five year survival 47%[6] |
| Frequency | Uncommon[1] |
Vaginal cancer is when cancer forms from healthy tissue within the vagina.[2][4] Symptoms may include abnormal vaginal bleeding, pelvic pain, pain with sex, a mass within the vagina, and pain with urination.[1][2] If the cervix is involved, it is classified as cervical cancer rather than vaginal cancer.[1]
Risk factors include human papilloma virus (HPV), diethylstilbestrol exposure in utero, smoking, and a prior hysterectomy for a tumor.[1][3] Squamous cell carcinomas make up about 85% of cases while adenocarcinoma make up about 7.5%.[1] Definitive diagnosis is by biopsy.[5] Cancer may also spreads from elsewhere to the vagina and this is more common.[4]
Prevention includes the HPV vaccine, safe sex, and not smoking.[3] Treatment depends on the stage of disease.[2] Options may include surgery, radiation therapy, chemotherapy, and immunotherapy.[2] Vaginal cancer represent less than 2% of female genital cancers.[1] It is most common in those 50 to 70 years of age.[3] The overall five year survival is 47%.[6]
Signs and symptoms
Most vaginal cancers do not cause signs or symptoms early on. When vaginal cancer does cause symptoms, they may include:
- Vaginal discharge or abnormal vaginal bleeding
- Unusually heavy flow of blood
- Bleeding after menopause
- Bleeding between periods; or any other
- Bleeding that is longer than normal
- Blood in the stool or urine
- Frequent or urgent need to urinate
- Feeling constipated[8]
- Pain during sexual intercourse
- a lump or growth in the vagina that can be felt[9]
Enlarged pelvic lymph nodes can sometimes be palpated[10]
Risk factors
- Prenatal exposure to diethylstilbestrol
- Infection with human papillomavirus (HPV) type 16
- Infection with human immunodeficiency virus (HIV) type 1[11][12]
- Previous history of cervical cancer
- Smoking
- Chronic vulvar itching or burning[8]
Diagnosis
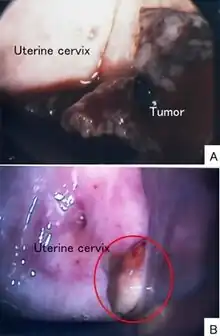
Several tests are used to diagnose vaginal cancer, including:
- Physical exam and history
- Pelvic exam
- Pap smear
- Biopsy
- Colposcopy
Recommendations for women with vaginal cancer is not to have routine surveillance imaging to monitor the cancer unless they have new symptoms or rising tumor markers.[13] Imaging without these indications is discouraged because it is unlikely to detect a recurrence or improve survival, and because it has its own costs and side effects.[13] MRI provides visualization of the extent of vaginal cancer.[14]
Types
There are two primary types of vaginal cancer: squamous-cell carcinoma and adenocarcinoma.[15]
- Squamous-cell carcinoma of the vagina arises from the squamous cells (epithelium) that line the vagina. This is the most common type of vaginal cancer. It is found most often in women aged 60 or older.
- Vaginal adenocarcinoma arises from the glandular (secretory) cells in the lining of the vagina. Adenocarcinoma is more likely to spread to the lungs and lymph nodes.
- Clear cell adenocarcinoma occurs in a small percentage of women (termed "DES-Daughters") born between 1938 and 1973 (later outside the United States) that were exposed to the drug diethylstilbestrol (DES) in utero. DES was prescribed to 5 to 10 million mothers period to prevent possible miscarriages and premature births.[16] Typically, women develop DES-related adenocarcinoma before age 30, but increasing evidence suggests possible effects or cancers (including other forms of vaginal glandular tumors) at a later age. DES-exposure in women is also linked to various infertility and pregnancy complications. Daughters exposed to DES in utero may also have an increased risk of moderate/severe cervical squamous cell dysplasia and an increased risk of breast cancer.[16] Approximately one in 1,000 (0.1%) DES Daughters will be diagnosed with clear cell adenocarcinoma. The risk is virtually non-existent among premenopausal women not exposed to DES.[17]
- Vaginal germ cell tumors (primarily teratoma and endodermal sinus tumor) are rare. They are found most often in infants and children.
- Sarcoma botryoides, a rhabdomyosarcoma also is found most often in infants and children.
- Vaginal melanoma, a melanoma that appears in the vagina.
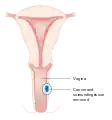
 Stage 1 vaginal cancer
Stage 1 vaginal cancer Stage 2 vaginal cancer
Stage 2 vaginal cancer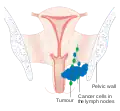 Stage 3 vaginal cancer
Stage 3 vaginal cancer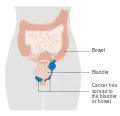 Stage 4A vaginal cancer
Stage 4A vaginal cancer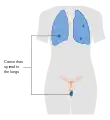 Stage 4B vaginal cancer
Stage 4B vaginal cancer
Management
Historically, the combination of external-beam radiation therapy (EBRT) has been the most common treatment for vaginal cancer. In early stages of vaginal cancer, surgery also has some benefit. This management and treatment is less effective for those with advanced stages of cancer but works well in early stages with high rates of cure. Advanced vaginal cancer only has a 5-year survival rates of 52.2%, 42.5% and 20.5% for patients with stage II, III and IVa disease. Newer treatments for advanced stages of ovarian have been developed. These utilize concurrent carboplatin plus paclitaxel, EBRT and high-dose-rate interstitial brachytherapy (HDR-ISBT).[10]
When the chance of surgical removal of all cancerous tissue is very low or when the surgery has a chance of damaging the bladder, vagina or bowel, radiation therapy is used. When a tumor is less than 4 cm in diameter, radiation therapy provides excellent results. In these instances, the 5-year survival rate is greater than 80%.[10] Treatments are individualized due to the rarity of vaginal cancer studies.[18]
 A local surgery to remove vaginal cancer
A local surgery to remove vaginal cancer A radical hysterectomy to treat vaginal cancer without reconstruction
A radical hysterectomy to treat vaginal cancer without reconstruction A radical hysterectomy for vaginal cancer with reconstruction of the vagina using other tissues
A radical hysterectomy for vaginal cancer with reconstruction of the vagina using other tissues
Epidemiology
Cancer of the vagina is rare and is only 2% of all gynecological cancers less than 0.5% of all cancers in women.[10] Estimated new cases in the United States in 2017 are 4,810. Deaths from vaginal during the same time were 1,240.[15] It is more common in older women.[19]
In the UK, 254 cases of Vaginal cancer were identified in 2014. Deaths from vaginal cancer in this period were 110.[20] Out of those with vaginal cancer, 53% are related to HPV infection.[11]
Research
Gene therapy to treat vaginal cancer is currently in clinical trials.[21]
See also
References
- 1 2 3 4 5 6 7 8 9 10 "Vaginal Cancer Treatment (PDQ®)–Health Professional Version - National Cancer Institute". www.cancer.gov. 9 October 2020. Archived from the original on 9 April 2019. Retrieved 30 October 2020.
- 1 2 3 4 5 6 "Vaginal Cancer Treatment (PDQ®)–Patient Version - National Cancer Institute". www.cancer.gov. 29 May 2020. Archived from the original on 9 April 2019. Retrieved 30 October 2020.
- 1 2 3 4 5 6 "Vaginal Cancer - Risk Factors and Prevention". Cancer.Net. 25 June 2012. Archived from the original on 29 September 2020. Retrieved 30 October 2020.
- 1 2 3 "Vaginal Cancer - Introduction". Cancer.Net. 25 June 2012. Archived from the original on 28 September 2020. Retrieved 30 October 2020.
- 1 2 "Vaginal Cancer - Diagnosis". Cancer.Net. 25 June 2012. Archived from the original on 25 September 2020. Retrieved 30 October 2020.
- 1 2 "Vaginal Cancer - Statistics". Cancer.Net. 25 June 2012. Archived from the original on 30 October 2020. Retrieved 30 October 2020.
- ↑ Tamura, R; Yokoyama, Y; Kobayashi, A; Osawa, Y; Shigeto, T; Futagami, M; Mizunuma, H (2013). "A case of small cell carcinoma of the vagina". Rare tumors. 5 (4): e58. doi:10.4081/rt.2013.e58. PMID 24416492.
- 1 2 "Vaginal and Vulvar Cancer" (PDF). Centers for Disease Control and Prevention. December 2016. Archived (PDF) from the original on 22 December 2017. Retrieved 18 December 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "Symptoms | Vaginal cancer | Cancer Research UK". www.cancerresearchuk.org. 10 September 2015. Archived from the original on 2017-12-22. Retrieved 2017-12-19.
- 1 2 3 4 Mabuchi, Seiji; Kawano, Mahiru; Isohashi, Fumiaki; Kuroda, Hiromasa; Sasano, Tomoyuki; Kimura, Tadashi (2015-01-01). "First two cases of primary carcinoma of the vagina successfully treated with concurrent weekly carboplatin plus paclitaxel, external beam radiotherapy and high-dose-rate interstitial brachytherapy: A case report and published work review". Journal of Obstetrics and Gynaecology Research. 41 (1): 156–161. doi:10.1111/jog.12492. ISSN 1447-0756.
- 1 2 "Vaginal cancer risk factors". Cancer Research UK. 2015-05-15. Archived from the original on 2017-12-14. Retrieved 2017-12-13.
- ↑ "List of Classifications by cancer sites with sufficient or limited evidence in humans, Volumes 1 to 120 a". World Health Organization, International Agency for Research on Cancer. 2017. Archived from the original on 25 June 2018. Retrieved 13 December 2017.
- 1 2 Society of Gynecologic Oncology (February 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, Society of Gynecologic Oncology, archived from the original on 1 December 2013, retrieved 19 February 2013
- ↑ Halperin, Edward C.; Brady, Luther W.; Perez, Carlos A.; Wazer, David E. (2013-05-06). Perez and Brady's principles and practice of radiation oncology. Halperin, Edward C.,, Brady, Luther W., 1925-, Wazer, David E.,, Perez, Carlos A., 1934- (Sixth ed.). Philadelphia. p. 1412. ISBN 9781451116489. OCLC 849739571.
- 1 2 "Vaginal Cancer Treatment". National Institutes of Health, National Cancer Institute. 9 February 2017. Archived from the original on 2019-04-09. Retrieved 2017-12-13.
- 1 2 "About DES". Centers for Disease Control and Prevention. Archived from the original on 2020-04-18. Retrieved 2017-12-13.
- ↑ "Known Health Effects for DES Daughters". Centers for Disease Control and Prevention. Archived from the original on 2017-12-14. Retrieved 2017-12-13.
- ↑ Damast, Shari; Takiar, Vinita; McCarthy, Shirley; Higgins, Susan A. (2016). "Treatment of early stage vaginal cancer with EBRT and MRI-based intracavitary brachytherapy: A retrospective case review". Gynecologic Oncology Reports. 17: 89–92. doi:10.1016/j.gore.2016.08.002. PMC 4975702. PMID 27536721.
- ↑ "Vaginal cancer | Vaginal cancer | Cancer Research UK". www.cancerresearchuk.org. Archived from the original on 2017-12-22. Retrieved 2017-12-19.
- ↑ "Vaginal cancer statistics". Cancer Research UK. 2015-05-14. Archived from the original on 2017-12-14. Retrieved 2017-12-13.
- ↑ "Unusual Cancers of Childhood Treatment". National Cancer Institute. 1980-01-01. Archived from the original on 2018-03-08. Retrieved 2018-03-09.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
External links
| Classification | |
|---|---|
| External resources |
- National Cancer Institute: Vaginal Cancer Archived 2013-12-27 at the Wayback Machine
- Vaginal cancer information from CRUK Archived 2021-08-27 at the Wayback Machine
- UK vaginal cancer statistics
- Cancer.Net: Vaginal cancer Archived 2013-12-27 at the Wayback Machine