Clear cell carcinoma of the uterine corpus
| Clear cell carcinoma of the uterine corpus | |
|---|---|
 | |
| Specialty | Gynecology, oncology |
| Symptoms | Abnormal vaginal bleeding[1] |
| Complications | Venous thromboembolism[1] |
| Usual onset | Females in their 60s[1] |
| Causes | Unknown[1] |
| Diagnostic method | Pap smear, histology, immunohistochemistry[1] |
| Differential diagnosis | Other type of endometrial cancer[1] |
| Prognosis | 5-year survival rate 55%-78%[1] |
| Frequency | Rare, less than 10% of all endometrial cancer[1] |
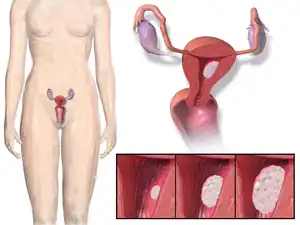
Clear cell carcinoma of the uterine corpus (CCC) is a type of endometrial cancer.[1] It typically presents with abnormal vaginal bleeding after menopause, but may be detected on a pap smear.[1]
The cause is not known.[1] On direct visualisation, it appears similar to other endometrial cancers, and breaks down easily to touch.[1] Under the microscope, the architecture is a mix of papillary, tubulocystic and solid pattern.[1] The tumor cells may have clear or eosinophilic cytoplasm, and typically show cuboidal, polygonal, hobnail, or flat appearance.[1] There are around four molecular subtypes, and the precursor lesion is unclear.[2] Complications include venous thromboembolism.[1]
CCC is rare, accounts for less than 10% of all endometrial cancer, and is more common in postmenopausal women.[1]
Diagnosis
The lesion is found in patients who present typically with abnormal or postmenopausal bleeding or discharge. Such bleeding is followed by further evaluation leading to a tissue diagnosis, usually done by a dilatation and curettage (D&C). A work-up to follow would look for metastasis using imaging technology including sonography and MRI. The median age at diagnosis in a large study was 66 years.[3]
Histopathology
Under the microscope, the architecture is a mix of papillary, tubulocystic and solid pattern.[1] The tumor cells may have clear or eosinophilic cytoplasm, and typically show cuboidal, polygonal, hobnail, or flat appearance.[1] There are four molecular subtypes; POLE mutations clear cell carcinomas, p53 abnormal clear cell carcinomas, NSMP (no specific molecular profile) clear cell ECs, and tumors that are a mix of clear cell and endometrioid components (mostly MMRd (MMR deficient)).[2]
Treatment and outcome
The primary treatment is surgical. FIGO-cancer staging is done at the time of surgery which consists of peritoneal cytology, total hysterectomy, bilateral salpingo-oophorectomy, pelvic/para-aortic lymphadenectomy, and omentectomy. The tumor is aggressive and spreads quickly into the myometrium and the lymphatic system. Thus even in presumed early stages, lymphadenectomy and omentectomy should be included in the surgical approach. If the tumor has spread surgery is cytoreductive followed by radiation therapy and/or chemotherapy.[3][4]
The five years survival is reported to be between 55% and 78%.[1] Increase age and late tumor stage give a poorer outcome.[1]
Staging
CCC is staged like other forms of endometrial carcinoma at time of surgery using the TNM staging system and the FIGO cancer staging.[1]
Epidemiology
CCC is rare, accounts for less than 10% of all endometrial cancer, and is more common in postmenopausal women.[1]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 WHO Classification of Tumours Editorial Board, ed. (2020). "6. Tumours of the uterine corpus:clear-cell carcinoma of the uterine corpus". Female genital tumours: WHO Classification of Tumours. Vol. 4 (5th ed.). Lyon (France): International Agency for Research on Cancer. pp. 258–259. ISBN 978-92-832-4504-9. Archived from the original on 2022-06-17. Retrieved 2022-07-30.
- 1 2 Huvila, Jutta; Pors, Jennifer; Thompson, Emily F.; Gilks, C. Blake (April 2021). "Endometrial carcinoma: molecular subtypes, precursors and the role of pathology in early diagnosis". The Journal of Pathology. 253 (4): 355–365. doi:10.1002/path.5608. ISSN 1096-9896. PMID 33368243. Archived from the original on 2022-06-15. Retrieved 2022-07-31.
- 1 2 C A Hamilton; M K Cheung; K Osann; L Chen; N N Teng; T A Longacre; M A Powell; M R Hendrickson; D S Kapp & J K Chan (Mar 2006). "Uterine papillary serous and clear cell carcinomas predict for poorer survival compared to grade 3 endometrioid corpus cancers". British Journal of Cancer. 94 (5): 642–6. doi:10.1038/sj.bjc.6603012. PMC 2361201. PMID 16495918.
- ↑ Stanojevic Z, Djordjevic B, Todorovska I, Lilic V, Zivadinovic R, Dunjic O (2008). "Risk factors and adjuvant chemotherapy in the treatment of endometrial cancer". J Buon. 13 (1): 23–30. PMID 18404782.
External links
| Classification |
|---|