Autism therapies
| Autism therapies | |
|---|---|
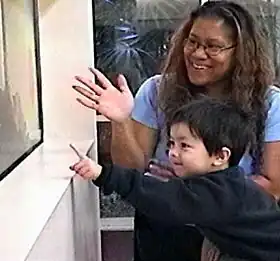 A three-year-old with autism points to fish in an aquarium, as part of an experiment (2004) on the effect of intensive shared-attention training on language development.[1] |
Autism therapies are a wide variety of therapies that attempt to improve the quality of life of autistic people and lessen the deficits and problematic behaviours colloquially associated with autism spectrum disorder (ASD). These methods of therapy also seek the increase of functional independence in autistic people. Autism can be described as social and language disability that is detected in most children as early as the of 18 months old. There is no known cause or cure for autism but treatment and therapies are suggested. None of these therapies eliminate autism within someone, let alone to a high degree of viability. Autistic children grow up to become autistic adults at risk of burnout and PTSD inflicted during childhood and adolescence, often overlooked by those who prioritize the elimination of autism over the common well being of autistic people. Treatment is typically catered to the person's needs. Treatments fall into two major categories: educational interventions and medical management. Training and support are also given to families of those with ASD.[2]
Studies of interventions have some methodological problems that prevent definitive conclusions about efficacy.[3] Although many psychosocial interventions have some positive evidence, suggesting that some form of treatment is preferable to no treatment, the systematic reviews have reported that the quality of these studies has generally been poor, their clinical results are mostly tentative, and there is little evidence for the relative effectiveness of treatment options.[4] Intensive, sustained special education programs and behavior therapy early in life can help children with ASD acquire self-care, social, and job skills,[2] and often can improve functioning, and decrease symptom severity and maladaptive behaviors;[5] Available approaches include applied behavior analysis (ABA), developmental models, structured teaching, speech and language therapy, social skills therapy, and occupational therapy.[2] Occupational therapists work with autistic children by creating interventions that promote social interaction like sharing and cooperation.[6] They also support the autistic child by helping them work through a dilemma as the OT imitates the child and waiting for a response from the child.[6] Educational interventions have some effectiveness in children: intensive ABA treatment has demonstrated effectiveness in enhancing global functioning in preschool children,[7] and is well established for improving intellectual performance of young children.[5] Neuropsychological reports are often poorly communicated to educators, resulting in a gap between what a report recommends and what education is provided.[8] The limited research on the effectiveness of adult residential programs shows mixed results.[9]
Many medications are used to treat problems associated with ASD.[10] More than half of U.S. children diagnosed with ASD are prescribed psychoactive drugs or anticonvulsants, with the most common drug classes being antidepressants, stimulants, and antipsychotics.[11] Aside from antipsychotics,[12] there is scant reliable research about the effectiveness or safety of drug treatments for adolescents and adults with ASD.[13][14] A person with ASD may respond atypically to medications, the medications can have adverse effects, and no known medication relieves autism's core symptoms of social and communication impairments.[15]
As of 2008 the treatments prescribed to children with ASD were expensive;[16] indirect costs are more so. For someone born in 2000, a U.S. study estimated an average discounted lifetime cost of $4.45 million (2022 dollars, inflation-adjusted from 2003 estimate[17]), with about 10% medical care, 30% extra education and other care, and 60% lost economic productivity.[18] A UK study estimated discounted lifetime costs at £1.83 million and £1.18 million for an autistic person with and without intellectual disability, respectively[19] (2022 pounds, inflation-adjusted from 2005/06 estimate[20]). Legal rights to treatment are complex, vary with location and age, and require advocacy by caregivers.[21] Publicly supported programs are often inadequate or inappropriate for a given child, and unreimbursed out-of-pocket medical or therapy expenses are associated with likelihood of family financial problems;[22] one 2008 U.S. study found a 14% average loss of annual income in families of children with ASD,[23] and a related study found that ASD is associated with higher probability that child care problems will greatly affect parental employment.[24] After childhood, key treatment issues include residential care, job training and placement, sexuality, social skills, and estate planning.[21]
Educational interventions
Educational interventions attempt to help children not only to learn academic subjects and gain traditional readiness skills, but also to improve functional communication and spontaneity, enhance social skills such as joint attention, develop cognitive skills such as symbolic play, reduce disruptive behavior, and generalize learned skills by applying them to new situations. Several program models have been developed, which in practice often overlap and share many features, including:[2]
- early intervention that is not dependent upon a definitive diagnosis;
- intense intervention, at least 25 hours per week, 12 months per year;
- low student/teacher ratio;
- family involvement, including training of parents;
- interaction with neurotypical peers;
- social stories, ABA and other visually based training;[25]
- structure that includes predictable routine and clear physical boundaries to lessen distraction; and
- ongoing measurement of a systematically planned intervention, resulting in adjustments as needed.
Several educational intervention methods are available, as discussed below. They can take place at home, at school, or at a center devoted to autism treatment; they can be implemented by parents, teachers, speech and language therapists, and occupational therapists.[2][6] A 2007 study found that augmenting a center-based program with weekly home visits by a special education teacher improved cognitive development and behavior.[26]
Studies of interventions have methodological flaws that prevent definitive conclusions about efficacy.[3] Although many psychosocial interventions have some positive evidence, suggesting that some form of treatment is preferable to no treatment, the methodological quality of systematic reviews of these studies has generally been poor, their clinical results are mostly tentative, and there is little evidence for the relative effectiveness of treatment options.[4] Concerns about outcome measures, such as their inconsistent use, most greatly affect how the results of scientific studies are interpreted.[27] A 2009 Minnesota study found that parents follow behavioral treatment recommendations significantly less often than they follow medical recommendations, and that they adhere more often to reinforcement than to punishment recommendations.[28] Intensive, sustained special education programs and behavior therapy early in life can help children acquire self-care, social, and job skills,[2] and often improve functioning and decrease symptom severity and maladaptive behaviors;[5] claims that intervention by around age three years is crucial are not substantiated.[29]
National Education Policies
U.S.
In the United States, there have been three major policies addressing special education in the United States. These policies were the Education for All Handicapped Children Act in 1975, the Individuals with Disabilities Education Act in 1997, and the No Child Left Behind in 2001. The development of those policies showed increased guidelines for special education and requirements; such as requiring states to fund special education, equality of opportunities, help with transitions after secondary schooling, requiring extra qualifications for special education teachers, and creating a more specific class setting for those with disabilities.[30][31][32] The Individuals with Disabilities Education Act, specifically had a large impact on special education as public schools were then required to employ high qualified staff. In 2009, for one to be a Certified Autism Specialist the requirements included: a master's degree, two years of career experience working with the autism population, earn 14 continuing education hours in autism every two years, and register with the International Institute of Education.[33]
Perceived disadvantages of Autistic people in the U.S. in the 2010's
Martha Nussbaum discusses how education is one of the fertile functions that is important for the development of a person and their ability to achieve a multitude of other capabilities within society.[34] Autism causes many symptoms that interfere with a child’s ability to receive a proper education such as deficits in imitation, observational learning, and receptive and expressive communication. As of 2014, of all disabilities affecting the population, autism ranked third lowest in acceptance into a postsecondary education institution.[35] In a 2012 study funded by the National Institute of Health, Shattuck et al. found that only 35% of autistics are enrolled in a 2 or 4 year college within the first two years after leaving high school compared to 40% of children who have a learning disability.[36] Due to the growing need for a college education to obtain a job, this statistic shows how autistics are at a disadvantage in gaining many of the capabilities that Nussbaum discusses and makes education more than just a type of therapy for those with autism.[35] According to the 2012 study by Shattuck, only 55% of children with autism participated in any paid employment within the first two years after high school. Furthermore, those with autism that come from low income families tend to have lower success in postsecondary schooling.[36]
Oftentimes, schools lacked the resources to create (what at the time was considered) an optimal classroom setting for those 'in need of special education'. In 2014 in the United States, it could cost between $6,595 to $10,421 extra to educate a child with autism.[37] In the 2011–2012 school year, the average cost of education for a public school student was $12,401. In 2015, some cases, the extra cost required to educate a child with autism nearly doubled the average cost to educate the average public school student.[38] As the range of those with autism can widely vary, it is very difficult to create an autism program that is well suited to the entire population of autistics as well as those with other disabilities. In the United States, in 2014 many school districts required schools to meet the needs of disabled students, regardless of the number of children with disabilities there are in the school.[39] This combined with a shortage of licensed special education teachers has created a deficiency in the special education system. in 2011 the shortage caused some states to give temporary special education licenses to teachers with the caveat that they receive a license within a few years.[40]
Mexico
In 1993, Mexico passed an education law that called for the inclusion of those with disabilities. This law was very important for Mexico education, however, there have been issues in implementing it due to a lack of resources.[41]
United Nations and Internationally
There have also been multiple international groups that have issued reports addressing issues in special education. The United Nations on “International Norms and Standards relating to Disability” in 1998. This report cites multiple conventions, statements, declarations, and other reports such as: The Universal Declaration of Human Rights, The Salamanca Statement, the Sundberg Declaration, the Copenhagen Declaration and Programme of Action, and many others. One main point that the report emphasizes is the necessity for education to be a human right. The report also states that the “quality of education should be equal to that of persons without disabilities.” The other main points brought up by the report discuss integrated education, special education classes as supplementary, teacher training, and equality for vocational education.[42] The United Nations also releases a report by the Special Rapporteur that has a focus on persons with disabilities. In 2015, a report titled “Report of the Special Rapporteur to the 52nd Session of the Commission for Social Development: Note by the Secretary-General on Monitoring of the implementation of the Standard Rules on the Equalization of Opportunities for Persons with Disabilities” was released. This report focused on looking at how the many countries involved, with a focus on Africa, have handled policy regarding persons with disabilities. In this discussion, the author also focuses on the importance of education for persons with disabilities as well as policies that could help improve the education system such as a move towards a more inclusive approach.[43] The World Health Organization has also published a report addressing people with disabilities and within this there is a discussion on education in their “World Report on Disability” in 201.[44] Other organizations that have issued reports discussing the topic are UNESCO, UNICEF, and the World Bank.[45]
Applied behavior analysis
Applied behavior analysis (ABA) is the applied research field of the science of behavior analysis, and it underpins a wide range of techniques used to treat autism and many other behaviors and diagnoses,[46] including those who are patients in rehab or in whom a behavior change is desired . ABA-based interventions focus on teaching tasks one-on-one using the behaviorist principles of stimulus, response and reward,[47] and on reliable measurement and objective evaluation of observed behavior.[2] There is wide variation in the professional practice of behavior analysis and among the assessments and interventions used in school-based ABA programs.[48] Conversely, various major figures within the autism community have written biographies detailing the harm caused by the provision of ABA, including restraint, sometimes used with mild self stimulatory behaviors such as hand flapping, and verbal abuse. The Autistic Self Advocacy Network campaigns against the use of ABA in autism.[49][50] – punishment procedures are very rarely used within the field today. These procedures were once used in the 70s and 80s however now there are ethical guidelines in place to prohibit the use.
Discrete trial training
Many intensive behavioral interventions rely heavily on discrete trial teaching (DTT) methods, which use stimulus-response-reward techniques to teach foundational skills such as attention, compliance, and imitation.[51] However, children have problems using DTT-taught skills in natural environments.[2] These students are also taught with naturalistic teaching procedures to help generalize these skills. In functional assessment, a common technique, a teacher formulates a clear description of a problem behavior, identifies antecedents, consequences, and other environmental factors that influence and maintain the behavior, develops hypotheses about what occasions and maintains the behavior, and collects observations to support the hypotheses.[2] A few more-comprehensive ABA programs use multiple assessment and intervention methods individually and dynamically.[48]
ABA-based techniques have demonstrated effectiveness in several controlled studies: children have been shown to make sustained gains in academic performance, adaptive behavior, and language, with outcomes significantly better than control groups.[2] A 2009 review of educational interventions for children, whose mean age was six years or less at intake, found that the higher-quality studies all assessed ABA, that ABA is well-established and no other educational treatment is considered probably efficacious, and that intensive ABA treatment, carried out by trained therapists, is demonstrated effective in enhancing global functioning in pre-school children.[7] These gains maybe complicated by initial IQ.[52] A 2008 evidence-based review of comprehensive treatment approaches found that ABA is well established for improving intellectual performance of young children with ASD.[5] A 2009 comprehensive synthesis of early intensive behavioral intervention (EIBI), a form of ABA treatment, found that EIBI produces strong effects, suggesting that it can be effective for some children with autism; it also found that the large effects might be an artifact of comparison groups with treatments that have yet to be empirically validated, and that no comparisons between EIBI and other widely recognized treatment programs have been published.[53] A 2009 systematic review came to the same principal conclusion that EIBI is effective for some but not all children, with wide variability in response to treatment; it also suggested that any gains are likely to be greatest in the first year of intervention.[29] A 2009 meta-analysis concluded that EIBI has a large effect on full-scale intelligence and a moderate effect on adaptive behavior.[54] However, a 2009 systematic review and meta-analysis found that applied behavior intervention (ABI), another name for EIBI, did not significantly improve outcomes compared with standard care of preschool children with ASD in the areas of cognitive outcome, expressive language, receptive language, and adaptive behavior.[55] Applied behavior analysis is cost effective for administrators [56]
Recently behavior analysts have built comprehensive models of child development (see Behavior analysis of child development) to generate models for prevention as well as treatment for autism.
Pivotal response training
Pivotal response treatment (PRT) is a naturalistic intervention derived from ABA principles. Instead of individual behaviors, it targets pivotal areas of a child's development, such as motivation, responsivity to multiple cues, self-management, and social initiations; it aims for widespread improvements in areas that are not specifically targeted. The child determines activities and objects that will be used in a PRT exchange. Intended attempts at the target behavior are rewarded with a natural reinforcer: for example, if a child attempts a request for a stuffed animal, the child receives the animal, not a piece of candy or other unrelated reinforcer.[57]
Communication interventions
The inability to communicate, verbally or non-verbally, is a core deficit in autism. Children with autism are often engaged in repetitive activity or other behaviors because they cannot convey their intent any other way. They do not know how to communicate their ideas to caregivers or others. Helping a child with autism learn to communicate their needs and ideas is absolutely core to any intervention. Communication can either be verbal or non-verbal. Children with autism require intensive intervention to learn how to communicate their intent.
Communication interventions fall into two major categories. First, many autistic children do not speak, or have little speech, or have difficulties in effective use of language.[58] Social skills have been shown to be effective in treating children with autism.[58] Interventions that attempt to improve communication are commonly conducted by speech and language therapists, and work on joint attention, communicative intent, and alternative or augmentative and alternative communication (AAC) methods such as visual methods,[59] for example visual schedules. AAC methods do not appear to impede speech and may result in modest gains.[60] A 2006 study reported benefits both for joint attention intervention and for symbolic play intervention,[61] and a 2007 study found that joint attention intervention is more likely than symbolic play intervention to cause children to engage later in shared interactions.[62]
Second, social skills treatment attempts to increase social and communicative skills of autistic individuals, addressing a core deficit of autism. A wide range of intervention approaches is available, including modeling and reinforcement, adult and peer mediation strategies, peer tutoring, social games and stories, self-management, pivotal response therapy, video modeling, direct instruction, visual cuing, Circle of Friends and social-skills groups.[63] A 2007 meta-analysis of 55 studies of school-based social skills intervention found that they were minimally effective for children and adolescents with ASD,[64] and a 2007 review found that social skills training has minimal empirical support for children with Asperger syndrome or high-functioning autism.[65]
SCERTS
The SCERTS model[66] is an educational model for working with children with autism spectrum disorder (ASD). It was designed to help families, educators and therapists work cooperatively together to maximize progress in supporting the child.
The acronym refers to the focus on:
- SC – social communication – the development of functional communication and emotional expression.
- ER – emotional regulation – the development of well-regulated emotions and ability to cope with stress.
- TS – transactional support – the implementation of supports to help families, educators and therapists respond to children's needs, adapt the environment and provide tools to enhance learning.
Relationship based, developmental models
Relationship based models give importance to the relationships that help children reach and master early developmental milestones. These are often missed or not mastered in children with ASD. Examples of these early milestones are engagement and interest in the world, intimacy with a caregiver, intentionality of action.
Relationship Development Intervention
Relationship development intervention[67] is a family-based treatment program for children with autism spectrum disorder (ASD). This program is based on the belief that the development of dynamic intelligence (the ability to think flexibly, take different perspectives, cope with change and process information simultaneously) is key to improving the quality of life of children with autism.
Son-Rise
Son-Rise is a home-based program that emphasizes on implementing a color- and sensory-free playroom. Before implementing the home-based program, an institute trains the parents how to accept their child without judgment through a series of dialogue sessions. Like Floortime, parents join their child's ritualistic behavior for relationship-building. To gain the child's "willing engagement", the facilitator continues to join them only this time through parallel play. Proponents claim that children will become non-autistic after parents accept them for who they are and engage them in play. The program was started by the parents of Raun Kaufman, who is claimed to have gone from being autistic to normal via the treatment in the early 1970s.[68] A stated goal of the program is to increase eye contact.[69] In a 2017 qualitative study it was found that autistic people have reported to find eye contact distressing.[70] No independent study has tested the efficacy of the program, but a 2003 study found that involvement with the program led to more drawbacks than benefits for the involved families over time,[71] and a 2006 study found that the program is not always implemented as it is typically described in the literature, which suggests it will be difficult to evaluate its efficacy.[72]
TEACCH
Treatment and Education of Autistic and Related Communication Handicapped Children (TEACCH), which has come to be called "structured teaching", emphasises structure by using organized physical environments, predictably sequenced activities, visual schedules and visually structured activities, and structured work/activity systems where each child can practice various tasks.[2] Parents are taught to implement the treatment at home. A 1998 controlled trial found that children treated with a TEACCH-based home program improved significantly more than a control group.[73] A 2013 meta-analysis compiling all the clinical trials of TEACCH indicated that it has small or no effects on perceptual, motor, verbal, cognitive, and motor functioning, communication skills, and activities of daily living. There were positive effects in social and maladaptive behavior, but these required further replication due to the methodological limitations of the pool of studies analysed.[74]
Sensory integration
Unusual responses to sensory stimuli are more common and prominent in children with autism, although there is not good evidence that sensory symptoms differentiate autism from other developmental disorders.[75] Several therapies have been developed to treat sensory processing disorder (SPD).[76] Some of these treatments (for example, sensorimotor handling) have a questionable rationale and have no empirical evidence. Other treatments have been studied, with small positive outcomes, but few conclusions can be drawn due to methodological problems with the studies. These treatments include prism lenses, physical exercise, auditory integration training, and sensory stimulation or inhibition techniques such as "deep pressure"—firm touch pressure applied either manually or via an apparatus such as a hug machine or a pressure garment.[77] Weighted vests, a popular deep-pressure therapy, have only a limited amount of scientific research available, which on balance indicates that the therapy is ineffective.[78] Although replicable treatments have been described and valid outcome measures are known, gaps exist in knowledge related to SPD and therapy.[79] In a 2011 Cochrane review, no evidence was found to support the use of auditory integration training as an ASD treatment method.[80] Because empirical support is limited, systematic evaluation is needed if these interventions are used.[81]
The term multisensory integration in simple terms means the ability to use all of ones senses to accomplish a task. Occupational therapists sometimes prescribe sensory treatments for children with Autism however in general there has been little or no scientific evidence of effectiveness.[77]
Animal-assisted therapy
Old model
Animal-assisted therapy, where an animal such as a dog or a horse becomes a basic part of a person's treatment, was a controversial treatment for some symptoms. A 2007 meta-analysis found that animal-assisted therapy was associated with "a moderate improvement in autism spectrum symptoms".[82] Reviews of published dolphin-assisted therapy (DAT) studies found important methodological flaws and concluded that there is no compelling scientific evidence that DAT is a legitimate therapy or that it affords any more than fleeting improvements in mood.[83]
New model
Modern animal-assisted therapy as relating to autism is not about 'controlling autistic symptoms' but about a natural way to bring about socializing[84] (via bridging the Double Empathy gap) and also for stress reduction.[85][86] As in a 2020 program: "the remarkable adherence to the therapy program by study participants and the program’s clinically relevant effects indicate that AAT with dogs can be used to reduce perceived stress and symptoms of agoraphobia, and to improve social awareness and communication in adults with ASD with normal to high intelligence."[87] In 2021, a study was conducted on this topic, specifically on "autonomic and endocrine activity in adults with autism spectrum disorder"[86] in part for stress reduction, particularly as for autistic people the "downside of social camouflaging is that it is a major source of stress".[86]
Neurofeedback
Neurofeedback attempts to train individuals to regulate their brainwave patterns by letting them observe their brain activity more directly. In its most traditional form, the output of EEG electrodes is fed into a computer that controls a game-like audiovisual display. Neurofeedback has been evaluated 'with positive results for ASD', but studies have lacked random assignment to controls.[88] This research is ongoing as of 2019 though now focused on "improving attention" and "reducing anxiety".[89]
Patterning
Patterning is a set of exercises that attempts to improve the organization of a child's neurologic impairments. It has been used for decades to treat children with several unrelated neurologic disorders, including autism. The method, taught at The Institutes for the Achievement of Human Potential, is based on oversimplified theories and is not supported by carefully designed research studies.[90]
Other methods
There are many simple methods such as priming, prompt delivery, picture schedules, peer tutoring, and cooperative learning, that have been proven to help autistic students to prepare for class and to understand the material better. Priming is done by allowing the students to see the assignment or material before they are shown in class. Prompt delivery consists of giving prompts to the autistic children in order to elicit a response to the academic material. Picture schedules are used to outline the progression of a class and are visual cues to allow autistic children to know when changes in the activity are coming up. This method has proven to be very useful in helping the students follow the activities. Peer tutoring and cooperative learning are ways in which an autistic student and a nonhandicapped student are paired together in the learning process. This has shown be very effective for “increasing both academic success and social interaction.”[91] There are more specific strategies that have been shown to improve an autistic’s education, such as LEAP, Treatment and Education of Autistic and Related Communication Handicapped Children, and Non-Model-Specific Special Education Programs for preschoolers. LEAP is “an intensive 12-month program that focuses on providing a highly structured and safe environment that helps students to participate in and derive benefit from educational programming” and focuses on children from 5-21 who have a more severe case of autism.[92] The goal of the program is to develop functional independence through academic instruction, vocational/translational curriculum, speech/language services, and other services personalized for each student.[92] While LEAP, TEACCH, and Non-Model Specific Special Education Programs are all different strategies, there has been no evidence that one is more effective than the other.[93]
Environmental enrichment
Environmental enrichment is concerned with how the brain is affected by the stimulation of its information processing provided by its surroundings (including the opportunity to interact socially). Brains in richer, more-stimulating environments, have increased numbers of synapses, and the dendrite arbors upon which they reside are more complex. This effect happens particularly during neurodevelopment, but also to a lesser degree in adulthood. With extra synapses there is also increased synapse activity and so increased size and number of glial energy-support cells. Capillary vasculation also is greater to provide the neurons and glial cells with extra energy. The neuropil (neurons, glial cells, capillaries, combined together) expands making the cortex thicker. There may also exist (at least in rodents) more neurons.
Research on nonhuman animals finds that more-stimulating environments could aid the treatment and recovery of a diverse variety of brain-related dysfunctions, including Alzheimer's disease and those connected to aging, whereas a lack of stimulation might impair cognitive development.
Research on humans suggests that lack of stimulation (deprivation—such as in old-style orphanages) delays and impairs cognitive development. Research also finds that higher levels of education (which is both cognitively stimulating in itself, and associates with people engaging in more challenging cognitive activities) results in greater resilience (cognitive reserve) to the effects of aging and dementia.
Massage therapy
A review of massage therapy as a symptomatic treatment of autism found limited evidence of benefit. There were few high quality studies, and due to the risk of bias found in the studies analyzed, no firm conclusions about the efficacy of massage therapy could be drawn.[94]
Music
Music therapy uses the elements of music to let people express their feelings and communicate. A 2014 review found that music therapy may help in social interactions and communication.[95]
Music therapy can involve various techniques depending on where the subject is sitting on the ASD scale.[96] Somebody who may be considered as 'low-functioning' would require vastly different treatment to somebody on the ASD scale who is 'high-functioning'. Examples of these types of therapeutic techniques include:[97]
- Free improvisation – No boundaries or skills required
- Structured improvisation – Some established parameters within the music
- Performing or recreating music – Reproducing a pre-composed piece of music or song with associated activities
- Composing music – Creating music that caters to the specific needs of that person using instruments or the voice
- Listening – Engaging in specific musical listening base exercises
Improvisational Music Therapy (IMT), is increasing in popularity as a therapeutic technique being applied to children with ASD. The process of IMT occurs when the client and therapist make up music, through the use of various instruments, song and movement. The specific needs of each child or client need to be taken into consideration. Some children with ASD find their different environments chaotic and confusing, therefore, IMT sessions require the presence of a certain routine and be predictable in nature, within their interactions and surroundings.[98] Music can provide all of this, it can be very predicable, it is highly repetitious with its melodies and sounds, but easily varied with phrasing, rhythm and dynamics giving it a controlled flexibility. The allowance of parents or caregivers to sessions can put the child at ease and allow for activities to be incorporated into everyday life.[98]
Sensory enrichment therapy
In all interventions for autistic children, the main strategy is to aim towards the improvement on sensitivity in all senses. Autistic children suffer from a lack of the ability to derive and sort out their senses as well as the feelings and moods of the people around them.[99] Many children with autism suffer from this Sensory Processing Disorder.[100] In sensory-based interventions, there have been signs of progress in children responding with an appropriate response when given a stimulus after being in sensory-based therapies for a period of time. However, at this time, there is no concrete evidence that these therapies are effective for children with Autism.[100] Autism is a very complex disorder and differs from child to child. This makes the effectiveness of each type of therapy and even therapy activity vary.
The purpose of these differentiated interventions are to intervene at the neurological level of the brain in hopes to develop appropriate responses to the different sensations from one's body and also to outside stimuli in one's environment. Scientist have used music therapies, massage therapies, occupational therapies and more. With the Autistic Spectrum being so diverse and widespread, each case or scenario is different.[77]
Mindfulness
Emerging evidence for mindfulness-based interventions for improving mental health in adults with autism has support through a recent systematic review. This includes evidence for decreasing stress, anxiety, ruminating thoughts, anger, and aggression.[101]
Parent-mediated interventions
Parent-mediated interventions offer support and practical advice to parents of autistic children.[59] A 2013 Cochrane Review found that there was no evidence of gains in most of the primary measures of the studies (e.g., the child's adaptive behaviour), however there was strong evidence for a positive pattern of change in parent-child interactions. There was some uncertain evidence of changes in the child's language and communication.[102] A very small number of randomized and controlled studies suggest that parent training can lead to reduced maternal depression, improved maternal knowledge of autism and communication style, and improved child communicative behavior, but due to the design and number of studies available, definitive evidence of effectiveness is not available.[103]
Early detection of ASD in children can often occur before a child reaches the age of three years old. Methods that target early behavior can influence the quality of life for a child with ASD. Parents can learn methods of interaction and behavior management to best assist their child's development. A 2013 Cochrance review concluded that there were some improvements when parent intervention was used.[104]
Medical management
Drugs, supplements, or diets are often used to alter physiology in an attempt to relieve common autistic symptoms such as seizures, sleep disturbances, irritability, and hyperactivity that can interfere with education or social adaptation or (more rarely) cause autistic individuals to harm themselves or others.[105] There is plenty of anecdotal evidence to support medical treatment; many parents who try one or more therapies report some progress, and there are a few well-publicized reports of children who are able to return to mainstream education after treatment, with dramatic improvements in health and well-being. However, this evidence may be confounded by improvements seen in autistic children who grow up without treatment, by the difficulty of verifying reports of improvements, and by the lack of reporting of treatments' negative outcomes.[106] Only a very few medical treatments are well supported by scientific evidence using controlled experiments.[105]
Medication
Many medications are used to treat problems associated with ASD.[10] More than half of U.S. children diagnosed with ASD are prescribed psychoactive drugs or anticonvulsants, with the most common drug classes being antidepressants, stimulants, and antipsychotics.[11] Only the antipsychotics have clearly demonstrated efficacy.[12]
Between the 1950s and 1970s LSD was studied, however, has not been studied in this capacity since.[107]
Research has focused on atypical antipsychotics, especially risperidone, which has the largest amount of evidence that consistently shows improvements in irritability, self-injury, aggression, and tantrums associated with ASD.[108] Risperidone is approved by the Food and Drug Administration (FDA) for treating symptomatic irritability in autistic children and adolescents.[12] In short-term trials (up to six months) most adverse events were mild to moderate, with weight gain, drowsiness, and high blood sugar requiring monitoring; long term efficacy and safety have not been fully determined.[109] It is unclear whether risperidone improves autism's core social and communication deficits.[12] The FDA's decision was based in part on a study of autistic children with severe and enduring problems of tantrums, aggression, and self-injury; risperidone is not recommended for autistic children with mild aggression and explosive behavior without an enduring pattern.[110]
Other drugs are prescribed off-label in the U.S., which means they have not been approved for treating ASD. Large placebo-controlled studies of olanzapine and aripiprazole were underway in early 2008.[12] Aripiprazole may be effective for treating autism in the short term, but is also associated with side effects, such as weight gain and sedation.[111]
Some selective serotonin reuptake inhibitors (SSRIs) and dopamine blockers can reduce some maladaptive behaviors associated with ASD.[112] Although SSRIs reduce levels of repetitive behavior in autistic adults,[113] a 2009 multisite randomized controlled study found no benefit and some adverse effects in children from the SSRI citalopram, raising doubts whether SSRIs are effective for treating repetitive behavior in autistic children.[114] A further study of related medical reviews determined that the prescription of SSRI antidepressants for treating autistic spectrum disorders in children lacked any evidence, and could not be recommended.[115]
Reviews of evidence found that the psychostimulant methylphenidate may be efficacious against hyperactivity and possibly impulsivity associated with ASD, although the findings were limited by low quality evidence.[116] There was no evidence that methylphenidate "has a negative impact on the core symptoms of ASD, or that it improves social interaction, stereotypical behaviours, or overall ASD."[116] Of the many medications studied for treatment of aggressive and self-injurious behavior in children and adolescents with autism, only risperidone and methylphenidate demonstrate results that have been replicated.[117]
A 1998 study of the hormone secretin reported improved symptoms and generated tremendous interest, but several controlled studies since have found no benefit.[118] An experimental drug STX107 has stopped overproduction of metabotropic glutamate receptor 5 in rodents, and it has been hypothesized that this may help in about 5% of autism cases, but this hypothesis has not been tested in humans.[119]
Oxytocin may play a role in autism and may be a possible treatment for repetitive and affiliative behaviors;[120] Two related studies in adults found that oxytocin decreased repetitive behaviors and improved interpretation of emotions, but these preliminary results do not necessarily apply to children.[119] Recent research suggests that oxytocin may decrease the noisiness of the brain's auditory system, increasing perception of social cues and the ability to react in social situations. However, the cues detected may not always be positive: increasing awareness of a trusted adult may be beneficial, but increasing awareness of an aggressor may increase distress. The possibility that oxytocin's effects are context-dependent means that its use as a treatment in autism-spectrum disorder should be carefully monitored.[121][122]
Aside from antipsychotics,[12] there is scant reliable research about the effectiveness or safety of drug treatments for adolescents and adults with ASD.[13] Results of the handful of randomized controlled trials that have been performed suggest that risperidone, the SSRI fluvoxamine, and the typical antipsychotic haloperidol may be effective in reducing some behaviors, that haloperidol may be more effective than the tricyclic antidepressant clomipramine, and that the opioid antagonist naltrexone hydrochloride is not effective.[14] In small studies, memantine has been shown to significantly improve language function and social behavior in children with autism.[123][124] Research is underway on the effects of memantine in adults with autism spectrum disorders.[125] A person with ASD may respond atypically to medications and the medications can have adverse side effects.[15][126]
Prosthetics
Unlike conventional neuromotor prostheses, neurocognitive prostheses would sense or modulate neural function in order to physically reconstitute cognitive processes such as executive function and language. No neurocognitive prostheses are currently available but the development of implantable neurocognitive brain-computer interfaces has been proposed to help treat conditions such as autism.[127]
Affective computing devices, typically with image or voice recognition capabilities, have been proposed to help autistic individuals improve their social communication skills.[128] These devices are still under development. Robots have also been proposed as educational aids for autistic children.[129]
Transcranial magnetic stimulation
Transcranial magnetic stimulation, which is a somewhat well established treatment for depression, has been proposed, and used, as a treatment for autism.[130] A review published in 2013 found insufficient evidence to support its widespread use for autism spectrum disorders.[131] A 2015 review found tentative but insufficient evidence to justify its use outside of clinical studies.[132]
Alternative medicine
Many alternative therapies and interventions used to be popular in the 1990s and early 2000s, ranging from elimination diets to chelation therapy, though few were supported by scientific studies.[133][134][65][135][136] Treatment approaches lacked empirical support in quality-of-life contexts, and many programs focused on success measures that lack predictive validity and real-world relevance.[137] Scientific evidence appeared to matter less to service providers than program marketing, training availability, and parent requests.[138] Back then, it was presumed that even if they did not help, conservative treatments such as changes in diet were "expected to be harmless aside from their bother and cost"[139] except that didn't take into account the mental health toll that attitude would have on the children in question who are now adults speaking out against such practices.[140]
Acupuncture
Acupuncture was studied and has not been found to be 'helpful in treating autism'.[141][142]
Hyperbaric oxygen

In 2007 further studies were needed in order for practitioners and families to make more conclusive and valid decisions concerning HBOT treatments.[143] One small 2009 double-blind study of autistic children found that 40 hourly treatments of 24% oxygen at 1.3 atmospheres provided significant improvement in the children's behavior immediately after treatment sessions but this study has not been independently confirmed.[144] This spawned a relatively large-scale controlled studies since to investigate HBOT. For example in 2010 using treatments of 24% oxygen at 1.3 atmospheres, though it found less promising results. A 2010 double-blind study compared HBOT to a placebo treatment in children with autistic disorder. Both direct observational measures of behavioral symptoms and standardized psychological assessments were used to evaluate the treatment. No differences were found between the HBOT group and the placebo group on any of the outcome measures.[145] A second 2011 single-subject design study also investigated the effects of 40 HBOT treatments of 24% oxygen at 1.3 atmospheres on directly observed behaviors using multiple baselines across 16 participants. Again, no consistent outcomes were observed across any group and further, no significant improvements were observed within any individual participant.[146] Together, these studies suggest that HBOT at 24% oxygen at 1.3 atmospheric pressure does not result in a clinically significant improvement of the behavioral symptoms of autistic disorder. Nonetheless, news reports and related blogs indicated that HBOT was used for many cases of children with autism in the 2010s.
When considering the financial and time investments required in order to participate in this treatment and the inconsistency of the present findings, HBOT seems to be a riskier and thus, often less favorable. As of May 2011 HBOT could cost up to $150 per hour with individuals using anywhere from 40 to 120 hours as a part of their integrated treatment programs. In addition, purchasing (at $8,495–27,995) and renting ($1,395 per month) of the HBOT chambers is another option some families use.[146]
As of 2017, "Hyperbaric oxygen therapy provides a higher concentration of oxygen delivered in a chamber or tube containing higher than sea level atmospheric pressure. Case series and randomized controlled trials show no evidence to support the benefit of HBOT for children with ASD. Only 1 randomized controlled trial reported effectiveness of this treatment, and those results have yet to be repeated."[147]
Chiropractic
Chiropractic is an alternative medical practice whose main hypothesis is that mechanical disorders of the spine affect general health via the nervous system, and whose main treatment is spinal manipulation. A significant portion of the profession rejects vaccination, as traditional chiropractic philosophy equates vaccines to poison.[148] Most chiropractic writings on vaccination focus on its negative aspects,[149] claiming that it is hazardous, ineffective, and unnecessary,[148] and in some cases suggesting that vaccination causes autism[149] or that chiropractors should be the primary contact for treatment of autism and other neurodevelopmental disorders.[150] Chiropractic treatment has not been shown to be effective for medical conditions other than back pain,[151] and there is insufficient scientific evidence to make conclusions about chiropractic care for autism.[152]
Craniosacral therapy
Craniosacral therapy is an alternative medical practice whose main hypothesis is that restrictions at cranial sutures of the skull affect rhythmic impulses conveyed via cerebrospinal fluid, and that gentle pressure on external areas can improve the flow and balance of the supply of this fluid to the brain, relieving symptoms of many conditions.[153] There is no scientific support for major elements of the underlying model,[154] there is little scientific evidence to support the therapy, and research methods that could conclusively evaluate the therapy's effectiveness have not been applied.[153] No published studies are available on the use of this therapy for autism.[133]
Chelation therapy
Based on the speculation that heavy metal poisoning may trigger the symptoms of autism, particularly in small subsets of individuals who cannot excrete toxins effectively, some parents have turned to alternative medicine practitioners who provide detoxification treatments via chelation therapy. However, evidence to support this practice has been anecdotal and not rigorous. Strong epidemiological evidence refutes links between environmental triggers, in particular thiomersal-containing vaccines, and the onset of autistic symptoms. In 2002 Thiamine tetrahydrofurfuryl disulfide (TTFD) was hypothesized to act as a chelating agent in children with autism and a 2002 pilot study administered TTFD rectally to ten autism spectrum children, and seemed to find beneficial clinical effect.[155] This study has not been replicated, and a 2006 review of thiamine by the same author did not mention thiamine's possible effect on autism.[156] There is not sufficient evidence to support the use of thiamine (vitamin B1) to treat autism.[134] Dubious invasive treatments are a much more serious matter: for example, in 2005, botched chelation therapy killed a five-year-old boy with autism.[157]
No scientific data supports the claim that the mercury in the vaccine preservative thiomersal causes autism[158] or its symptoms,[159] and there is no scientific support for chelation therapy as a treatment for autism.[160][161]
Diets and Dietary Supplements
1990's hypotheses
In the early 1990s, it was hypothesized that autism could be caused or aggravated by opioid peptides like casomorphine that are metabolic products of gluten and casein.[162] Based on that hypothesis, diets that eliminate foods containing either gluten or casein, or both, are widely promoted, and many testimonials can be found describing benefits in autism-related symptoms, notably social engagement and verbal skills. Studies supporting those claims had significant flaws, so those data were inadequate to guide treatment recommendations.[139][163] Vitamin C decreased stereotyped behavior in a small 1993 study.[164] The study had not been replicated as of 2005, and vitamin C had limited popularity as an autism treatment. High doses might cause kidney stones or gastrointestinal upset such as diarrhea.[105]
2000-2014 hypotheses and research
In the early 2000's, many parents gave their children dietary supplements in an attempt to 'treat autism' or to 'alleviate its symptoms'. The range of supplements given was wide and few are supported by scientific data.[134][105]
In 2005, it was thought that: although some children with autism also have gastrointestinal (GI) symptoms, there is a lack of published rigorous data to support the theory that autistic children have more or different GI symptoms than usual;[165] studies report conflicting results, and the relationship between GI problems and ASD is unclear.[2] Atypical eating behavior was thought to occur in about three-quarters of children with ASD, to the extent that it was formerly a diagnostic indicator. Selectivity is the most common problem, although eating rituals and food refusal also occur;[166] at the time it did not appear to result in malnutrition in studies. Other elimination diets were also proposed, targeting salicylates, food dyes, yeast, and simple sugars. No scientific evidence has established the efficacy of such diets in 'treating autism' in children. An elimination diet may create nutritional deficiencies that harm overall health unless care is taken to assure proper nutrition.[134]
In 2006 studies suggested that complementary and alternative medical (CAM) therapy use in children with chronic illnesses is higher than in children in the general population. In a study by Helen H L Wong and Ronald G Smith, they investigated patterns of CAM therapy use in children diagnosed with autism spectrum disorders (ASD, n = 50) as compared to a control population of children with no ASD (n = 50). Over half of the parents in the ASD group reported using, or had used at least one CAM therapy for their child (52%) as compared to 28% of the control group (P = 0.024). Seventy percent of therapies used in the ASD group were biologically based therapies consisting of special diets or supplements, and parents felt that 75% of the therapies used were beneficial.[167]
For example, a 2008 study found that autistic boys on casein-free diets had significantly thinner bones than usual, presumably because the diets contribute to calcium and vitamin D deficiencies.[168] A 2009 review found some low-quality evidence to support the use of vitamin B6 in combination with magnesium at high doses, but the evidence was equivocal and the review noted the possible danger of fatal hypermagnesemia.[169] A 2005 Cochrane Review of the evidence for the use of B6 and magnesium found that "[d]ue to the small number of studies, the methodological quality of studies, and small sample sizes, no recommendation can be advanced regarding the use of B6-Mg as a treatment for autism."[170]
Probiotics containing potentially beneficial bacteria were hypothesized to 'relieve some symptoms of autism' by minimizing yeast overgrowth in the colon. The hypothesized yeast overgrowth has not been confirmed by endoscopy, the mechanism connecting yeast overgrowth to autism is only hypothetical, and no clinical trials as of 2005 had been published in the peer-reviewed literature.[105]
Dimethylglycine (DMG) was hypothesized to improve speech and 'reduce autistic behaviors',[134] and was a commonly used supplement.[105] Two double-blind, placebo-controlled studies found no statistically significant effect on 'autistic behaviors',[134] and no peer-reviewed studies have addressed treatment with the related compound trimethylglycine.[105]
Melatonin is sometimes used to manage sleep problems. Adverse effects were generally reported to be mild, including drowsiness, headache, dizziness, and nausea; however, an increase in seizure frequency was reported among susceptible children.[134] Several small RCTs indicated that melatonin was effective in treating insomnia in autistic children, but further large studies are needed.[171] A 2013 literature review found 20 studies that reported improvements in sleep parameters as a result of melatonin supplementation, and concluded that "the administration of exogenous melatonin for abnormal sleep parameters in ASD is evidence-based."[172]
Although omega-3 fatty acids, which are polyunsaturated fatty acids (PUFA), were 'a popular treatment for children with ASD' in the 2000's and 2010's, there is very little high-quality scientific evidence supporting their effectiveness.[173][174] Several other supplements were hypothesized 'to relieve autism symptoms', including BDTH2,[175] carnosine, cholesterol,[176] cyproheptadine, D-cycloserine, folic acid, glutathione, metallothionein promoters, other PUFA such as omega-6 fatty acids, tryptophan, tyrosine, thiamine (see Chelation therapy), vitamin B12, and zinc. These lack reliable scientific evidence of efficacy or safety in treatment of autism.[134][105]
2015–Present research
It is now known that "children with ASD are at risk of having alimentary tract disorders – mainly, they are at a greater risk of general gastrointestinal (GI) concerns, constipation, diarrhea, and abdominal pain"[177][178][179] and as succinctly summarized the Mayo Clinic website in 2019, "Yes, children with autism spectrum disorder (ASD) tend to have more medical issues, including gastrointestinal (GI) symptoms such as abdominal pain, constipation and diarrhea, compared with their peers."[180] Presently, there is not 'a diet for autism' just advice to not ingest things the individual's body seems to reject, for example: gluten if the person happens to have Celiac disease.[140] As of 2021, "there is no clinical evidence for applying specific (e.g., gluten-free or pro-biotic) diets" to the topic of autism.[181]
Electroconvulsive therapy
In 2009 studies indicated that 12–17% of adolescents and young adults with autism satisfy diagnostic criteria for catatonia, which is loss of or hyperactive motor activity. Electroconvulsive therapy (ECT) have been used to treat cases of catatonia and related conditions in people with autism but as of 2009 no controlled trials had been performed of ECT in autism, and there are serious ethical and legal obstacles to its use.[182]
Stem cell therapy
2007-2012
Mesenchymal stem cells and cord blood CD34+ cells have been proposed to treat autism in 2007[183] and as of 2012 it was thought they may represent a future treatment.[184] Since immune system deregulation has been implicated in autism, mesenchymal stem cells show the greatest promise as treatment for the disorder. Changes in the innate and adaptive immune system have been observed- those with autism show an imbalance in CD3+, CD4+, and CD8+ T cells, as well as in NK cells.[185] In addition, peripheral blood mononuclear cells (PBMCs) overproduce IL-1β.[185] It was theorized that MSC mediated immune suppressive activity could restore this immune imbalance.
Other
Pseudoscience
A number of naturopathic practitioners claim that CEASE therapy, a mixture of homeopathy, supplements and 'vaccine detoxing', can help people with autism however no robust evidence is available for this.
Packing
In packing, children were wrapped tightly for up to an hour in wet sheets that have been refrigerated, with only their heads left free. The treatment was repeated several times a week, and could continue for years. It was intended as treatment for autistic children who harm themselves and mostly children who could not speak. Similar envelopment techniques had been used for centuries, such as to calm violent patients in Germany in the 19th century; it was re-popularized in France in the 1960s, based on psychoanalytic theories such as the theory of the refrigerator mother. As of 2007, packing was used in hundreds of French clinics. There was no scientific evidence for the effectiveness of packing in 2007, and there was some concern about risk of adverse health effects.[186] As of 2019: "The main French associations of parents with autistic children succeeded in obtaining the prohibition of packing, announced by the French Secretary of State to the Ministry of Health in April 2016."[187]
Religious abuse as treatment
Exorcism
The Table Talk of Martin Luther contains the story of a twelve-year-old boy who some believe was 'severely autistic'.[188] According to Luther's notetaker Mathesius, Luther thought the boy was a soulless mass of flesh possessed by the devil, and suggested that he be suffocated.[189]
In 2003, an autistic boy in Wisconsin suffocated during an exorcism by an Evangelical minister in which he was wrapped in sheets.[190][191]
Ultraorthodox Jewish parents in Israel sometimes used spiritual and mystical interventions such as prayers, blessings, recitations of religious text, amulets, changing the child's name, and exorcism.[192]
Shaming / Other
A 2009 study has suggested that spirituality of mothers with autistic spectrum disorders led to positive outcomes whereas religious activities of mothers were associated with negative outcomes for the child.[193]
Historical outlooks
U.S., U.K., and France
Children in Britain and America would often be put in institutions on the instruction of doctors and the parents told to forget about them, for example, "in Britain, until 1961, almost all doctors regarded these symptoms as part of some general "childhood psychosis" or junior version of schizophrenia".[194] Observer journalist Christopher Stevens, father of an autistic child, reports how a British doctor told him that after a child was admitted to such an institution, usually "nature would take its course" and the child would die due to the prevalence of tuberculosis.[195]
Anti-cure perspective and Autism rights movement
The exact cause of autism is unclear, yet some organizations advocate researching a cure. Many self-advocacy autism rights organizations such as Autistic Self Advocacy Network view autism as a different neurology rather than as a mental disorder, advocate acceptance, and are against ABA as it is seen as trying to force conformity to "neuronormative" society.[196][197]
Criticisms of most educational, social, and behavioral focused autism therapies as put forth by autistic adults, teachers, and researchers frequently fall into the idea of these programs encouraging[198] or even training behavioral responses directed toward "camouflaging",[199][200][201][202][203][204][205][206] "passing as non-autistic",[198][207][208] or "masking".[206][209][210][211][212][213][204][214][215] Recent studies indicate that, among autistic people, burnout[216][217] "driven by the stress of masking and living in an unaccommodating neurotypical world"[218][219] is an issue (which also impacts autistic young people.[220] and children)[221] Animal-assisted therapy used to be directed toward symptoms of autism and some studies of the programs are now directed toward burnout.[86]
In 2018 more studies began involving the experiences of autistic adults[222][223] including their experiences with general practice medicine.[224] Subsequent related studies have focused on communication preferences of autistic adults[225] and the idea of "the ‘Autistic Advantage', a strengths-based model".[226][227][228]
See also
References
- ↑ Powell K (August 2004). "Opening a window to the autistic brain". PLOS Biology. 2 (8): E267. doi:10.1371/journal.pbio.0020267. PMC 509312. PMID 15314667.
- 1 2 3 4 5 6 7 8 9 10 11 12 Myers SM, Johnson CP (November 2007). "Management of children with autism spectrum disorders". Pediatrics. 120 (5): 1162–82. doi:10.1542/peds.2007-2362. PMID 17967921. S2CID 1656920. Lay summary – AAP (2007-10-29).
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - 1 2 Ospina MB, Krebs Seida J, Clark B, Karkhaneh M, Hartling L, Tjosvold L, et al. (2008). "Behavioural and developmental interventions for autism spectrum disorder: a clinical systematic review". PLOS ONE. 3 (11): e3755. Bibcode:2008PLoSO...3.3755O. doi:10.1371/journal.pone.0003755. PMC 2582449. PMID 19015734.
- 1 2 Seida JK, Ospina MB, Karkhaneh M, Hartling L, Smith V, Clark B (February 2009). "Systematic reviews of psychosocial interventions for autism: an umbrella review". Developmental Medicine and Child Neurology. 51 (2): 95–104. doi:10.1111/j.1469-8749.2008.03211.x. PMID 19191842. S2CID 39383638.
- 1 2 3 4 Rogers SJ, Vismara LA (January 2008). "Evidence-based comprehensive treatments for early autism". Journal of Clinical Child and Adolescent Psychology. 37 (1): 8–38. doi:10.1080/15374410701817808. PMC 2943764. PMID 18444052.
- 1 2 3 Case-Smith J, Arbesman M (2008-07-01). "Evidence-based review of interventions for autism used in or of relevance to occupational therapy". The American Journal of Occupational Therapy. 62 (4): 416–29. doi:10.5014/ajot.62.4.416. PMID 18712004.
- 1 2 Eikeseth S (2009). "Outcome of comprehensive psycho-educational interventions for young children with autism". Research in Developmental Disabilities. 30 (1): 158–78. doi:10.1016/j.ridd.2008.02.003. PMID 18385012.
- ↑ Kanne SM, Randolph JK, Farmer JE (December 2008). "Diagnostic and assessment findings: a bridge to academic planning for children with autism spectrum disorders". Neuropsychology Review. 18 (4): 367–84. doi:10.1007/s11065-008-9072-z. PMID 18855144. S2CID 21108225.
- ↑ Van Bourgondien ME, Reichle NC, Schopler E (April 2003). "Effects of a model treatment approach on adults with autism". Journal of Autism and Developmental Disorders. 33 (2): 131–40. doi:10.1023/A:1022931224934. PMID 12757352. S2CID 30125359.
- 1 2 Leskovec TJ, Rowles BM, Findling RL (2008). "Pharmacological treatment options for autism spectrum disorders in children and adolescents". Harvard Review of Psychiatry. 16 (2): 97–112. doi:10.1080/10673220802075852. PMID 18415882. S2CID 26112061.
- 1 2 Medications for U.S. children with ASD:
- Oswald DP, Sonenklar NA (June 2007). "Medication use among children with autism spectrum disorders". Journal of Child and Adolescent Psychopharmacology. 17 (3): 348–55. doi:10.1089/cap.2006.17303. PMID 17630868.
- Mandell DS, Morales KH, Marcus SC, Stahmer AC, Doshi J, Polsky DE (March 2008). "Psychotropic medication use among Medicaid-enrolled children with autism spectrum disorders". Pediatrics. 121 (3): e441-8. doi:10.1542/peds.2007-0984. PMC 2861431. PMID 18310165.
- 1 2 3 4 5 6 Posey DJ, Stigler KA, Erickson CA, McDougle CJ (January 2008). "Antipsychotics in the treatment of autism". The Journal of Clinical Investigation. 118 (1): 6–14. doi:10.1172/JCI32483. PMC 2171144. PMID 18172517.
- 1 2 Angley M, Young R, Ellis D, Chan W, McKinnon R (September 2007). "Children and autism--Part 1--recognition and pharmacological management" (PDF). Australian Family Physician. 36 (9): 741–4. PMID 17915375. Archived from the original (PDF) on 2007-10-25.
- 1 2 Broadstock M, Doughty C, Eggleston M (July 2007). "Systematic review of the effectiveness of pharmacological treatments for adolescents and adults with autism spectrum disorder". Autism. 11 (4): 335–48. doi:10.1177/1362361307078132. PMID 17656398. S2CID 42629626.
- 1 2 Buitelaar JK (2003). "Why have drug treatments been so disappointing?". Autism: Neural Basis and Treatment Possibilities. Novartis Foundation Symposia. Vol. 251. pp. 235–44, discussion 245–9, 281–97. doi:10.1002/0470869380.ch14. ISBN 978-0-470-85099-2. PMID 14521196.
- ↑ Shimabukuro TT, Grosse SD, Rice C (March 2008). "Medical expenditures for children with an autism spectrum disorder in a privately insured population". Journal of Autism and Developmental Disorders. 38 (3): 546–52. doi:10.1007/s10803-007-0424-y. PMID 17690969. S2CID 38290838.
- ↑ 1634–1699: McCusker, J. J. (1997). How Much Is That in Real Money? A Historical Price Index for Use as a Deflator of Money Values in the Economy of the United States: Addenda et Corrigenda (PDF). American Antiquarian Society. 1700–1799: McCusker, J. J. (1992). How Much Is That in Real Money? A Historical Price Index for Use as a Deflator of Money Values in the Economy of the United States (PDF). American Antiquarian Society. 1800–present: Federal Reserve Bank of Minneapolis. "Consumer Price Index (estimate) 1800–". Retrieved January 1, 2020.
- ↑ Ganz ML (April 2007). "The lifetime distribution of the incremental societal costs of autism". Archives of Pediatrics & Adolescent Medicine. 161 (4): 343–9. doi:10.1001/archpedi.161.4.343. PMID 17404130. Lay summary – Harvard School of Public Health (2006-04-25).
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - ↑ Knapp M, Romeo R, Beecham J (May 2009). "Economic cost of autism in the UK". Autism. 13 (3): 317–36. doi:10.1177/1362361309104246. PMID 19369391. S2CID 20093805. Lay summary – ScienceDaily (2009-05-18).
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - ↑ UK Retail Price Index inflation figures are based on data from Clark, Gregory (2017). "The Annual RPI and Average Earnings for Britain, 1209 to Present (New Series)". MeasuringWorth. Retrieved December 2, 2021.
- 1 2 Aman MG (2005). "Treatment planning for patients with autism spectrum disorders". The Journal of Clinical Psychiatry. 66 (Suppl 10): 38–45. PMID 16401149.
- ↑ Sharpe DL, Baker DL (2007). "Financial issues associated with having a child with autism". Journal of Family and Economic Issues. 28 (2): 247–64. doi:10.1007/s10834-007-9059-6. S2CID 145663530.
- ↑ Montes G, Halterman JS (April 2008). "Association of childhood autism spectrum disorders and loss of family income". Pediatrics. 121 (4): e821-6. doi:10.1542/peds.2007-1594. PMID 18381511. S2CID 55179.
- ↑ Montes G, Halterman JS (July 2008). "Child care problems and employment among families with preschool-aged children with autism in the United States". Pediatrics. 122 (1): e202-8. doi:10.1542/peds.2007-3037. PMID 18595965. S2CID 22686553.
- ↑ Mitelman S, Von Kohorn O (September 2012). "Social Signals – Mike's Crush". American Journal of Sexuality Education. 7 (3): 282–284. doi:10.1080/15546128.2012.707095. S2CID 144245708.
- ↑ Rickards AL, Walstab JE, Wright-Rossi RA, Simpson J, Reddihough DS (August 2007). "A randomized, controlled trial of a home-based intervention program for children with autism and developmental delay". Journal of Developmental and Behavioral Pediatrics. 28 (4): 308–16. doi:10.1097/DBP.0b013e318032792e. PMID 17700083. S2CID 39987661.
- ↑ Wheeler D, Williams K, Seida J, Ospina M (2008). "The Cochrane Library and Autism Spectrum Disorder: an overview of reviews". Evidence-Based Child Health. 3 (1): 3–15. doi:10.1002/ebch.218. Archived from the original on 2012-12-10.
- ↑ Moore TR, Symons FJ (August 2009). "Adherence to behavioral and medical treatment recommendations by parents of children with autism spectrum disorders". Journal of Autism and Developmental Disorders. 39 (8): 1173–84. doi:10.1007/s10803-009-0729-0. PMID 19333747. S2CID 20631596.
- 1 2 Howlin P, Magiati I, Charman T (January 2009). "Systematic review of early intensive behavioral interventions for children with autism". American Journal on Intellectual and Developmental Disabilities. 114 (1): 23–41. doi:10.1352/2009.114:23-41. PMID 19143460.
- ↑ Education for All Handicapped Children Act of 1975
- ↑ Individuals with Disabilities Education Act of 1997
- ↑ No Child Left Behind Act of 2001
- ↑ "Standards". International Institute of Education Standards, Inc. Archived from the original on 13 September 2009.
- ↑ Nussbaum M (2009). Creating Capabilities: The Human Development Approach. Belknap Press of Harvard University Press. pp. 17–45. ISBN 978-0-674-07235-0.
- 1 2 Fleury VP, Hedges S, Hume K, Browder DM, Thompson JL, Fallin K, et al. (2014-03-01). "Addressing the Academic Needs of Adolescents With Autism Spectrum Disorder in Secondary Education". Remedial and Special Education. 35 (2): 68–79. doi:10.1177/0741932513518823. ISSN 1538-4756. S2CID 145044525.
- 1 2 Shattuck PT, Narendorf SC, Cooper B, Sterzing PR, Wagner M, Taylor JL (June 2012). "Postsecondary education and employment among youth with an autism spectrum disorder". Pediatrics. 129 (6): 1042–9. doi:10.1542/peds.2011-2864. PMC 3362908. PMID 22585766.
- ↑ Lavelle TA, Weinstein MC, Newhouse JP, Munir K, Kuhlthau KA, Prosser LA (March 2014). "Economic burden of childhood autism spectrum disorders". Pediatrics. 133 (3): e520-9. doi:10.1542/peds.2013-0763. PMC 7034397. PMID 24515505.
- ↑ "The Condition of Education 2015". 2015-05-28. Retrieved 2015-11-10.
- ↑ Wall P (2014-08-11). "Special-education overhaul leaves students less isolated, but schools struggle to keep up". Chalkbeat New York. Retrieved 2015-11-10.
- ↑ "The Need Grows for Special Education Teachers in the U.S." CFNC. 2011. Retrieved 2015-11-10.
- ↑ Tuman JP, Roth-Johnson D, Baker DL, Vecchio J (2010-03-26). Autism and Special Education Policy in Mexico. SSRN 1578963.
- ↑ "UN Enable – Compilation of International Norms And Standards Relating to Disability". United Nations Enable. July 2002. Retrieved 2015-11-10.
- ↑ "Special Rapporteur on Disability of the Commission for Social Development". 2015. Archived from the original on 2015-07-07. Retrieved 2015-11-10.
- ↑ World report on disability. Geneva, Switzerland: World Health Organization. 2011. ISBN 978-92-4-156418-2.
- ↑ "Global Reports". Archived from the original on 2015-11-19. Retrieved 2015-11-10.
- ↑ Dillenburger K, Keenan M (June 2009). "None of the As in ABA stand for autism: dispelling the myths". Journal of Intellectual & Developmental Disability. 34 (2): 193–5. doi:10.1080/13668250902845244. PMID 19404840. S2CID 1818966.
- ↑ Howard JS, Sparkman CR, Cohen HG, Green G, Stanislaw H (2005). "A comparison of intensive behavior analytic and eclectic treatments for young children with autism". Research in Developmental Disabilities. 26 (4): 359–83. doi:10.1016/j.ridd.2004.09.005. PMID 15766629.
- 1 2 Steege MW, Mace FC, Perry L, Longenecker H (2007). "Applied behavior analysis: beyond discrete trial teaching". Psychology in the Schools. 44 (1): 91–9. doi:10.1002/pits.20208.
- ↑ Autistic Self Advocacy Network. "Autistic Self Advocacy Network – Nothing About Us Without Us". www.autisticadvocacy.org.
- ↑ DeVita-Raeburn E (2016-08-11). "Is the Most Common Therapy for Autism Cruel?". The Atlantic.
- ↑ Ryan CS, Hemmes NS (2005). "Post-training Discrete-Trial Teaching Performance by Instructors of Young Children with Autism in Early Intensive Behavioral Intervention". The Behavior Analyst Today. 6 (1): 1–16. doi:10.1037/h0100052.
- ↑ Weiss MJ, Delmolino L (2006). "The Relationship Between Early Learning Rates and Treatment Outcome For Children With Autism Receiving Intensive Home-Based Applied Behavior Analysis". The Behavior Analyst Today. 7 (1): 96–100. doi:10.1037/h0100140.
- ↑ Reichow B, Wolery M (January 2009). "Comprehensive synthesis of early intensive behavioral interventions for young children with autism based on the UCLA young autism project model". Journal of Autism and Developmental Disorders. 39 (1): 23–41. doi:10.1007/s10803-008-0596-0. PMID 18535894. S2CID 6932830.
- ↑ Eldevik S, Hastings RP, Hughes JC, Jahr E, Eikeseth S, Cross S (May 2009). "Meta-analysis of Early Intensive Behavioral Intervention for children with autism". Journal of Clinical Child and Adolescent Psychology. 38 (3): 439–50. doi:10.1080/15374410902851739. PMID 19437303. S2CID 205873629.
- ↑ Spreckley M, Boyd R (March 2009). "Efficacy of applied behavioral intervention in preschool children with autism for improving cognitive, language, and adaptive behavior: a systematic review and meta-analysis". The Journal of Pediatrics. 154 (3): 338–44. doi:10.1016/j.jpeds.2008.09.012. PMID 18950798.
- ↑ Jacobson JW (2000). "Converting to a Behavior Analysis Format for Autism Services: Decision-Making for Educational Administrators, Principals, and Consultants". The Behavior Analyst Today. 1 (3): 6–16. doi:10.1037/h0099889.
- ↑ Pivotal response therapy:
- Koegel RL, Koegel LK (2006). Pivotal Response Treatments for Autism: Communication, Social, & Academic Development. Brookes. ISBN 1-55766-819-1.
- Koegel LK, Koegel RL, Harrower JK, Carter CM (1999). "Pivotal response intervention I: overview of approach". Journal of the Association for Persons with Severe Handicaps. 24 (3): 174–85. doi:10.2511/rpsd.24.3.174. S2CID 143633277.
- 1 2 Gillis JM, Butler RC (2007). "Social skills interventions for preschoolers with Autism Spectrum Disorder: A description of single – subject design studies". Journal of Early and Intensive Behavior Intervention. 4 (3): 532–548. doi:10.1037/h0100390.
- 1 2 Scottish Intercollegiate Guidelines Network (SIGN) (2007). "Assessment, diagnosis and clinical interventions for children and young people with autism spectrum disorders" (PDF). SIGN publication no. 98. Archived (PDF) from the original on 7 April 2008. Retrieved 2008-04-02. Lay summary (PDF) – SIGN (2008).
{{cite journal}}: Cite journal requires|journal=(help); Cite uses deprecated parameter|lay-date=(help) - ↑ Schlosser RW, Wendt O (August 2008). "Effects of augmentative and alternative communication intervention on speech production in children with autism: a systematic review". American Journal of Speech-Language Pathology. 17 (3): 212–30. doi:10.1044/1058-0360(2008/021). PMID 18663107.
- ↑ Kasari C, Freeman S, Paparella T (June 2006). "Joint attention and symbolic play in young children with autism: a randomized controlled intervention study". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 47 (6): 611–20. doi:10.1111/j.1469-7610.2005.01567.x. PMID 16712638. "Erratum". Journal of Child Psychology and Psychiatry. 48 (5): 523. 2007. doi:10.1111/j.1469-7610.2007.01768.x.
no
- ↑ Gulsrud AC, Kasari C, Freeman S, Paparella T (November 2007). "Children with autism's response to novel stimuli while participating in interventions targeting joint attention or symbolic play skills". Autism. 11 (6): 535–46. doi:10.1177/1362361307083255. PMID 17947289. S2CID 24239762.
- ↑ Matson JL, Matson ML, Rivet TT (September 2007). "Social-skills treatments for children with autism spectrum disorders: an overview". Behavior Modification. 31 (5): 682–707. doi:10.1177/0145445507301650. PMID 17699124. S2CID 35318587.
- ↑ Bellini S, Peters JK, Benner L, Hopf A (2007). "A meta-analysis of school-based social skills interventions for children with autism spectrum disorders". Remedial and Special Education. 28 (3): 153–62. doi:10.1177/07419325070280030401. S2CID 145700489.
- 1 2 Rao PA, Beidel DC, Murray MJ (February 2008). "Social skills interventions for children with Asperger's syndrome or high-functioning autism: a review and recommendations". Journal of Autism and Developmental Disorders. 38 (2): 353–61. doi:10.1007/s10803-007-0402-4. PMID 17641962. S2CID 2507088.
- ↑ Prizant BM, Wetherby AM, Rubin E, Laurent AC, Rydell PJ (2005). The SCERTS manual : a comprehensive educational approach for young children with autism spectrum disorders. Baltimore, Md.: Paul H. Brookes. ISBN 978-1-55766-818-9.
- ↑ Gutstein SE, Burgess AF, Montfort K (September 2007). "Evaluation of the relationship development intervention program". Autism. 11 (5): 397–411. doi:10.1177/1362361307079603. PMID 17942454. S2CID 9207853.
- ↑ Kaufman BN (1995). Son-Rise: the Miracle Continues. HJ Kramer. ISBN 0-915811-61-8.
- ↑ "Training Parents to Promote Communication and Social Behavior in Children with Autism: The Son-Rise Program" (PDF). www.autismtreatmentcenter.org. Retrieved 2022-01-05.
- ↑ Trevisan DA, Roberts N, Lin C, Birmingham E (2017-11-28). "How do adults and teens with self-declared Autism Spectrum Disorder experience eye contact? A qualitative analysis of first-hand accounts". PLOS ONE. 12 (11): e0188446. Bibcode:2017PLoSO..1288446T. doi:10.1371/journal.pone.0188446. PMC 5705114. PMID 29182643.
- ↑ Williams KR, Wishart JG (2003). "The Son-Rise Program intervention for autism: an investigation into family experiences". Journal of Intellectual Disability Research. 47 (Pt 4-5): 291–9. doi:10.1046/j.1365-2788.2003.00491.x. PMID 12787161.
- ↑ Williams KR (January 2006). "The Son-Rise Program intervention for autism: prerequisites for evaluation". Autism. 10 (1): 86–102. doi:10.1177/1362361306062012. PMID 16522712. S2CID 22206988.
- ↑ Ozonoff S, Cathcart K (February 1998). "Effectiveness of a home program intervention for young children with autism". Journal of Autism and Developmental Disorders. 28 (1): 25–32. doi:10.1023/A:1026006818310. PMID 9546299. S2CID 23324899.
- ↑ Virues-Ortega J, Julio FM, Pastor-Barriuso R (December 2013). "The TEACCH program for children and adults with autism: a meta-analysis of intervention studies". Clinical Psychology Review. 33 (8): 940–53. doi:10.1016/j.cpr.2013.07.005. PMID 23988454.
- ↑ Rogers SJ, Ozonoff S (December 2005). "Annotation: what do we know about sensory dysfunction in autism? A critical review of the empirical evidence". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 46 (12): 1255–68. doi:10.1111/j.1469-7610.2005.01431.x. PMID 16313426.
- ↑ "Sensory integrative therapy". Research Autism. Retrieved 2007-10-08.
- 1 2 3 Baranek GT (October 2002). "Efficacy of sensory and motor interventions for children with autism". Journal of Autism and Developmental Disorders. 32 (5): 397–422. doi:10.1023/A:1020541906063. PMID 12463517. S2CID 16449130.
- ↑ Stephenson J, Carter M (January 2009). "The use of weighted vests with children with autism spectrum disorders and other disabilities". Journal of Autism and Developmental Disorders. 39 (1): 105–14. doi:10.1007/s10803-008-0605-3. PMID 18592366. S2CID 28121843.
- ↑ Schaaf RC, Miller LJ (2005). "Occupational therapy using a sensory integrative approach for children with developmental disabilities". Mental Retardation and Developmental Disabilities Research Reviews. 11 (2): 143–8. doi:10.1002/mrdd.20067. PMID 15977314.
- ↑ Sinha Y, Silove N, Hayen A, Williams K (December 2011). "Auditory integration training and other sound therapies for autism spectrum disorders (ASD)". The Cochrane Database of Systematic Reviews (12): CD003681. doi:10.1002/14651858.CD003681.pub3. PMC 7173755. PMID 22161380.
- ↑ Hodgetts S, Hodgetts W (December 2007). "Somatosensory stimulation interventions for children with autism: literature review and clinical considerations". Canadian Journal of Occupational Therapy. 74 (5): 393–400. doi:10.2182/cjot.07.013. PMID 18183774. S2CID 25016676.
- ↑ Nimer J, Lundahl B (2007). "Animal-assisted therapy: a meta-analysis". Anthrozoös. 20 (3): 225–38. doi:10.2752/089279307X224773. S2CID 53310654.
- ↑ Marino L, Lilienfeld SO (2007). "Dolphin-Assisted Therapy: more flawed data and more flawed conclusions" (PDF). Anthrozoös. 20 (3): 239–49. doi:10.2752/089279307X224782. S2CID 6119940. Archived from the original (PDF) on 2008-02-28. Retrieved 2008-02-20.
- ↑ Ávila-Álvarez A, Alonso-Bidegain M, De-Rosende-Celeiro I, Vizcaíno-Cela M, Larrañeta-Alcalde L, Torres-Tobío G (July 2020). "Improving social participation of children with autism spectrum disorder: Pilot testing of an early animal-assisted intervention in Spain". Health & Social Care in the Community. 28 (4): 1220–1229. doi:10.1111/hsc.12955. hdl:2183/28097. PMID 32022346. S2CID 211035217.
- ↑ Wijker C, Leontjevas R, Spek A, Enders-Slegers MJ (December 2019). "Process Evaluation of Animal-Assisted Therapy: Feasibility and Relevance of a Dog-Assisted Therapy Program in Adults with Autism Spectrum Disorder". Animals. 9 (12): 1103. doi:10.3390/ani9121103. PMC 6940976. PMID 31835401.
- 1 2 3 4 Wijker C, Kupper N, Leontjevas R, Spek A, Enders-Slegers MJ (2021-09-01). "The effects of Animal Assisted Therapy on autonomic and endocrine activity in adults with autism spectrum disorder: A randomized controlled trial". General Hospital Psychiatry. 72: 36–44. doi:10.1016/j.genhosppsych.2021.05.003. PMID 34237553. S2CID 235778636.
- ↑ Wijker C, Leontjevas R, Spek A, Enders-Slegers MJ (June 2020). "Effects of Dog Assisted Therapy for Adults with Autism Spectrum Disorder: An Exploratory Randomized Controlled Trial". Journal of Autism and Developmental Disorders. 50 (6): 2153–2163. doi:10.1007/s10803-019-03971-9. PMC 7261269. PMID 30900194.
- ↑ Coben R, Linden M, Myers TE (March 2010). "Neurofeedback for autistic spectrum disorder: a review of the literature". Applied Psychophysiology and Biofeedback. 35 (1): 83–105. doi:10.1007/s10484-009-9117-y. PMID 19856096. S2CID 8425504.
- ↑ Mercado J, Espinosa-Curiel I, Escobedo L, Tentori M (2019-05-01). "Developing and evaluating a BCI video game for neurofeedback training: the case of autism". Multimedia Tools and Applications. 78 (10): 13675–13712. doi:10.1007/s11042-018-6916-2. ISSN 1573-7721. S2CID 54074403.
- ↑ Ziring PR, brazdziunas D, Cooley WC, Kastner TA, Kummer ME, González de Pijem L, et al. (November 1999). "American Academy of Pediatrics. Committee on Children with Disabilities. The treatment of neurologically impaired children using patterning". Pediatrics. 104 (5 Pt 1): 1149–51. doi:10.1542/peds.104.5.1149. PMID 10545565. S2CID 17770231.
- ↑ Harrower JK, Dunlap G (October 2001). "Including children with autism in general education classrooms. A review of effective strategies". Behavior Modification. 25 (5): 762–84. doi:10.1177/0145445501255006. PMID 11573339. S2CID 23887538.
- 1 2 "LEAP Program (Lifeskills and Education for Students with Autism and Other Pervasive Behavioral Challenges)." Kennedy Krieger Institute: Unlocking Potential. 2012. Accessed November 1, 2015.
- ↑ Boyd BA, Hume K, McBee MT, Alessandri M, Gutierrez A, Johnson L, et al. (February 2014). "Comparative efficacy of LEAP, TEACCH and non-model-specific special education programs for preschoolers with autism spectrum disorders". Journal of Autism and Developmental Disorders. 44 (2): 366–80. doi:10.1007/s10803-013-1877-9. PMID 23812661. S2CID 26813806.
- ↑ Lee MS, Kim JI, Ernst E (March 2011). "Massage therapy for children with autism spectrum disorders: a systematic review". The Journal of Clinical Psychiatry. 72 (3): 406–11. doi:10.4088/JCP.09r05848whi. PMID 21208598.
- ↑ Geretsegger M, Elefant C, Mössler KA, Gold C (June 2014). "Music therapy for people with autism spectrum disorder". The Cochrane Database of Systematic Reviews (6): CD004381. doi:10.1002/14651858.CD004381.pub3. PMC 6956617. PMID 24936966.
- ↑ NurseJournal Staff (June 2021). "The Benefits of Music Therapy for Autistic Children". NurseJournal.org.
- ↑ James R, Sigafoos J, Green VA, Lancioni GE, O'Reilly MF, Lang R, et al. (2015). "Music therapy for individuals with autism spectrum disorder: A systematic review". Review Journal of Autism and Developmental Disorders. 2 (1): 39–54. doi:10.1007/s40489-014-0035-4. S2CID 145714890.
- 1 2 Geretsegger M, Holck U, Carpente JA, Elefant C, Kim J, Gold C (2015). "Common Characteristics of Improvisational Approaches in Music Therapy for Children with Autism Spectrum Disorder: Developing Treatment Guidelines". Journal of Music Therapy. 52 (2): 258–81. doi:10.1093/jmt/thv005. PMID 26019303.
- ↑ "Strategies and interventions". The National Autistic Society. United Kingdom.
- 1 2 Pfeiffer BA, Koenig K, Kinnealey M, Sheppard M, Henderson L (2011). "Effectiveness of sensory integration interventions in children with autism spectrum disorders: a pilot study". The American Journal of Occupational Therapy. 65 (1): 76–85. doi:10.5014/ajot.2011.09205. PMC 3708964. PMID 21309374.
- ↑ Benevides TW, Shore SM, Andresen ML, Caplan R, Cook B, Gassner DL, et al. (August 2020). "Interventions to address health outcomes among autistic adults: A systematic review". Autism. 24 (6): 1345–1359. doi:10.1177/1362361320913664. PMC 7787674. PMID 32390461.
- ↑ Oono, Inalegwu P; Honey, Emma J; McConachie, Helen (2013-04-30). "Parent-mediated early intervention for young children with autism spectrum disorders (ASD)". Cochrane Database of Systematic Reviews. Wiley (4): CD009774. doi:10.1002/14651858.cd009774.pub2. ISSN 1465-1858. PMID 23633377.
- ↑ McConachie H, Diggle T (February 2007). "Parent implemented early intervention for young children with autism spectrum disorder: a systematic review". Journal of Evaluation in Clinical Practice. 13 (1): 120–9. doi:10.1111/j.1365-2753.2006.00674.x. PMID 17286734.
- ↑ Oono IP, Honey EJ, McConachie H (April 2013). "Parent-mediated early intervention for young children with autism spectrum disorders (ASD)". The Cochrane Database of Systematic Reviews. 4 (4): CD009774. doi:10.1002/14651858.CD009774.pub2. PMID 23633377.
- 1 2 3 4 5 6 7 8 Levy SE, Hyman SL (2005). "Novel treatments for autistic spectrum disorders". Mental Retardation and Developmental Disabilities Research Reviews. 11 (2): 131–42. doi:10.1002/mrdd.20062. PMID 15977319.
- ↑ Schreibman L (2005). "Critical evaluation of issues in autism". The Science and Fiction of Autism. Harvard University Press. ISBN 0-674-01931-8.
- ↑ Sigafoos J, Green VA, Edrisinha C, Lancioni GE (2006). "Flashback to the 1960s: LSD in the treatment of autism". Developmental Neurorehabilitation. 10 (1): 75–81. doi:10.1080/13638490601106277. PMID 17608329. S2CID 23563951.
- ↑ Chavez B, Chavez-Brown M, Sopko MA, Rey JA (2007). "Atypical antipsychotics in children with pervasive developmental disorders". Paediatric Drugs. 9 (4): 249–66. doi:10.2165/00148581-200709040-00006. PMID 17705564. S2CID 6690106.
- ↑ Scott LJ, Dhillon S (2007). "Risperidone: a review of its use in the treatment of irritability associated with autistic disorder in children and adolescents". Paediatric Drugs. 9 (5): 343–54. doi:10.2165/00148581-200709050-00006. PMID 17927305.
- ↑ Scahill L (July 2008). "How do I decide whether or not to use medication for my child with autism? Should I try behavior therapy first?". Journal of Autism and Developmental Disorders. 38 (6): 1197–8. doi:10.1007/s10803-008-0573-7. PMID 18463973. S2CID 20767044.
- ↑ Hirsch LE, Pringsheim T (June 2016). "Aripiprazole for autism spectrum disorders (ASD)". The Cochrane Database of Systematic Reviews (6): CD009043. doi:10.1002/14651858.CD009043.pub3. PMC 7120220. PMID 27344135.
- ↑ Myers SM (August 2007). "The status of pharmacotherapy for autism spectrum disorders". Expert Opinion on Pharmacotherapy. 8 (11): 1579–603. doi:10.1517/14656566.8.11.1579. PMID 17685878. S2CID 24674542.
- ↑ Volkmar FR (June 2009). "Citalopram treatment in children with autism spectrum disorders and high levels of repetitive behavior". Archives of General Psychiatry. 66 (6): 581–2. doi:10.1001/archgenpsychiatry.2009.42. PMID 19487622.
- ↑ King BH, Hollander E, Sikich L, McCracken JT, Scahill L, Bregman JD, et al. (June 2009). "Lack of efficacy of citalopram in children with autism spectrum disorders and high levels of repetitive behavior: citalopram ineffective in children with autism". Archives of General Psychiatry. 66 (6): 583–90. doi:10.1001/archgenpsychiatry.2009.30. PMC 4112556. PMID 19487623. Lay summary – Los Angeles Times (2009-06-02).
{{cite journal}}: Cite uses deprecated parameter|lay-source=(help) - ↑ Williams K, Brignell A, Randall M, Silove N, Hazell P (August 2013). "Selective serotonin reuptake inhibitors (SSRIs) for autism spectrum disorders (ASD)". The Cochrane Database of Systematic Reviews. 8 (8): CD004677. doi:10.1002/14651858.CD004677.pub3. PMID 23959778.
- 1 2 Sturman N, Deckx L, van Driel ML, et al. (Cochrane Developmental, Psychosocial and Learning Problems Group) (November 2017). "Methylphenidate for children and adolescents with autism spectrum disorder". The Cochrane Database of Systematic Reviews. 2017 (11): CD011144. doi:10.1002/14651858.CD011144.pub2. PMC 6486133. PMID 29159857.
- ↑ Parikh MS, Kolevzon A, Hollander E (April 2008). "Psychopharmacology of aggression in children and adolescents with autism: a critical review of efficacy and tolerability". Journal of Child and Adolescent Psychopharmacology. 18 (2): 157–78. doi:10.1089/cap.2007.0041. PMID 18439113.
- ↑ Francis K (July 2005). "Autism interventions: a critical update". Developmental Medicine and Child Neurology. 47 (7): 493–9. doi:10.1017/S0012162205000952. PMID 15991872.
- 1 2 Opar A (April 2008). "Search for potential autism treatments turns to 'trust hormone'". Nature Medicine. 14 (4): 353. doi:10.1038/nm0408-353. PMID 18391923. S2CID 200768.
- ↑ Bartz JA, Hollander E (2008). "Oxytocin and experimental therapeutics in autism spectrum disorders". Advances in Vasopressin and Oxytocin — from Genes to Behaviour to Disease. Progress in Brain Research. Vol. 170. pp. 451–62. doi:10.1016/S0079-6123(08)00435-4. ISBN 978-0-444-53201-5. PMID 18655901.
- ↑ Holmes, Bob (11 February 2022). "Oxytocin's effects aren't just about love". Knowable Magazine. doi:10.1146/knowable-021122-1. Retrieved 15 February 2022.
- ↑ Froemke, Robert C.; Young, Larry J. (8 July 2021). "Oxytocin, Neural Plasticity, and Social Behavior". Annual Review of Neuroscience. 44 (1): 359–381. doi:10.1146/annurev-neuro-102320-102847. ISSN 0147-006X. Retrieved 15 February 2022.
- ↑ Chez MG, Burton Q, Dowling T, Chang M, Khanna P, Kramer C (May 2007). "Memantine as adjunctive therapy in children diagnosed with autistic spectrum disorders: an observation of initial clinical response and maintenance tolerability". Journal of Child Neurology. 22 (5): 574–9. doi:10.1177/0883073807302611. PMID 17690064. S2CID 41428656.
- ↑ Erickson CA, Posey DJ, Stigler KA, Mullett J, Katschke AR, McDougle CJ (March 2007). "A retrospective study of memantine in children and adolescents with pervasive developmental disorders". Psychopharmacology. 191 (1): 141–7. doi:10.1007/s00213-006-0518-9. PMID 17016714. S2CID 13128356.
- ↑ Joshi G (26 February 2016). "A Study of Memantine Hydrochloride (Namenda®) for Cognitive and Behavioral Impairment in Adults With Autism Spectrum Disorders".
- ↑ Strock M (2007). "Autism spectrum disorders (pervasive developmental disorders)". National Institute of Mental Health. Archived from the original on 2007-10-04. Retrieved 2007-10-05.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Serruya MD, Kahana MJ (October 2008). "Techniques and devices to restore cognition". Behavioural Brain Research. 192 (2): 149–65. doi:10.1016/j.bbr.2008.04.007. PMC 3051349. PMID 18539345.
- ↑ Bishop J (2003). "The Internet for educating individuals with social impairments". Journal of Computer Assisted Learning. 19 (4): 546–56. doi:10.1046/j.0266-4909.2003.00057.x.
- ↑ el Kaliouby R, Picard R, Baron-Cohen S (December 2006). "Affective computing and autism". Annals of the New York Academy of Sciences. 1093 (1): 228–48. Bibcode:2006NYASA1093..228K. doi:10.1196/annals.1382.016. PMID 17312261. S2CID 405379.
- ↑ Novella S (1 July 2013). "Transcranial Magnetic Stimulation for Autism". Neurologica Blog. Retrieved 15 December 2013.
- ↑ Oberman LM, Rotenberg A, Pascual-Leone A (February 2015). "Use of transcranial magnetic stimulation in autism spectrum disorders". Journal of Autism and Developmental Disorders. 45 (2): 524–36. doi:10.1007/s10803-013-1960-2. PMC 4519010. PMID 24127165.
- ↑ Oberman LM, Enticott PG, Casanova MF, Rotenberg A, Pascual-Leone A, McCracken JT (February 2016). "Transcranial magnetic stimulation in autism spectrum disorder: Challenges, promise, and roadmap for future research". Autism Research. 9 (2): 184–203. doi:10.1002/aur.1567. PMC 4956084. PMID 26536383.
- 1 2 Levy SE, Hyman SL (October 2008). "Complementary and alternative medicine treatments for children with autism spectrum disorders". Child and Adolescent Psychiatric Clinics of North America. 17 (4): 803–20, ix. doi:10.1016/j.chc.2008.06.004. PMC 2597185. PMID 18775371.
- 1 2 3 4 5 6 7 8 Angley M, Semple S, Hewton C, Paterson F, McKinnon R (October 2007). "Children and autism--Part 2--management with complementary medicines and dietary interventions" (PDF). Australian Family Physician. 36 (10): 827–30. PMID 17925903. Archived from the original (PDF) on 2007-12-01.
- ↑ Schechtman MA (August 2007). "Scientifically unsupported therapies in the treatment of young children with autism spectrum disorders". Pediatric Annals. 36 (8): 497–8, 500–2, 504–5. doi:10.3928/0090-4481-20070801-12. PMID 17849608.
- ↑ Lack of support for interventions:
- Howlin P (2005). "The effectiveness of interventions for children with autism". In Fleischhacker WW, Brooks DJ (eds.). Neurodevelopmental Disorders. Journal of Neural Transmission. Supplementum. Springer. pp. 101–19. doi:10.1007/3-211-31222-6_6. ISBN 3-211-26291-1. PMID 16355605.
- Sigman M, Spence SJ, Wang AT (2006). "Autism from developmental and neuropsychological perspectives". Annual Review of Clinical Psychology. 2: 327–55. doi:10.1146/annurev.clinpsy.2.022305.095210. PMID 17716073.
- Williams White S, Keonig K, Scahill L (November 2007). "Social skills development in children with autism spectrum disorders: a review of the intervention research". Journal of Autism and Developmental Disorders. 37 (10): 1858–68. doi:10.1007/s10803-006-0320-x. PMID 17195104. S2CID 14573426.
- ↑ Burgess AF, Gutstein SE (May 2007). "Quality of Life for People with Autism: Raising the Standard for Evaluating Successful Outcomes". Child and Adolescent Mental Health. 12 (2): 80–86. doi:10.1111/j.1475-3588.2006.00432.x. PMID 32811109.
- ↑ Stahmer AC, Collings NM, Palinkas LA (2005). "Early Intervention Practices for Children With Autism: Descriptions From Community Providers". Focus on Autism and Other Developmental Disabilities. 20 (2): 66–79. doi:10.1177/10883576050200020301. PMC 1350798. PMID 16467905.
- 1 2 Christison GW, Ivany K (April 2006). "Elimination diets in autism spectrum disorders: any wheat amidst the chaff?". Journal of Developmental and Behavioral Pediatrics. 27 (2 Suppl): S162-71. doi:10.1097/00004703-200604002-00015. PMID 16685183.
- 1 2 "I Wanted to "Cure My Autism," Too– One Autistic Woman's Story of Internalized Ableism". NeuroClastic. 2019-06-10. Retrieved 2022-01-05.
- ↑ Lee MS, Choi TY, Shin BC, Ernst E (August 2012). "Acupuncture for children with autism spectrum disorders: a systematic review of randomized clinical trials". Journal of Autism and Developmental Disorders. 42 (8): 1671–1683. doi:10.1007/s10803-011-1409-4. PMID 22124580. S2CID 30628519.
- ↑ Cheuk DK, Wong V, Chen WX (September 2011). Cheuk DK (ed.). "Acupuncture for autism spectrum disorders (ASD)". The Cochrane Database of Systematic Reviews. 9 (9): CD007849. doi:10.1002/14651858.CD007849.pub2. PMID 21901712.
- ↑ Rossignol DA, Rossignol LW, James SJ, Melnyk S, Mumper E (2007). "The Effects of Hyperbaric Oxygen Therapy on Oxidative Stress, Inflammation, and Symptoms in Children with Autism: An Open-label Pilot Study". BMC Pediatrics. 7 (36): 1–13. doi:10.1186/1471-2431-7-36. PMC 2244616. PMID 18005455.
- ↑ Rossignol DA, Rossignol LW, Smith S, Schneider C, Logerquist S, Usman A, et al. (March 2009). "Hyperbaric treatment for children with autism: a multicenter, randomized, double-blind, controlled trial". BMC Pediatrics. 9: 21. doi:10.1186/1471-2431-9-21. PMC 2662857. PMID 19284641. Lay summary – BBC News (2009-03-14).
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - ↑ Granpeesheh D, Tarbox J, Dixon DR, Wilke AE, Allen MS, Bradstreet J (2010). "Randomized trial of hyperbaric oxygen therapy for children with autism". Research in Autism Spectrum Disorders. 4 (2): 268–275. doi:10.1016/j.rasd.2009.09.014.
- 1 2 Jepson B, Granpeesheh D, Tarbox J, Olive ML, Stott C, Braud S, et al. (May 2011). "Controlled evaluation of the effects of hyperbaric oxygen therapy on the behavior of 16 children with autism spectrum disorders". Journal of Autism and Developmental Disorders. 41 (5): 575–88. doi:10.1007/s10803-010-1075-y. PMID 20680427. S2CID 653316.
- ↑ Sakulchit T, Ladish C, Goldman RD (June 2017). "Hyperbaric oxygen therapy for children with autism spectrum disorder". Canadian Family Physician. 63 (6): 446–448. PMC 5471082. PMID 28615394.
- 1 2 Campbell JB, Busse JW, Injeyan HS (April 2000). "Chiropractors and vaccination: A historical perspective". Pediatrics. 105 (4): E43. doi:10.1542/peds.105.4.e43. PMID 10742364. S2CID 14561867.
- 1 2 Busse JW, Morgan L, Campbell JB (June 2005). "Chiropractic antivaccination arguments". Journal of Manipulative and Physiological Therapeutics. 28 (5): 367–73. doi:10.1016/j.jmpt.2005.04.011. PMID 15965414.
- ↑ Madsen KM, Hviid A, Vestergaard M, Schendel D, Wohlfahrt J, Thorsen P, et al. (November 2002). "A population-based study of measles, mumps, and rubella vaccination and autism". The New England Journal of Medicine. 347 (19): 1477–82. doi:10.1056/NEJMoa021134. PMC 2504909. PMID 12421889.
- ↑ Ernst E (May 2008). "Chiropractic: a critical evaluation". Journal of Pain and Symptom Management. 35 (5): 544–62. doi:10.1016/j.jpainsymman.2007.07.004. PMID 18280103.
- ↑ Hawk C, Khorsan R, Lisi AJ, Ferrance RJ, Evans MW (June 2007). "Chiropractic care for nonmusculoskeletal conditions: a systematic review with implications for whole systems research". Journal of Alternative and Complementary Medicine. 13 (5): 491–512. doi:10.1089/acm.2007.7088. PMID 17604553.
- 1 2 Green C, Martin CW, Bassett K, Kazanjian A (December 1999). "A systematic review of craniosacral therapy: biological plausibility, assessment reliability and clinical effectiveness". Complementary Therapies in Medicine. 7 (4): 201–7. doi:10.1016/S0965-2299(99)80002-8. PMID 10709302. An earlier version of the paper is available without a subscription: Green C, Martin CW, Bassett K, Kazanjian A (1999). "A systematic review and critical appraisal of the scientific evidence on craniosacral therapy" (PDF). BCOHTA 99:1J. British Columbia Office of Health Technology Assessment. Archived from the original (PDF) on 2008-02-29. Retrieved 2007-10-08.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Hartman SE, Norton JM (2002). "Interexaminer reliability and cranial osteopathy" (PDF). 6 (1): 23–34. Retrieved 2007-10-08.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Lonsdale D, Shamberger RJ, Audhya T (August 2002). "Treatment of autism spectrum children with thiamine tetrahydrofurfuryl disulfide: a pilot study" (PDF). Neuro Endocrinology Letters. 23 (4): 303–8. PMID 12195231. Archived from the original (PDF) on 2008-02-29.
- ↑ Lonsdale D (March 2006). "A review of the biochemistry, metabolism and clinical benefits of thiamin(e) and its derivatives". Evidence-Based Complementary and Alternative Medicine. 3 (1): 49–59. doi:10.1093/ecam/nek009. PMC 1375232. PMID 16550223. Archived from the original on 2007-10-25.
- ↑ Hazards of chelation therapy:
- Brown MJ, Willis T, Omalu B, Leiker R (August 2006). "Deaths resulting from hypocalcemia after administration of edetate disodium: 2003-2005". Pediatrics. 118 (2): e534-6. doi:10.1542/peds.2006-0858. PMID 16882789. S2CID 28656831.
- Baxter AJ, Krenzelok EP (December 2008). "Pediatric fatality secondary to EDTA chelation". Clinical Toxicology. 46 (10): 1083–4. doi:10.1080/15563650701261488. PMID 18949650. S2CID 24576683.
- ↑ Doja A, Roberts W (November 2006). "Immunizations and autism: a review of the literature". The Canadian Journal of Neurological Sciences. 33 (4): 341–6. doi:10.1017/s031716710000528x. PMID 17168158. S2CID 4670282.
- ↑ Thompson WW, Price C, Goodson B, Shay DK, Benson P, Hinrichsen VL, et al. (September 2007). "Early thimerosal exposure and neuropsychological outcomes at 7 to 10 years". The New England Journal of Medicine. 357 (13): 1281–92. doi:10.1056/NEJMoa071434. PMID 17898097.
- ↑ Weber W, Newmark S (December 2007). "Complementary and alternative medical therapies for attention-deficit/hyperactivity disorder and autism". Pediatric Clinics of North America. 54 (6): 983–1006, xii. doi:10.1016/j.pcl.2007.09.006. PMID 18061787.
- ↑ Davis TN, O'Reilly M, Kang S, Lang R, Rispoli M, Sigafoos J, et al. (2013). "Chelation treatment for autism spectrum disorders: A systematic review". Research in Autism Spectrum Disorders. 7 (1): 49–55. doi:10.1016/j.rasd.2012.06.005.
The research reviewed here does not support the use of chelation as a treatment for ASD
- ↑ Reichelt KL, Knivsberg AM, Lind G, Nødland M (1991). "Probable etiology and possible treatment of childhood autism". 4: 308–19.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Millward C, Ferriter M, Calver S, Connell-Jones G (April 2008). "Gluten- and casein-free diets for autistic spectrum disorder". The Cochrane Database of Systematic Reviews (2): CD003498. doi:10.1002/14651858.CD003498.pub3. PMC 4164915. PMID 18425890. (Retracted, see doi:10.1002/14651858.cd003498.pub4)
- ↑ Dolske MC, Spollen J, McKay S, Lancashire E, Tolbert L (September 1993). "A preliminary trial of ascorbic acid as supplemental therapy for autism". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 17 (5): 765–74. doi:10.1016/0278-5846(93)90058-Z. PMID 8255984. S2CID 29370921.
- ↑ Erickson CA, Stigler KA, Corkins MR, Posey DJ, Fitzgerald JF, McDougle CJ (December 2005). "Gastrointestinal factors in autistic disorder: a critical review". Journal of Autism and Developmental Disorders. 35 (6): 713–27. doi:10.1007/s10803-005-0019-4. PMID 16267642. S2CID 26829936.
- ↑ Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H, Folstein S (2007). "Atypical behaviors in children with autism and children with a history of language impairment". Research in Developmental Disabilities. 28 (2): 145–62. doi:10.1016/j.ridd.2006.02.003. PMID 16581226.
- ↑ Wong HH, Smith RG (October 2006). "Patterns of complementary and alternative medical therapy use in children diagnosed with autism spectrum disorders". Journal of Autism and Developmental Disorders. 36 (7): 901–9. doi:10.1007/s10803-006-0131-0. PMID 16897395. S2CID 30307579.
- ↑ Hediger ML, England LJ, Molloy CA, Yu KF, Manning-Courtney P, Mills JL (May 2008). "Reduced bone cortical thickness in boys with autism or autism spectrum disorder". Journal of Autism and Developmental Disorders. 38 (5): 848–56. doi:10.1007/s10803-007-0453-6. PMID 17879151. S2CID 31255839. Lay summary – NIH News (2008-01-29).
{{cite journal}}: Cite uses deprecated parameter|lay-url=(help) - ↑ Rossignol DA (2009). "Novel and emerging treatments for autism spectrum disorders: a systematic review" (PDF). Annals of Clinical Psychiatry. 21 (4): 213–36. PMID 19917212. Archived from the original (PDF) on 2015-07-15.
- ↑ Nye C, Brice A (October 2005). Nye C (ed.). "Combined vitamin B6-magnesium treatment in autism spectrum disorder". The Cochrane Database of Systematic Reviews (4): CD003497. doi:10.1002/14651858.CD003497.pub2. PMC 7003675. PMID 16235322.
- ↑ Malow BA, Byars K, Johnson K, Weiss S, Bernal P, Goldman SE, et al. (November 2012). "A practice pathway for the identification, evaluation, and management of insomnia in children and adolescents with autism spectrum disorders". Pediatrics. 130 (Supplement 2): S106-24. doi:10.1542/peds.2012-0900I. PMID 23118242. S2CID 15066964.
- ↑ Rossignol DA, Frye RE (2013). "Melatonin in autism spectrum disorders". Current Clinical Pharmacology. 9 (4): 326–34. doi:10.2174/15748847113086660072. PMID 24050742.
- ↑ Bent S, Bertoglio K, Hendren RL (August 2009). "Omega-3 fatty acids for autistic spectrum disorder: a systematic review". Journal of Autism and Developmental Disorders. 39 (8): 1145–54. doi:10.1007/s10803-009-0724-5. PMC 2710498. PMID 19333748.
- ↑ James S, Montgomery P, Williams K (November 2011). James S (ed.). "Omega-3 fatty acids supplementation for autism spectrum disorders (ASD)". The Cochrane Database of Systematic Reviews (11): CD007992. doi:10.1002/14651858.CD007992.pub2. PMID 22071839.
- ↑ Tsouderos T (2010-01-17). "OSR#1: industrial chemical or autism treatment?". Chicago Tribune. Archived from the original on 2010-02-21. Retrieved 2010-02-11.
- ↑ Aneja A, Tierney E (April 2008). "Autism: the role of cholesterol in treatment". International Review of Psychiatry. 20 (2): 165–70. doi:10.1080/09540260801889062. PMID 18386207. S2CID 13175585.
- ↑ Wasilewska J, Klukowski M (2015-09-28). "Gastrointestinal symptoms and autism spectrum disorder: links and risks - a possible new overlap syndrome". Pediatric Health, Medicine and Therapeutics. 6: 153–166. doi:10.2147/PHMT.S85717. PMC 5683266. PMID 29388597.
- ↑ Gorrindo P, Williams KC, Lee EB, Walker LS, McGrew SG, Levitt P (April 2012). "Gastrointestinal dysfunction in autism: parental report, clinical evaluation, and associated factors". Autism Research. 5 (2): 101–108. doi:10.1002/aur.237. PMC 3335766. PMID 22511450.
- ↑ Abdelrahman HM, Sherief LM, Alghobashy AA, Abdel Salam SM, Hashim HM, Abdel Fattah NR, Mohamed RH (January 2015). "Association of 5-HT2A receptor gene polymorphisms with gastrointestinal disorders in Egyptian children with autistic disorder". Research in Developmental Disabilities. 36C: 485–490. doi:10.1016/j.ridd.2014.10.023. PMID 25462508.
- ↑ "Autism spectrum disorder and digestive symptoms". Mayo Clinic. Retrieved 2022-01-05.
- ↑ Popow C, Ohmann S, Plener P (September 2021). "Practitioner's review: medication for children and adolescents with autism spectrum disorder (ASD) and comorbid conditions". Neuropsychiatrie. 35 (3): 113–134. doi:10.1007/s40211-021-00395-9. PMC 8429404. PMID 34160787.
- ↑ Dhossche DM, Reti IM, Wachtel LE (March 2009). "Catatonia and autism: a historical review, with implications for electroconvulsive therapy". The Journal of ECT. 25 (1): 19–22. doi:10.1097/YCT.0b013e3181957363. PMID 19190507.
- ↑ Ichim TE, Solano F, Glenn E, Morales F, Smith L, Zabrecky G, Riordan NH (June 2007). "Stem cell therapy for autism". Journal of Translational Medicine. 5 (30): 30. doi:10.1186/1479-5876-5-30. PMC 1914111. PMID 17597540.
- ↑ Siniscalco D, Sapone A, Cirillo A, Giordano C, Maione S, Antonucci N (2012). "Autism spectrum disorders: is mesenchymal stem cell personalized therapy the future?". Journal of Biomedicine & Biotechnology. 2012: 480289. doi:10.1155/2012/480289. PMC 3151496. PMID 22496609.
- 1 2 Siniscalco D, Sapone A, Cirillo A, Giordano C, Maione S, Antonucci N (1 January 2012). "Autism spectrum disorders: is mesenchymal stem cell personalized therapy the future?". Journal of Biomedicine & Biotechnology. 2012: 480289. doi:10.1155/2012/480289. PMC 3151496. PMID 22496609.
- ↑ Spinney L (August 2007). "Therapy for autistic children causes outcry in France". Lancet. 370 (9588): 645–6. doi:10.1016/S0140-6736(07)61322-1. PMID 17726792. S2CID 30354968.
- ↑ Chamak B (2019-06-01). "Lobbying by association: The case of autism and the controversy over packing therapy in France". Social Science & Medicine. 230: 256–263. doi:10.1016/j.socscimed.2019.04.027. ISSN 0277-9536. PMID 31035204. S2CID 140304275.
- ↑ Wing L (1997). "The history of ideas on autism: legends, myths and reality". 1 (1): 13–23. doi:10.1177/1362361397011004. S2CID 145210370.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Miles M (2005). "Martin Luther and childhood disability in 16th century Germany: what did he write? what did he say?". Independent Living Institute. Retrieved 2008-12-23.
- ↑ Collins D (2003-08-25). "Autistic boy dies during exorcism". CBS News.
- ↑ "Exorcisms often claim the most innocent -- our children". NBC News. Retrieved 2022-01-05.
- ↑ Shaked M, Bilu Y (March 2006). "Grappling with affliction: autism in the Jewish ultraorthodox community in Israel". Culture, Medicine and Psychiatry. 30 (1): 1–27. doi:10.1007/s11013-006-9006-2. PMID 16783528. S2CID 25565277.
- ↑ Ekas NV, Whitman TL, Shivers C (May 2009). "Religiosity, spirituality, and socioemotional functioning in mothers of children with autism spectrum disorder". Journal of Autism and Developmental Disorders. 39 (5): 706–19. doi:10.1007/s10803-008-0673-4. PMID 19082877. S2CID 6735662.
- ↑ "Autism's early child". the Guardian. 2011-11-13. Retrieved 2022-01-05.
- ↑ Autism's early child, Guardian, retrieved 13/11/2011
- ↑ Harmon A (2004-12-20). "How About Not 'Curing' Us, Some Autistics Are Pleading". The New York Times. Archived from the original on December 2, 2011. Retrieved 2007-11-07.
- ↑ Saner E (2007-08-07). "It is not a disease, it is a way of life". The Guardian. Archived from the original on 20 August 2007. Retrieved 2007-08-07.
- 1 2 Ne'eman A (July 2021). "When Disability Is Defined by Behavior, Outcome Measures Should Not Promote "Passing"". AMA Journal of Ethics. 23 (7): E569–E575. doi:10.1001/amajethics.2021.569. PMID 34351268. S2CID 236926326.
- ↑ DeThorne LS, Searsmith K (2021-02-23). "Autism and Neurodiversity: Addressing Concerns and Offering Implications for the School-Based Speech-Language Pathologist". Perspectives of the ASHA Special Interest Groups. 6 (1): 184–190. doi:10.1044/2020_PERSP-20-00188. S2CID 233919959.
- ↑ Belcher HL, Morein-Zamir S, Mandy W, Ford RM (August 2021). "Camouflaging Intent, First Impressions, and Age of ASC Diagnosis in Autistic Men and Women". Journal of Autism and Developmental Disorders. doi:10.1007/s10803-021-05221-3. PMID 34342806. S2CID 236884857.
- ↑ Cook J, Crane L, Hull L, Bourne L, Mandy W (June 2021). "Self-reported camouflaging behaviours used by autistic adults during everyday social interactions". Autism: 13623613211026754. doi:10.1177/13623613211026754. PMID 34180249. S2CID 235661866.
- ↑ Hull L, Lai MC, Baron-Cohen S, Allison C, Smith P, Petrides KV, Mandy W (February 2020). "Gender differences in self-reported camouflaging in autistic and non-autistic adults". Autism. 24 (2): 352–363. doi:10.1177/1362361319864804. PMID 31319684. S2CID 197664299.
- ↑ Hull L, Mandy W, Lai MC, Baron-Cohen S, Allison C, Smith P, Petrides KV (March 2019). "Development and Validation of the Camouflaging Autistic Traits Questionnaire (CAT-Q)". Journal of Autism and Developmental Disorders. 49 (3): 819–833. doi:10.1007/s10803-018-3792-6. PMC 6394586. PMID 30361940.
- 1 2 Fombonne E (July 2020). "Camouflage and autism". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 61 (7): 735–738. doi:10.1111/jcpp.13296. PMID 32658354. S2CID 220500153.
- ↑ Cage E, Troxell-Whitman Z (2020-12-01). "Understanding the Relationships Between Autistic Identity, Disclosure, and Camouflaging". Autism in Adulthood. 2 (4): 334–338. doi:10.1089/aut.2020.0016. ISSN 2573-9581. S2CID 225399823.
- 1 2 Mandy W (November 2019). "Social camouflaging in autism: Is it time to lose the mask?". Autism. 23 (8): 1879–1881. doi:10.1177/1362361319878559. PMID 31552745. S2CID 202762080.
- ↑ Libsack EJ, Keenan EG, Freden CE, Mirmina J, Iskhakov N, Krishnathasan D, Lerner MD (December 2021). "A Systematic Review of Passing as Non-autistic in Autism Spectrum Disorder". Clinical Child and Family Psychology Review. 24 (4): 783–812. doi:10.1007/s10567-021-00365-1. PMID 34505231. S2CID 237472360.
- ↑ Benham JL, Kizer JS (2016-10-31). "Aut-ors of our Experience: Interrogating Intersections of Autistic Identity". Canadian Journal of Disability Studies. 5 (3): 77–113. doi:10.15353/cjds.v5i3.298. ISSN 1929-9192.
- ↑ Corscadden P, Casserly AM (2021-09-19). "Identification of Autism in Girls: Role of Trait Subtleties, Social Acceptance and Masking". REACH: Journal of Inclusive Education in Ireland. 34 (1). ISSN 0790-8695.
- ↑ Lawrence C (2019-04-18). Teacher Education and Autism: A Research-Based Practical Handbook. Jessica Kingsley Publishers. ISBN 978-1-78592-608-2.
- ↑ Pearson A, Rose K (2021-03-01). "A Conceptual Analysis of Autistic Masking: Understanding the Narrative of Stigma and the Illusion of Choice". Autism in Adulthood. 3 (1): 52–60. doi:10.1089/aut.2020.0043. ISSN 2573-9581. S2CID 234215884.
- ↑ Miller D, Rees J, Pearson A (2021-12-01). ""Masking Is Life": Experiences of Masking in Autistic and Nonautistic Adults". Autism in Adulthood. 3 (4): 330–338. doi:10.1089/aut.2020.0083. ISSN 2573-9581.
- ↑ Sedgewick F, Hull L, Ellis H (2021-12-21). Autism and Masking: How and Why People Do It, and the Impact It Can Have. Jessica Kingsley Publishers. ISBN 978-1-78775-580-2.
- ↑ Parsloe SM, Babrow AS (2016-04-02). "Removal of Asperger's syndrome from the DSM V: community response to uncertainty". Health Communication. 31 (4): 485–494. doi:10.1080/10410236.2014.968828. PMID 26400415. S2CID 23520937.
- ↑ DeThorne L, Searsmith K (2021-02-23). "Autism and Neurodiversity: Addressing Concerns and Offering Implications for the School-Based Speech-Language Pathologist". Perspectives of the ASHA Special Interest Groups. 6 (1): 184–190. doi:10.1044/2020_PERSP-20-00188. S2CID 233919959.
- ↑ Raymaker DM, Teo AR, Steckler NA, Lentz B, Scharer M, Delos Santos A, et al. (June 2020). ""Having All of Your Internal Resources Exhausted Beyond Measure and Being Left with No Clean-Up Crew": Defining Autistic Burnout". Autism in Adulthood. 2 (2): 132–143. doi:10.1089/aut.2019.0079. PMC 7313636. PMID 32851204.
- ↑ Ghanouni P, Quirke S, Blok J, Casey A (December 2021). "Independent living in adults with autism spectrum disorder: Stakeholders' perspectives and experiences". Research in Developmental Disabilities. 119: 104085. doi:10.1016/j.ridd.2021.104085. PMID 34600352. S2CID 238254134.
- ↑ Higgins JM, Arnold SR, Weise J, Pellicano E, Trollor JN (November 2021). "Defining autistic burnout through experts by lived experience: Grounded Delphi method investigating #AutisticBurnout". Autism. 25 (8): 2356–2369. doi:10.1177/13623613211019858. PMID 34088219. S2CID 235346830.
- ↑ Mantzalas J, Richdale AL, Adikari A, Lowe J, Dissanayake C (2021-09-20). "What Is Autistic Burnout? A Thematic Analysis of Posts on Two Online Platforms". Autism in Adulthood. doi:10.1089/aut.2021.0021. ISSN 2573-9581. S2CID 240600343.
- ↑ Phung J, Penner M, Pirlot C, Welch C (2021). "What I Wish You Knew: Insights on Burnout, Inertia, Meltdown, and Shutdown From Autistic Youth". Frontiers in Psychology. 12: 741421. doi:10.3389/fpsyg.2021.741421. PMC 8595127. PMID 34803822.
- ↑ McGuinness K (2021-05-31). "An evaluation of a tool, based on spoon theory, to promote self-regulation and avoidance of burnout in autistic children and young people". Good Autism Practice (GAP). 22 (1): 59–72.
- ↑ Tint A, Weiss JA (November 2018). "A qualitative study of the service experiences of women with autism spectrum disorder". Autism. 22 (8): 928–937. doi:10.1177/1362361317702561. PMID 28914071. S2CID 45067365.
- ↑ Cage E, Di Monaco J, Newell V (February 2018). "Experiences of Autism Acceptance and Mental Health in Autistic Adults". Journal of Autism and Developmental Disorders. 48 (2): 473–484. doi:10.1007/s10803-017-3342-7. PMC 5807490. PMID 29071566.
- ↑ Bradshaw P, Pickett C, van Driel ML, Brooker K, Urbanowicz A (March 2021). "Recognising, supporting and understanding Autistic adults in general practice settings". Australian Journal of General Practice. 50 (3): 126–130. doi:10.31128/AJGP-11-20-5722. PMID 33634275. S2CID 232057052.
- ↑ Howard PL, Sedgewick F (November 2021). "'Anything but the phone!': Communication mode preferences in the autism community". Autism. 25 (8): 2265–2278. doi:10.1177/13623613211014995. hdl:1983/9e9e3795-ff6d-4fbc-b794-27d0a808cc0e. PMID 34169750. S2CID 235635726.
- ↑ Grant A, Kara H (2021-12-08). "Considering the Autistic advantage in qualitative research: the strengths of Autistic researchers". Contemporary Social Science. 16 (5): 589–603. doi:10.1080/21582041.2021.1998589. ISSN 2158-2041. S2CID 243907591.
- ↑ Wilson C (2018-07-14). "The autistic advantage". New Scientist. 239 (3186): 32–33. Bibcode:2018NewSc.239...32W. doi:10.1016/S0262-4079(18)31254-5. ISSN 0262-4079. S2CID 125917495.
- ↑ Russell G, Kapp SK, Elliott D, Elphick C, Gwernan-Jones R, Owens C (June 2019). "Mapping the Autistic Advantage from the Accounts of Adults Diagnosed with Autism: A Qualitative Study". Autism in Adulthood. 1 (2): 124–133. doi:10.1089/aut.2018.0035. PMC 6493410. PMID 31058260.
Further reading
- Adams JB (2013). Summary of Dietary, Nutritional, and Medical Treatments for Autism – based on over 150 published research studies (PDF). ASU Autism/Asperger's Research Program (Report). Vol. 40. ARI publication. pp. 1–53. Archived from the original (PDF) on 2013-03-19.
- Fitzpatrick M (2008). Defeating Autism: A Damaging Delusion. London: Routledge. ISBN 978-0-415-44981-6. Reviewed in: Guldberg H (2008-12-19). "'Autistic children are now seen as a burden'". spiked.
- Foxx RM, Mulick JA (2016). Controversial therapies for autism and intellectual disabilities. Routledge.
- Monteiro MJ (2016). Family therapy and the autism spectrum. Routledge.
- Shaw W, Rimland B (2008). Biological treatments for autism and PDD (3rd ed.). Great Plains Laboratory Incorporated. ISBN 978-0-9661238-1-4.
- Ministries of Health and Education (2008). New Zealand Autism Spectrum Disorder Guideline (PDF). Wellington: Ministry of Health. ISBN 978-0-478-31257-7. Archived from the original (PDF) on 2008-10-16. Retrieved 2009-01-23. Archived 2008-10-16 at the Wayback Machine
- Bryson SE, Rogers SJ, Fombonne E (September 2003). "Autism spectrum disorders: early detection, intervention, education, and psychopharmacological management". Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie. 48 (8): 506–16. doi:10.1177/070674370304800802. PMID 14574826. S2CID 18876545.
- Erickson CA, Posey DJ, Stigler KA, McDougle CJ (September 2007). "Pharmacologic treatment of autism and related disorders". Pediatric Annals. 36 (9): 575–85. doi:10.3928/0090-4481-20070901-09. PMID 17910205.
- Keogh K (2014). "Autism therapy 'reduces core symptoms in children". Learning Disability Practice. 19 (10): 6. doi:10.7748/ldp.19.10.6.s2.
- Naviaux RK (November 2018). "Antipurinergic therapy for autism-An in-depth review". Mitochondrion. 43: 1–15. doi:10.1016/j.mito.2017.12.007. PMID 29253638.
- Posey DJ, McDougle CJ (October 2008). "Treating autism spectrum disorders. Preface". Child and Adolescent Psychiatric Clinics of North America. 17 (4): xv–xviii. doi:10.1016/j.chc.2008.07.001. PMID 18775365. This describes a special issue of the journal Child and Adolescent Psychiatric Clinics of North America, titled "Treating Autism Spectrum Disorders" (volume 17, issue 4, pages 713–932) and dated October 2008.