Cetrorelix
 | |
 | |
| Names | |
|---|---|
| Trade names | Cetrotide, others |
| Other names | Cetrorelix acetate |
IUPAC name
| |
| Clinical data | |
| Drug class | GnRH antagonist[1] |
| Main uses | Fertility treatment[2] |
| Side effects | Ovarian hyperstimulation syndrome, nausea, headache[1] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Routes of use | Subcutaneous injection |
| External links | |
| AHFS/Drugs.com | Monograph |
| Legal | |
| Legal status |
|
| Pharmacokinetics | |
| Bioavailability | 85% |
| Protein binding | 86% |
| Elimination half-life | 62.8 hours / 3 mg single dose; 5 hours / 0.25 mg single dose; 20.6 hours / 0.25 mg multiple doses |
| Excretion | feces (5% to 10% as unchanged drug and metabolites); urine (2% to 4% as unchanged drug) |
| Chemical and physical data | |
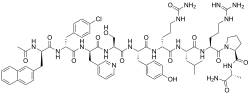
| Formula | C70H92ClN17O14 |
| Molar mass | 1431.06 g·mol−1 |
InChI
| |
Cetrorelix , sold under the brand name Cetrotide, is a medication used in fertility treatment to prevent early ovulation in women getting ovarian stimulation.[2] It is given by injection under the skin.[3]
Common side effects include ovarian hyperstimulation syndrome, nausea, and headache.[1] Other side effects may include anaphylaxis and liver problems.[1] Use during pregnancy may harm the baby.[1] It is a gonadotropin-releasing hormone (GnRH) blocker.[1]
Cetrorelix was approved for medical use in Europe in 1999 and the United States in 2000.[2][1] In the United Kingdom 250 micrograms costs the NHS about £27 as of 2021.[3] This amount in the United States costs about 250 USD.[4]
Medical uses
Cetrorelix is used in in-vitro fertilization.[5] In IVF use it is injected daily after follicle stimulation has been initiated and evidence of follicle maturation is approaching; given daily it prevents an endogenous LH surge that would trigger an untimely ovulation prior to the hCG administration. As an alternative to the GnRH antagonist, also a GnRH agonist could be given, but agonist have to be started earlier to overcome the agonistic effect. Cetrorelix can be mixed with follitropin alpha without compromising their reported safety and efficacy.[6]
Dosage
It is administered as either multiple 0.25 mg daily subcutaneous injections or as a single-dose 3 mg subcutaneous injection. The duration of the 3 mg single dose is four days; if human chorionic gonadotropin (hCG) is not administered within four days, a daily 0.25 mg dose is started and continued until hCG is administered.
Contraindications
The use of cetrorelix is contraindicated in severe renal impairment. It is not intended for women aged 65 years or older. Use in women with severe allergic conditions is not recommended. Use with caution in women with active allergies or history of allergies.
Mechanism of action
A synthetic decapeptide. The drug works by blocking the action of GnRH upon the pituitary, thus rapidly suppressing the production and action of luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
Research
Cetrorelix was under development for the treatment of benign prostatic hyperplasia, premenopausal breast cancer, endometriosis, ovarian cancer, prostate cancer, and uterine fibroids, but development for these indications was discontinued.[7]
A study published in Nature Medicine found a link between hormonal imbalance in the womb and Polycystic ovary syndrome (PCOS), specifically prenatal exposure to anti-Müllerian hormone. [8] For the study, the researchers injected pregnant mice with AMH so that they had a higher than normal concentration of the hormone. Indeed, they gave birth to daughters who later developed PCOS-like tendencies. These included problems with fertility, delayed puberty, and erratic ovulation. To reverse it, the researchers dosed the polycystic mice with cetrorelix, which made the symptoms to go away. These experiments should be confirmed in humans, but it could be the first step in understanding the relationship between the polycystic ovary and the anti-Müllerian hormone.
Over a period of 3 weeks, daily injections of cetrorelix were administered to 12 men in order to suppress testosterone levels. Testosterone levels were suppressed as compared to a control group. During this time of suppression, increases in high density lipoproteins (HDLs) were seen. HDLs are responsible for removing cholesterol from the blood and higher amounts are correlated with increased cardiovascular health.[9]
See also
- Gonadotropin-releasing hormone receptor § Antagonists
References
- 1 2 3 4 5 6 7 "Cetrorelix Monograph for Professionals". Drugs.com. Archived from the original on 4 February 2021. Retrieved 3 January 2022.
- 1 2 3 "Cetrotide". Archived from the original on 16 May 2021. Retrieved 3 January 2022.
- 1 2 BNF 81: March-September 2021. BMJ Group and the Pharmaceutical Press. 2021. p. 778. ISBN 978-0857114105.
- ↑ "Cetrorelix Prices, Coupons & Savings Tips - GoodRx". GoodRx. Retrieved 3 January 2022.
- ↑ Aeternia Zentaris product page
- ↑ Lin YH, Wen YR, Chang Y, Seow KM, Hsieh BC, Hwang JL, Tzeng CR (June 2010). "Safety and efficacy of mixing cetrorelix with follitropin alfa: a randomized study". Fertility and Sterility. 94 (1): 179–83. doi:10.1016/j.fertnstert.2009.02.062. PMID 19339001.
- ↑ "Cetrorelix". AdisInsight. Archived from the original on 2017-12-25. Retrieved 2021-01-31.
- ↑ Tata B, Mimouni NE, Barbotin AL, Malone SA, Loyens A, Pigny P, et al. (June 2018). "Elevated prenatal anti-Müllerian hormone reprograms the fetus and induces polycystic ovary syndrome in adulthood". Nature Medicine. 24 (6): 834–846. doi:10.1038/s41591-018-0035-5. PMC 6098696. PMID 29760445.
- ↑ von Eckardstein A (1997). "Suppression of Endogenous Testosterone in Young Men Increases Serum Levels of High Density Lipoprotein Subclass Lipoprotein A-I and Lipoprotein(a)". Journal of Clinical Endocrinology. 82 (10): 3367.
External links
| Identifiers: |
|---|
- "Cetrorelix". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 2020-10-22. Retrieved 2021-01-31.
- "Cetrorelix acetate". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 2021-02-04. Retrieved 2021-01-31.