Cocaine use disorder
| Cocaine use disorder | |
|---|---|
| Other names: Cocaine dependence, cocaine addiction, cocaine misuse, cocaine abuse | |
| Video explanation | |
| Specialty | Psychiatry |
| Symptoms | Taking more than was intended, ongoing desire to use, use resulting in work or school issues, not stopping despite health problems[1] |
| Complications | Heart disease, HIV/AIDS, hepatitis C, muscle breakdown, homelessness[2][3] |
| Risk factors | Adult ADHD, schizophrenia, antisocial personality disorder, other substance use disorders, unstable home environment[1][4] |
| Diagnostic method | Urine drug screen[1] |
| Treatment | Contingency management programs, cognitive behavioral therapy[2] |
| Frequency | 0.4% of adults[5] |
Cocaine use disorder (CUD) is cocaine use in a manner that results in significant impairment.[1] This may involve taking more than was intended, ongoing desire to use, use resulting in work or school issues, and not stopping despite health problems from such use.[1] Other symptoms may include those of cocaine intoxication, cocaine withdrawal, psychosis, and weight lose.[3] Complications may include heart disease, HIV/AIDS, hepatitis C, muscle breakdown, and homelessness.[2][3] Use is associated with anxiety disorders and depression.[3]
Risk factors included adult ADHD, with 10% being affected, schizophrenia, antisocial personality disorder, other substance use disorders, and an unstable home environment.[1][4] The severity can be divided into mild, moderate, and severe.[3] Diagnosis may be supported by a urine drug screen, which may remains positive 3 days after a single use and 12 days after heavy use.[1]
The evidence for specific treatments is limited.[2] Efforts may include contingency management programs, which provides vouchers for avoiding use, and cognitive behavioral therapy.[2][6] No medications have been approved for this use.[6] Evidence for providing other stimulants is insufficient as of 2020.[2]
About 19 million people used cocaine in 2018 (0.4% of adults).[5] Use is most common in Australia, North America and Europe.[5] About a million people in the United States have cocaine use disorder.[6] In Uruguay 43% of people who used cocaine were considered to have cocaine use disorder.[5] Young adults are most commonly affected.[1][3] In the United States, in 2019, nearly 16,000 overdose deaths involved cocaine.[7]
Signs and symptoms

Cocaine is a stimulant known to make users feel energetic, cheerful, talkative, etc. In time, negative side effects include increased body temperature, irregular or rapid heart rate, high blood pressure, increased risk of heart attacks, strokes and even sudden death from cardiac arrest.[8] Many habitual abusers develop a transient, manic-like condition similar to amphetamine psychosis and schizophrenia, whose symptoms include aggression, severe paranoia, restlessness, confusion[9] and tactile hallucinations; which can include the feeling of something crawling under the skin (formication), also known as "coke bugs", during binges.[10] Users of cocaine have also reported having thoughts of suicide, unusual weight loss, trouble maintaining relationships, and an unhealthy, pale appearance.[9]
Withdrawal
After using cocaine on a regular basis, many users will become addicted. When the drug is discontinued immediately, the user will experience what has come to be known as a "crash" along with a number of other cocaine withdrawal symptoms, including paranoia, depression, exhaustion, anxiety, itching, mood swings, irritability, fatigue, insomnia, an intense craving for more cocaine, and in some cases nausea and vomiting. Some cocaine users also report having similar symptoms to schizophrenia patients and feel that their mind is lost. Some users also report formication: a feeling of a crawling sensation on the skin also known as "coke bugs". These symptoms can last for weeks or, in some cases, months. Even after most withdrawal symptoms dissipate most users feel the need to continue using the drug; this feeling can last for years and may peak during times of stress. About 30–40% of individuals with cocaine dependence will turn to other substances such as medication and alcohol after giving up cocaine. There are various medications on the market to ease cocaine withdrawal symptoms.
Risk
A study consisting of 1,081 U.S. residents who had first used cocaine within the previous 24 months was conducted. It was found that the risk of becoming dependent on cocaine within two years of first use was 5–6%. The risk of becoming dependent within 10 years of first use increased to 15–16%. These were the aggregate rates for all types of use considered, such as smoking, snorting, and injecting. Among recent-onset users individual rates of dependency were higher for smoking (3.4 times) and much higher for injecting. Women were 3.3 times more likely to become dependent, compared with men. Users who started at ages 12 or 13 were four times as likely to become dependent compared to those who started between ages 18 and 20.[11][12][13]
Treatment
Therapy
Twelve-step programs such as Cocaine Anonymous (modeled on Alcoholics Anonymous) have been widely used to help those with cocaine addiction. Cognitive behavioral therapy (CBT) combined with motivational therapy (MT) have proven to be more helpful than 12 step programs in treating cocaine dependency.[14] However, both these approaches have a fairly low success rate. Other non-pharmacological treatments such as acupuncture[15][16] and hypnosis have been explored, but without conclusive results.[17][18]
Medications
Numerous medications have been investigated for use in cocaine dependence, but as of 2015, none of them were considered to be effective.[19] Anticonvulsants, such as carbamazepine, gabapentin, lamotrigine, and topiramate, do not appear to be effective as treatment.[19][20] Limited evidence suggests that antipsychotics are also ineffective for treatment of cocaine dependence.[21] Few studies have examined bupropion (a novel antidepressant) for cocaine dependence; however, trials performed thus far have not shown it to be an effective form of treatment for this purpose.[22]
The National Institute on Drug Abuse (NIDA) of the U.S. National Institutes of Health is researching modafinil, a narcolepsy drug and mild stimulant, as a potential cocaine treatment. Ibogaine has been under investigation as a treatment for cocaine dependency and is used in clinics in Mexico, the Netherlands and Canada, but cannot be used legally in the United States. Other medications that have been investigated for this purpose include acetylcysteine, baclofen,[23] and vanoxerine.[24] Medications such as phenelzine, have been used to cause an "aversion reaction" when administered with cocaine.[lower-alpha 1]
Epidemiology
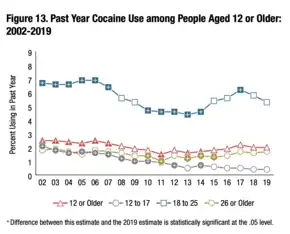
In the United States, past year cocaine users in 2019 was 5.5 million for people aged 12 or older. When broken into age groups, ages 12–17 had 97,000 users; ages 18–25 had 1.8 million users and ages 26 or older had 3.6 million users.[26]
Past year cocaine users with a cocaine use disorder in 2019 was 1 million for people aged 12 or older. When broken into age groups, ages 12–17 had 5,000 people with a cocaine use disorder; ages 18–25 had 250,000 people with a cocaine use disorder and ages 26 or older had 756,000 people with a cocaine use disorder[26]
In the United States, cocaine use overdose deaths have been on the rise and in 2019, the CDC reported over 16,000 deaths from cocaine overdose.[27]
Research
Kim Janda has been working for years on a vaccination that would treat cocaine use disorders[28] by limiting its rewarding effects.[29] TA-CD is an active vaccine which negate the effects of cocaine, making it suitable for use in treatment of addiction. It is created by combining norcocaine with inactivated cholera toxin.[30]
Transcranial magnetic stimulation (TMS) is being studied as a treatment for cocaine addiction. So far studies have been undertaken by Medical University of South Carolina (MUSC), National Institute on Drug Abuse (NIDA), and Mexican National Institute of Psychiatry.[31]
See also
- SB-277011-A – a dopamine D3 receptor antagonist, used in the study of cocaine addiction. Where cocaine reduces the threshold for brain electrical self-stimulation in rats, an indication of cocaine's rewarding effects, SB-277011-A completely reverses this effect.
References
- 1 2 3 4 5 6 7 8 Diagnostic and Statistical Manual of Mental Disorders (Fifth ed.). American Psychiatric Association. 2013. pp. 561. doi:10.1176/appi.books.9780890425596.156852. ISBN 978-0-89042-555-8.
{{cite book}}: Cite has empty unknown parameter:|1=(help) - 1 2 3 4 5 6 Ronsley, Claire; Nolan, Seonaid; Knight, Rod; Hayashi, Kanna; Klimas, Jano; Walley, Alex; Wood, Evan; Fairbairn, Nadia (18 June 2020). "Treatment of stimulant use disorder: A systematic review of reviews". PLOS ONE. 15 (6): e0234809. doi:10.1371/journal.pone.0234809.
- 1 2 3 4 5 6 Ryan, SA (December 2019). "Cocaine Use in Adolescents and Young Adults". Pediatric clinics of North America. 66 (6): 1135–1147. doi:10.1016/j.pcl.2019.08.014. PMID 31679603.
- 1 2 Oliva, F; Mangiapane, C; Nibbio, G; Berchialla, P; Colombi, N; Vigna-Taglianti, FD (9 November 2020). "Prevalence of cocaine use and cocaine use disorder among adult patients with attention-deficit/hyperactivity disorder: A systematic review and meta-analysis". Journal of psychiatric research. doi:10.1016/j.jpsychires.2020.11.021. PMID 33199055.
- 1 2 3 4 WORLD DRUG REPORT 2020 (SET OF 6 BOOKLETS) (PDF). [S.l.]: UNITED NATIONS. 2020. pp. 25–30. ISBN 978-92-1-148345-1. Archived (PDF) from the original on 29 January 2021. Retrieved 20 February 2021.
- 1 2 3 Kampman, KM (October 2019). "The treatment of cocaine use disorder". Science advances. 5 (10): eaax1532. doi:10.1126/sciadv.aax1532. PMID 31663022.
- ↑ "Overdose Death Rates". National Institute on Drug Abuse. 29 January 2021. Archived from the original on 25 January 2018. Retrieved 26 February 2021.
- ↑ Walsh, Karen (October 2010). "Teen Cocaine Use". Archived from the original on 13 February 2018. Retrieved 12 December 2013.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 LeVert, Suzanne (2006). Drugs: The Facts About Cocaine. New York: Marshall Cavendish Benchmark. pp. 41, 76.
- ↑ Gawin, F.H. (1991). "Cocaine addiction: Psychology and neurophysiology". Science. 251 (5001): 1580–6. Bibcode:1991Sci...251.1580G. doi:10.1126/science.2011738. PMID 2011738. S2CID 26660048.
- ↑ Tierney, John. "The Rational Choices of Crack Addicts". New York Times. Archived from the original on 20 September 2013. Retrieved 16 September 2013.
- ↑ Wagner, FA (2002), "From first drug use to drug dependence; developmental periods of risk for dependence upon marijuana, cocaine, and alcohol", Neuropsychopharmacology, 26 (4): 479–88, doi:10.1016/S0893-133X(01)00367-0, PMID 11927172
- ↑ O'Brien MS, Anthony JC (2005). "Risk of becoming cocaine dependent: epidemiological estimates for the United States, 2000–2001". Neuropsychopharmacology. 30 (5): 1006–1018. doi:10.1038/sj.npp.1300681. PMID 15785780.
- ↑ "Cognitive behavioural therapy reduced cocaine abuse compared with 12 step facilitation". ebmh.bmj.com. 17 January 2008. Archived from the original on 17 February 2012. Retrieved 25 August 2012.
- ↑ Margolin, Arthur; et al. (2 January 2002). "Acupuncture for the treatment of cocaine addiction: A randomized controlled trial". The Journal of the American Medical Association. 287 (1): 55–63. doi:10.1001/jama.287.1.55. PMID 11754709.
- ↑ Otto, Katharine C.; Quinn, Colin; Sung, Yung-Fong (Spring 1998). "Auricular acupuncture as an adjunctive treatment for cocaine addiction: A pilot study". The American Journal on Addictions. 7 (2): 164–170. doi:10.1111/j.1521-0391.1998.tb00331.x. PMID 9598220.
- ↑ Page, R.A.; Handleya, G.W. (1993). "The use of hypnosis in cocaine addiction". American Journal of Clinical Hypnosis. 36 (2): 120–123. doi:10.1080/00029157.1993.10403054. PMID 8259763.
- ↑ Potter, Greg (2004). "Intensive therapy: Utilizing hypnosis in the treatment of substance abuse disorders". American Journal of Clinical Hypnosis. 47 (1): 21–28. doi:10.1080/00029157.2004.10401472. PMID 15376606. S2CID 42943267.
- 1 2 Minozzi, S; Cinquini, M; Amato, L; Davoli, M; Farrell, MF; Pani, PP; Vecchi, S (April 2015). "Anticonvulsants for cocaine dependence". Cochrane Database of Systematic Reviews (Systematic Review & Meta-Analysis). 17 (4): CD006754. doi:10.1002/14651858.CD006754.pub4. PMID 25882271.
- ↑ Singh, M; Keer, D; Klimas, J; Wood, E; Werb, D (August 2016). "Topiramate for cocaine dependence: a systematic review and meta-analysis of randomized controlled trials". Addiction (Systematic Review & Meta-Analysis). 111 (8): 1337–46. doi:10.1111/add.13328. PMID 26826006. S2CID 34637139.
- ↑ Indave, BI; Minozzi, S; Pani, PP; Amato, L (March 2016). "Antipsychotic medications for cocaine dependence". Cochrane Database of Systematic Reviews (Systematic Review and Meta-Analysis). 3: CD006306. doi:10.1002/14651858.CD006306.pub3. PMID 26992929.
- ↑ Mariani, JJ; Levin, FR (June 2012). "Psychostimulant treatment of cocaine dependence". Psychiatric Clinics of North America (Review). 35 (2): 425–39. doi:10.1016/j.psc.2012.03.012. PMC 3417072. PMID 22640764.
- ↑ Karila L; Gorelick D; Weinstein A; et al. (May 2008). "New treatments for cocaine dependence: a focused review". Int. J. Neuropsychopharmacol. 11 (3): 425–38. doi:10.1017/S1461145707008097. PMID 17927843.
- ↑ Cherstniakova SA, Bi D, Fuller DR, Mojsiak JZ, Collins JM, Cantilena LR (September 2001). "Metabolism of vanoxerine, 1-[2-[bis(4-fluorophenyl)methoxy]ethyl]-4-(3-phenylpropyl)piperazine, by human cytochrome P450 enzymes". Drug Metab. Dispos. 29 (9): 1216–20. PMID 11502731. Archived from the original on 28 August 2021. Retrieved 17 November 2009.
- ↑ "Chemistry, Design, and Structure-Activity Relationship of Cocaine Antagonists" Archived 4 March 2016 at the Wayback Machine. Satendra Singh et al. Chem. Rev. 2000, 100. 925-1024. PubMed; Chemical Reviews (Impact Factor: 45.66). 04/2000; 100(3):925-1024 American Chemical Society; 2000, ISSN 0009-2665 ChemInform; May, 16th 2000, Volume 31, Issue 20, DOI: 10.1002/chin.200020238. Mirror hotlink. Archived 3 July 2015 at the Wayback Machine
- 1 2 "National Survey on Drug Use and Health". nsduhweb.rti.org. Archived from the original on 4 March 2014. Retrieved 9 May 2021.
- ↑ Abuse, National Institute on Drug. "Cocaine". National Institute on Drug Abuse. Archived from the original on 25 January 2022. Retrieved 1 May 2021.
- ↑ Douglas Quenqua (3 October 2011). "An Addiction Vaccine, Tantalizingly Close". The New York Times. Archived from the original on 16 July 2017. Retrieved 15 November 2019.
- ↑ "Baylor Doctors are Working on Cocaine Vaccine". CocaineHelp.org. 17 January 2008. Archived from the original on 9 May 2008. Retrieved 11 September 2008.
- ↑ Martell BA, Mitchell E, Poling J, Gonsai K, Kosten TR (July 2005). "Vaccine pharmacotherapy for the treatment of cocaine dependence". Biol. Psychiatry. 58 (2): 158–64. doi:10.1016/j.biopsych.2005.04.032. PMID 16038686. S2CID 22415520.
- ↑ Wadman, Meredith (29 August 2017). "Brain-altering magnetic pulses could zap cocaine addiction". Science Magazine. American Association for the Advancement of Science. Archived from the original on 2 September 2017. Retrieved 1 September 2017.
Reference notes
External links
| Classification | |
|---|---|
| External resources |