Congenital Zika syndrome
| Congenital Zika syndrome | |
|---|---|
 | |
| Congenital Zika syndrome | |
| Specialty | Pediatrics |
| Symptoms | Small head, visual problems, contractures, stiffness[1] |
| Usual onset | Newborn baby[2] |
| Causes | Zika virus[2] |
| Risk factors | Zika virus infection in mother[2] |
| Diagnostic method | History, symptoms, blood/urine tests, medical imaging[2] |
| Differential diagnosis | Congenital toxoplasmosis, congenital syphilis, congenital varicella syndrome, parvovirus B19, congenital rubella, congenital cytomegalovirus infection, congenital herpes simplex, Aicardi-Goutières syndrome[2] |
| Prevention | Avoiding mosquito bites, mosquito control, birth control education[3] |
| Treatment | Supportive care[3] |
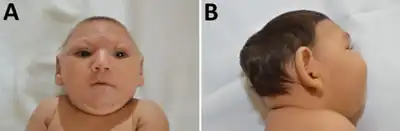
Congenital Zika syndrome presents as birth defects in a newborn baby of some mothers infected with Zika virus during pregnancy.[1] Symptoms typically include a small head, visual problems, contractures, and stiffness.[1] Less frequently heart problems, ambiguous genitalia, undescended testes, bowel problems, difficulty swallowing, hearing problems, or a small baby may occur.[2] Complications may include miscarriage or stillbirth.[2]
The cause is infection by the Zika virus, a type of flavivirus, during pregnancy.[2] Most infected mothers and their babies have no or mild symptoms.[4] Congenital Zika syndrome can occur regardless of whether the mother had symptoms.[3] Diagnosis is supported by detecting the virus in the mother, particularly if there are symptoms or a history of travel to an area with the Aedes mosquito.[3] Blood tests may confirm the diagnosis and distinguish Zika from Dengue.[3] Ultrasound may detect symptoms in the unborn baby.[2] MRI of the brain of the baby may show a collapsed skull and small brain.[2]
Treatment of Zika infection is supportive, with rest and hydration.[3] Prevention is by avoiding mosquito bites, mosquito control, and birth control education.[3]
Congenital Zika syndrome affects around 10% of babies born to mothers who had Zika infection during pregnancy.[3] The link between Zika and microcephaly was first documented in 2015 in Brazil.[2] The following year Zika was declared a Public Health Emergency of International Concern by the World Health Organization.[2] Limitations to diagnosis include the high cost of testing for Zika.[2] The Zika virus was first isolated in 1954 in Nigeria.[2]
Signs and symptoms
Symptoms typically include a small head, visual problems, contractures, and stiffness.[1] Less frequently heart problems, ambiguous genitalia, undescended testes, bowel problems, difficulty swallowing, hearing problems, or a small baby may occur.[2] Other abnormal nerve development consequences include, dystonia, tremors, mental disability, and hearing loss.[4]
In the eyes there may be scarring in the eyes and underdevelopment of the optic nerve.[4]
 Finger deformities
Finger deformities Clubfeet
Clubfeet Knee dislocation
Knee dislocation Knee contracture
Knee contracture Joint contractures
Joint contractures
Diagnosis
Testing is recommended by the CDC for all babies born to mothers who test positive for Zika, and all babies with symptoms of Zika virus.[4] This is typically by RT-PCR and antibody testing on blood, and ZIKV RT-PCR on urine.[4]
 MRI- bilateral dislocation of hips, epiphyseal core (small arrow), and dysplastic acetabulum (large arrow)
MRI- bilateral dislocation of hips, epiphyseal core (small arrow), and dysplastic acetabulum (large arrow) X-ray knees
X-ray knees CT hips
CT hips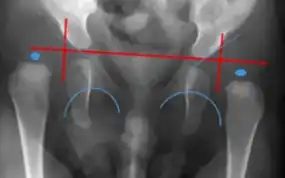 X-ray- dislocation of hips
X-ray- dislocation of hips
See also
References
- 1 2 3 4 "Congenital Zika Syndrome & Other Birth Defects | CDC". Centers for Disease Control and Prevention. 22 April 2022. Archived from the original on 12 June 2023. Retrieved 8 September 2023.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Freitas, Danielle A.; Souza-Santos, Reinaldo; Carvalho, Liege M. A.; Barros, Wagner B.; Neves, Luiza M.; Brasil, Patrícia; Wakimoto, Mayumi D. (15 December 2020). "Congenital Zika syndrome: A systematic review". PLoS ONE. 15 (12): e0242367. doi:10.1371/journal.pone.0242367. ISSN 1932-6203. Archived from the original on 9 June 2022. Retrieved 9 September 2023.
- 1 2 3 4 5 6 7 8 "Zika virus". www.who.int. World Health Organization. Archived from the original on 26 January 2023. Retrieved 12 September 2023.
- 1 2 3 4 5 Hills, Susan L.; Woodworth, Kate R. (2022). "92. Zika virus disease and congenital Zika virus disease". In Jong, Elaine C.; Stevens, Dennis L. (eds.). Netter's Infectious Diseases (2nd ed.). Philadelphia: Elsevier. pp. 556–561. ISBN 978-0-323-71159-3. Archived from the original on 2023-09-13. Retrieved 2023-09-12.