Erythroderma
| Erythroderma | |
|---|---|
| Other names: Exfoliative dermatitis, Dermatitis exfoliativa | |
_Skin_Syndrome_-_Feet_Collage.jpg.webp) | |
| Red skin syndrome | |
Erythroderma is an inflammatory skin disease with redness and scaling that affects nearly the entire cutaneous surface.[1][2] This term applies when 90% or more of the skin is affected.[3]
In ICD-10, a distinction is made between "exfoliative dermatitis" at L26, and "erythroderma" at L53.9.
Symptoms and signs
The presentation of erythroderma may affect most of an individuals skin, additionally being red, dry skin, and cause fever. [4]
_(DermNet_NZ_reactions-erythroderma-14).jpg.webp) Erythroderma
Erythroderma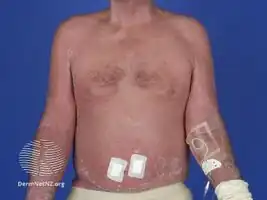 Erythroderma
Erythroderma_(DermNet_NZ_reactions-erythroderma-16).jpg.webp) Erythroderma
Erythroderma
Causes
Erythroderma is generalized exfoliative dermatitis, which involves 90% or more of the patient's skin.[5] The most common cause of erythroderma is exacerbation of an underlying skin disease, such as psoriasis, contact dermatitis, seborrheic dermatitis, lichen planus, pityriasis rubra pilaris or a drug reaction, such as the use of topical steroids.[6] Primary erythroderma is less frequent and is usually seen in cases of cutaneous T-cell lymphoma, in particular in Sézary's disease.[7]
The most common causes of exfoliative dermatitis are best remembered by the mnemonic device ID-SCALP.[5] The causes and their frequencies are as follows:
- Idiopathic - 30%
- Drug allergy - 28%
- Seborrheic dermatitis - 2%
- Contact dermatitis - 3%
- Atopic dermatitis - 10%
- Lymphoma and leukemia - 14%
- Psoriasis - 8%
Treatment
The treatment for erythroderma depends on the primary cause. Topical steroids and use of a sauna suit are often used to treat exfoliative dermatitis regardless of the cause. Retinoids and immunosuppressive drugs can be used when it is caused by psoriasis or pityriasis rubra pilaris.[2] A sedative antihistamine may be a useful adjunct for pruritic patients, since it helps patients to sleep at night, thus limiting nocturnal scratching and excoriations. Antimicrobial agents often are used if an infection is suspected to be precipitating or complicating exfoliative dermatitis. Other drugs specifically indicated for management of underlying cause of exfoliative dermatitis may be necessary.[5]
Epidemiology
The incidence of erythroderma is estimated to be 1-2 in 100,000.[8] While erythroderma can occur at any age, it is most common in older, male adults.
History
The classification of exfoliative dermatitis into Wilson-Brocq (chronic relapsing), Hebra or pityriasis rubra (progressive), and Savill (self-limited) types may have had historical value, but it currently lacks pathophysiologic or clinical utility.[1]
References
- 1 2 Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. p. 436. ISBN 0-07-138076-0.
- 1 2 James, William D.; Elston, Dirk M.; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac M. (2020). "Pityriasis Rosea, Pityriasis Rubra Pilaris, and Other Papulosquamous and Hyperkeratotic Diseases". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh. pp. 205–214. ISBN 9780323547536.
- ↑ Japp, Alan G.; Robertson, Colin; Wright, Rohana J.; Reed, Matthew J.; Robson, Andrew (2018). "27. Rash: acute generalised skin eruption". Macleod's Clinical Diagnosis (2nd ed.). Elsevier. pp. 240–245. ISBN 978-0-7020-6962-8. Archived from the original on 2022-11-15. Retrieved 2022-11-16.
- ↑ "erythroderma (Concept Id: C0011606) - MedGen - NCBI". www.ncbi.nlm.nih.gov. Archived from the original on 28 August 2021. Retrieved 23 July 2021.
- 1 2 3 Umar, Sanusi H. (5 December 2020). "Erythroderma (Generalized Exfoliative Dermatitis): Background, Pathophysiology, Etiology". eMedicine. Medscape. Archived from the original on 23 January 2021. Retrieved 15 January 2021.
- ↑ Fukaya, Mototsugu (2000). Withdrawal from corticosteroids in patients with atopic dermatitis. www.tclinic.jp. Archived from the original on December 23, 2014.
{{cite book}}: CS1 maint: unfit URL (link) - ↑ "Dermatology: An Illustrated Colour Text - David J. Gawkrodger - Google Books". web.archive.org. June 16, 2013. Archived from the original on June 16, 2013. Retrieved January 15, 2021.
{{cite web}}: CS1 maint: bot: original URL status unknown (link) - ↑ Sigurdsson, V (November 2001). "The incidence of erythroderma: a survey among all dermatologists in The Netherlands". Journal of the American Academy of Dermatology. 45 (5): 675–678. doi:10.1067/mjd.2001.116224. PMID 11606915.
External links
| Classification | |
|---|---|
| External resources |