Lichen nitidus
| Lichen nitidus | |
|---|---|
 | |
| Photography of lichen nitidus: A) Glistening forearm papules; B) Papular lesions of lower limbs | |
| Specialty | Dermatology |
| Symptoms | Tiny, discrete and uniform, shiny, flat-topped, pale flesh-colored or reddish-brown bumps in skin, Koebner phenomenon[1] |
| Duration | Few years[2] |
| Causes | Unknown[1] |
| Risk factors | Children, young adults, darker skin[2] |
| Diagnostic method | Visualisation, biopsy[2] |
| Treatment | Sun protection, corticosteroids, antihistamine[1][2] |
| Medication | Triamcinolone ointment 1% twice daily for 14-days,[2] fexofenadine 180mg daily and hydroxyzine 25-50mg at night as needed[2] |
| Prognosis | Progresses slowly, can resolve spontaneously, harmless[1] |
| Frequency | Uncommon[2] |
Lichen nitidus is a longterm inflammatory skin disease, characterized by tiny bumps in the skin.[1] These are typically discrete and uniform, shiny, flat-topped, pale flesh-colored or reddish-brown, and usually affect the penis, forearms, lower tummy, inner wrists and backs of hands in a localised pattern or in a line.[1] They may appear as pale dots against dark skin.[1] Occasionally, minimal scaling is present or can be induced by rubbing the surface of the bumps.[2][3] It is painless and usually not itchy.[4]
The cause is unknown.[1][5] Some cases have been associated with tattoos.[1] It tends to last a few years before it spontaneously resolves.[2] Diagnosis is by visualisation and sometimes biopsy, which shows infiltration of lymphocytes in the top layer of the skin.[2]
Treatment includes sun protection, corticosteroids, and antihistamine.[1][2] Application of triamcinolone ointment 1% twice daily for 14-days, fexofenadine 180mg daily by mouth and hydroxyzine 25-50mg at night by mouth as and when required, may be used if symptoms.[2]
The disease is uncommon.[2]The incidence is around 3.4 cases per 10,000 people, and generally affects darker skin types.[2] It usually affects children and young adults.[6] Felix Pinkus first described the condition in 1907.[7]
Signs and symptoms
Linear arrangements of these papules is common (referred to as a Koebner phenomenon), especially on the forearms,[1] but may occasionally be grouped, though not confluent, on flexural areas.[1] Generally, the initial lesions are localized, and remain so, to the chest, abdomen, glans penis, and flexor aspects of the upper extremities;[8] however, less commonly, the disease process can (1) be strictly isolated to the palms and soles,[9] presenting with many hyperkeratotic, yellow papules that may coalesce into plaques that fissure[3][9] or “...sometimes a non-specific keratoderma resembling chronic eczema,”[9] or (2) become more widespread, with papules widely distributed on the body—the extensor surfaces of the elbows, wrists, and hands, folds of the neck, submammary region in females, groin, thighs, ankles, and feet[10]>[1]—and fusing into erythematous, minimally scaled plaques, with redness that develops tints of violet, brown, and yellow.[3][11]
.jpg.webp) Lichen nitidus
Lichen nitidus.jpg.webp) Lichen nitidus
Lichen nitidus.jpg.webp) Lichen nitidus
Lichen nitidus
Pathology
The histology of lichen nitidus is significant for a "...localized granulomatous lymphohistiocytic infiltrate in an expanded dermal papilla with thinning of overlying epidermis and downward extension of the rete ridges at the lateral margin of the infiltrate, producing a typical 'claw clutching a ball' picture...."[10]
.jpg.webp) Lichen nitidus
Lichen nitidus.jpg.webp) Lichen nitidus
Lichen nitidus.jpg.webp) Lichen nitidus
Lichen nitidus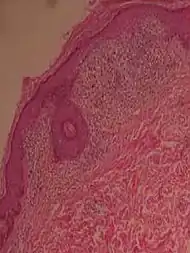 Histopathology of lichen nitidus: Downward extension of the rete ridges at the lateral margins of a lymphohistiocytic infiltrate, resulting in a typical "claw clutching a ball" appearance.
Histopathology of lichen nitidus: Downward extension of the rete ridges at the lateral margins of a lymphohistiocytic infiltrate, resulting in a typical "claw clutching a ball" appearance.
Treatment
Generally, lichen nitidus is asymptomatic and self-limited; therefore, no treatment is required. However, if persistent pruritus is present, or the appearance “...interferes with daily activities or outlook...”[1] topical glucocorticoids may be tried. If the disease process is symptomatic, generalized and extensive, oral glucocorticoids may be indicated.[1] Other reported treatments include PUVA, UVA/UVB phototherapy,[8] astemizole,[10] acitretin, and etretinate.[1] When appears with sun/humidity; air conditioning (cool dry air) reduces swelling and discomfort.
History
The German dermatologist, Felix Pinkus, first described the condition in 1907.[7]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "12. Lichen planus and related conditions". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. pp. 225–226. ISBN 978-0-323-54753-6. Archived from the original on 2023-04-28. Retrieved 2023-04-28.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Lim, Henry W. (2020). "409. Eczemas, photodermatoses, papulomatoses, papulosquamous (including fungal) diseases, and figurate erythema: Lichen nitidus". In Goldman, Lee; Schafer, Andrew I. (eds.). Goldman-Cecil Medicine. Vol. 2 (26th ed.). Philadelphia: Elsevier. p. 2618. ISBN 978-0-323-53266-2.
- 1 2 3 Fitzpatrick, Thomas B.; Freedberg, Irwin M. (1999). Fitzpatrick's dermatology in general medicine. New York: McGraw-Hill, Health Professions Division. pp. 577–81. ISBN 0-07-912938-2.
- ↑ Schwartz, C; Goodman, MB (10 July 2021). "Lichen Nitidus". StatPearls. PMID 31869173. Archived from the original on 25 April 2021. Retrieved 6 April 2022.
- ↑ Inamadar, Arun C.; Palit, Aparna; Ragunatha, S. (2014). Textbook of Pediatric Dermatology (2nd ed.). New Delhi: JP Medical Ltd. pp. 385–386. ISBN 978-93-5152-083-2. Archived from the original on 2022-04-06. Retrieved 2022-04-06.
- ↑ Johnstone, Ronald B. (2017). "3. Lichenoid reaction pattern". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 39. ISBN 978-0-7020-6830-0. Archived from the original on 2021-05-25. Retrieved 2022-04-07.
- 1 2 Crissey, John Thorne; Parish, Lawrence C.; Holubar, Karl (2002). Historical Atlas of Dermatology and Dermatologists. New York: CRC Press. p. 122. ISBN 1-84214-100-7. Archived from the original on 2022-04-06. Retrieved 2022-04-06.
- 1 2 Do MO, Kim MJ, Kim SH, Myung KB, Choi YW (2007). "Generalized Lichen Nitidus Successfully Treated with Narrow-band UVB Phototherapy : Two Cases Report". J. Korean Med. Sci. 22 (1): 163–6. doi:10.3346/jkms.2007.22.1.163. PMC 2693559. PMID 17297274.
- 1 2 3 Thibaudeau A, Maillard H, Croué A, Belperron P, Avenel Audran M, Verret JL (2004). "[Palmoplantar lichen nitidus: a rare cause of palmoplantar hyperkeratosis.]". Ann Dermatol Venereol (in français). 131 (8–9): 822–4. doi:10.1016/S0151-9638(04)93769-6. PMID 15505553.
- 1 2 3 Al-Mutairi N, Hassanein A, Nour-Eldin O, Arun J (2005). "Generalized lichen nitidus". Pediatr Dermatol. 22 (2): 158–60. doi:10.1111/j.1525-1470.2005.22215.x. PMID 15804308.
- ↑ Soroush V, Gurevitch AW, Peng SK (1999). "Generalized lichen nitidus: case report and literature review". Cutis. 64 (2): 135–6. PMID 10467510.
External links
| Classification | |
|---|---|
| External resources |
- Lichen Nitidus Archived 2011-09-03 at the Wayback Machine at DermNet photo library