Focal nodular hyperplasia
| Focal nodular hyperplasia | |
|---|---|
 | |
| Micrograph of focal nodular hyperplasia. H&E stain. | |
Focal nodular hyperplasia (FNH) is a benign tumor of the liver (hepatic tumor), which is the second most prevalent tumor of the liver (the first is hepatic hemangioma). It is usually asymptomatic, rarely grows or bleeds, and has no malignant potential. This tumour was once often resected because it was difficult to distinguish from hepatic adenoma, but with modern multiphase imaging is usually now diagnosed by strict imaging criteria and not resected.
Signs and symptoms
Focal nodular hyperplasia's most recognizable gross feature is a central stellate scar seen in 60–70% of cases. Microscopically, a lobular proliferation of bland-appearing hepatocytes with a bile ductular proliferation and malformed vessels within the fibrous scar is the most common pattern. Other patterns include telangiectatic, hyperplastic-adenomatous, and lesions with focal large-cell dysplasia.[1] Rarely, these lesions may be multiple or can occur as part of a syndrome with hemangiomas, epithelioid hemangioendothelioma, hepatic adenomas, fibrolamellar hepatocellular carcinoma, vascular malformations of the brain, meningiomas, and/or astrocytomas.[1]
Pathophysiology
FNH is not a true neoplasm; it is believed to result from localized hyperplastic hepatocyte response to an underlying congenital arteriovenous malformation. It consists of normal liver constituents in an abnormally organized pattern, grows in a stellate pattern and may display central necrosis when large.[2] Additionally evidence suggests that the incidence of FNH is related to oral contraceptive use.[3]
Diagnosis
 Map-like pattern of staining of glutamine synthetase in FNH * as compared to normal liver **
Map-like pattern of staining of glutamine synthetase in FNH * as compared to normal liver **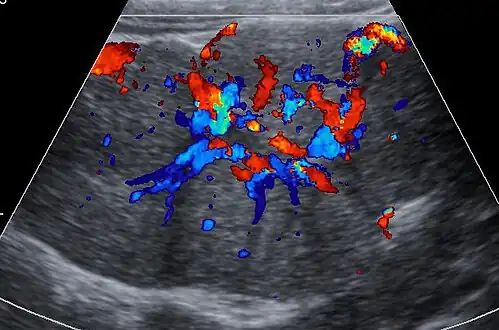 Ultrasound of malformed vessels within the fibrous scar of FNH.
Ultrasound of malformed vessels within the fibrous scar of FNH.
Unenhanced CT or MRI usually does not show the difference in intensity between the FNH and surrounding liver except when there is marked liver steatosis that reduces the attenuation of the liver, causing FNH to be hyperattenuating when compared with the surrounding liver. In the arterial phase CT or MRI, there is a strong enhancement not followed by washout. The lesion presents a slight hyperintensity or isodensity on portal venous phase or delayed phase images. There is also a presence of a central scar and absence of a capsule for the FNH.[4]
Treatment
In terms of the management of FNH surgical resection is possible[5]
Epidemiology

The prevalence of FNH of individuals undergoing evaluation with an ultrasound of the abdomen is 0.03%.[7] About 20% of FNH lesions are associated with hepatic hemangiomas.[7]
Notes
- 1 2 Nguyen, Bich N.; Fléjou, Jean-François; Terris, Benoit; Belghiti, Jacques; Degott, Claude (1999). "Focal Nodular Hyperplasia of the Liver". The American Journal of Surgical Pathology. 23 (12): 1441–54. doi:10.1097/00000478-199912000-00001. PMID 10584697.
- ↑ Imaging in Focal Nodular Hyperplasia at eMedicine
- ↑ Scalori, Astrid; Tavani, Alessandra; Gallus, Silvano; La Vecchia, Carlo; Colombo, Massimo (2002). "Oral contraceptives and the risk of focal nodular hyperplasia of the liver: A case-control study". American Journal of Obstetrics and Gynecology. 186 (2): 195–7. doi:10.1067/mob.2002.120277. PMID 11854634.
- ↑ Dioguardi Burgio, Marco; Ronot, Maxime; Salvaggio, Giuseppe; Vilgrain, Valérie; Brancatelli, Giuseppe (December 2016). "Imaging of Hepatic Focal Nodular Hyperplasia: Pictorial Review and Diagnostic Strategy". Seminars in Ultrasound, CT and MRI. 37 (6): 511–524. doi:10.1053/j.sult.2016.08.001. PMID 27986170. Archived from the original on 2022-02-24. Retrieved 2022-03-08.
- ↑ Hamad, Sammy; Willyard, Charles E.; Mukherjee, Sandeep (2022). "Focal Nodular Hyperplasia". StatPearls. StatPearls Publishing. Retrieved 28 September 2022.
- ↑ Table 37.2 in: Sternberg, Stephen (2012). Sternberg's diagnostic surgical pathology. Place of publication not identified: LWW. ISBN 978-1-4511-5289-0. OCLC 953861627.
- 1 2 Myers, L; Ahn, J (August 2020). "Focal Nodular Hyperplasia and Hepatic Adenoma: Evaluation and Management". Clinics in Liver Disease. 24 (3): 389–403. doi:10.1016/j.cld.2020.04.013. PMID 32620279. S2CID 220335859.
References
- Chun Hsee, Li; McCall, John L.; Koea, Jonathan B. (2005). "Focal nodular hyperplasia: what are the indications for resection?". HPB. 7 (4): 298–302. doi:10.1080/13651820500273624. PMC 2043107. PMID 18333211.
External links
| Classification | |
|---|---|
| External resources |