Fibrolamellar hepatocellular carcinoma
| Fibrolamellar hepatocellular carcinoma | |
|---|---|
| Other names: FHCC | |
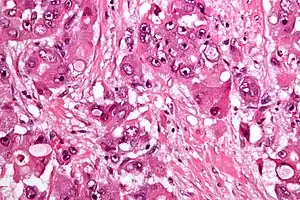 | |
| Micrograph of fibrolamellar hepatocarcinoma showing the characteristic laminated fibrosis between the tumor cells with a low NC ratio. H&E stain. | |
Fibrolamellar hepatocellular carcinoma (FHCC) is a rare form of hepatocellular carcinoma (HCC) that typically affects young adults and is characterized, under the microscope, by laminated fibrous layers interspersed between the tumour cells. Approximately 200 new cases are diagnosed worldwide each year.[1]
Signs and symptoms
The clinical presentation of Fibromellar hepatocellular carcinoma is consistent with:[2]
- Abdominal pain
- Nausea
- Malaise
Cause
A recent study showed the presence of the DNAJB1-PRKACA chimeric transcript (resulting from a 400kb somatic deletion on chromosome 19) in 100% of the FHCCs examined (15/15)[3] This gene fusion has been confirmed in a second study.[4]
Pathology
The histopathology of FHCC is characterized by laminated fibrous layers, interspersed between the tumor cells. Cytologically, the tumor cells have a low nuclear to cytoplasmic ratio with abundant eosinophilic cytoplasm. Tumors are non-encapsulated, but well circumscribed, when compared to conventional HCC (which typically has an invasive border).
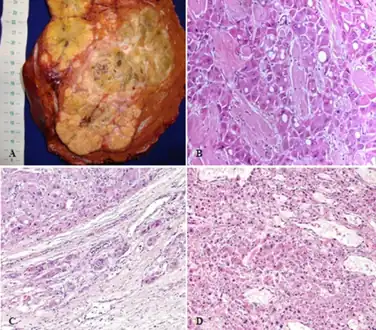 a-d)Pathological aspects of fibrolamellar hepatocellular carcinoma
a-d)Pathological aspects of fibrolamellar hepatocellular carcinoma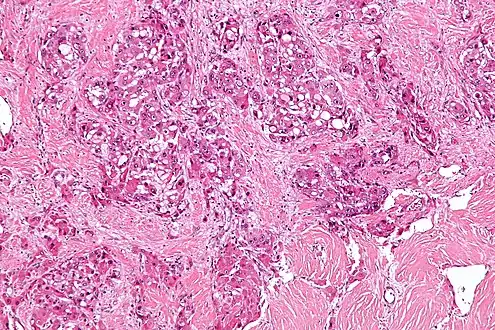 Intermed. mag.Fibrolamellar hepatocellular carcinoma
Intermed. mag.Fibrolamellar hepatocellular carcinoma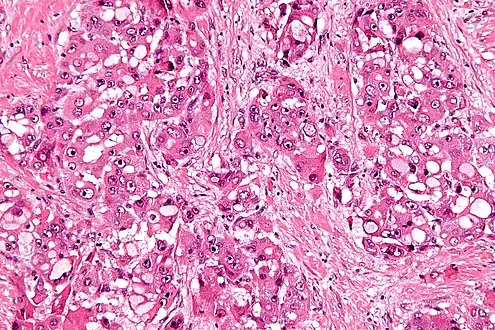 High mag.Fibrolamellar hepatocellular carcinoma
High mag.Fibrolamellar hepatocellular carcinoma
Diagnosis
Due to lack of symptoms, until the tumor is sizable, this form of cancer is often advanced when diagnosed. Symptoms include vague abdominal pain, nausea, abdominal fullness, malaise and weight loss. They may also include a palpable liver mass.[5] Other presentations include jaundice, ascites, fulminant liver failure, encephalopathy, gynecomastia (males only), thrombophlebitis of the lower limbs, recurrent deep vein thrombosis, anemia and hypoglycemia.
The usual markers for liver disease – aspartate aminotransferase, alanine aminotransferase and alkaline phosphatase – are often normal or only slightly elevated. FHCC often does not produce alpha fetoprotein (AFP), a widely used marker for conventional hepatocellular carcinoma. It is associated with elevated neurotensin levels.
Diagnosis is normally made by imaging (ultrasound, CT or MRI) and biopsy
Treatment
In FHCC, plasma neurotensin and serum vitamin B12 binding globulin are commonly increased and are useful in monitoring the disease and detecting recurrence.
FHCC can often be surgically removed. Liver resection is the optimal treatment and may need to be performed more than once, since this disease has a very high recurrence rate. Due to such recurrence, periodic follow-up medical imaging (CT or MRI) is necessary.
As the tumor is quite rare, there is no standard chemotherapy regimen. Radiotherapy has been used but data is limited concerning its use. The survival rate for fibrolamellar HCC largely depends on whether (and to what degree) the cancer has metastasized, i.e. spread to the lymph nodes or other organs. Distant spread (metastases), significantly reduces the median survival rate. Five-year survival rates vary between 40–90%.
Epidemiology
FHCC accounts for 1–10% of primary liver cancers.[6] It typically has a young age at presentation (20–40 years: mean age ~27 years[7]) when compared to conventional HCC. Unlike the more common HCC, patients most often do not have coexistent liver disease such as cirrhosis.
History
This disease was first described by Hugh Edmondson in a 14-year-old female with no underlying liver disease.[8] The name fibrolamellar hepatocellular carcinoma was coined by Craig et al. in 1980.[9] It was not recognised as a distinct form of cancer by the WHO until 2010.[10]
References
- ↑ "Teen Makes Genetic Discovery of Her Own Rare Cancer". Archived from the original on 2019-05-03. Retrieved 2022-03-13.
- ↑ Abdelhamed, Walaa; El-Kassas, Mohamed (15 June 2022). "Fibrolamellar hepatocellular carcinoma: A rare but unpleasant event". World Journal of Gastrointestinal Oncology. 14 (6): 1103–1114. doi:10.4251/wjgo.v14.i6.1103. ISSN 1948-5204. Archived from the original on 29 September 2022. Retrieved 29 September 2022.
- ↑ Honeyman JN, Simon EP, Robine N, Chiaroni-Clarke R, Darcy DG, Lim II, Gleason CE, Murphy JM, Rosenberg BR, Teegan L, Takacs CN, Botero S, Belote R, Germer S, Emde AK, Vacic V, Bhanot U, LaQuaglia MP, Simon SM (28 February 2014). "Detection of a Recurrent DNAJB1-PRKACA Chimeric Transcript in Fibrolamellar Hepatocellular Carcinoma". Science. 343 (6174): 1010–4. Bibcode:2014Sci...343.1010H. doi:10.1126/science.1249484. PMC 4286414. PMID 24578576.
- ↑ Dinh TA, Vitucci EC, Wauthier E, Graham RP, Pitman WA, Oikawa T, Chen M, Silva G, Greene KG, Torbenson MS, Reid LM, Sethupathy P (2017) Comprehensive analysis of The Cancer Genome Atlas reveals a unique gene and non-coding RNA signature of fibrolamellar carcinoma. Sci Rep 7:44653. doi: 10.1038/srep44653
- ↑ Yen, JB.; Chang, KW. (2009). "Fibrolamellar hepatocellular carcinoma- report of a case". Chang Gung Med J. 32 (3): 336–9. PMID 19527614.
- ↑ Lafaro KJ, Pawlik TM (2015) Fibrolamellar hepatocellular carcinoma: current clinical perspectives. J Hepatocell Carcinoma 2:151–157 doi: 10.2147/JHC.S75153
- ↑ Stipa F, Yoon SS, Liau KH, et al. (March 2006). "Outcome of patients with fibrolamellar hepatocellular carcinoma". Cancer. 106 (6): 1331–8. doi:10.1002/cncr.21703. PMID 16475212.
- ↑ Edmondson HA (1956) Differential diagnosis of tumors and tumor-like lesions of liver in infancy and childhood. AMA J Dis Child 91(2):168–186
- ↑ Craig JR, Peters RL, Edmondson HA, Omata M. Fibrolamellar carcinoma of the liver: a tumor of adolescents and young adults with distinctive clinico-pathologic features. Cancer 46(2):372–379
- ↑ Bosman FT (2010) World Health Organization. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: International Agency for Research on Cancer
External links
| Classification | |
|---|---|
| External resources |