Hydrocele
| Hydrocele | |
|---|---|
| Other names: Hydrocoele, hydrocele testis | |
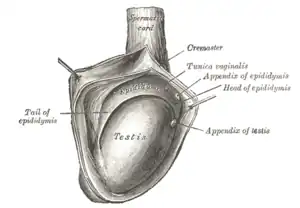 | |
| The right testis, exposed by laying open the tunica vaginalis. (Tunica vaginalis is labeled at upper right.) | |
| Specialty | Urology |
| Symptoms | Painless fluid filled sac within the scrotum[1] |
| Complications | Infection, bleeding, infertility[2] |
| Types | Communicating, noncommunicating[3] |
| Causes | Children: Failure of closure of the processus vaginalis[2] Adults: Filariasis, injury, following hernia surgery[2] |
| Diagnostic method | Examination, ultrasound[3] |
| Differential diagnosis | Groin hernia, testicular tumor, epididymitis, spermatocele, varicocele[2] |
| Treatment | Observation, surgery[2] |
| Frequency | Common[4] |
A hydrocele is a collection of fluid, most commonly around the testicle.[5] It generally presents as painless swelling of the scrotum.[3][2] Usually only one side is affected.[1] Complications may include infection, bleeding, or infertility.[2] In females a hydrocele may form in the labia majora.[4]
The most common cause in children is a failure of the processus vaginalis to close.[2] In adults the most common causes include filariasis, injury, and following hernia surgery.[2] The underlying mechanism involves fluid collecting within the tunica vaginalis.[2] Diagnosis is usually by examination and ultrasound.[3]
Cases in newborns typically resolve on their own in the first year or two of life.[2] In those who develop symptoms, surgery is the primary treatment.[2] While it can be aspirated, the fluid generally simply recollects.[2] In newborns, outcomes are generally excellent; while in adulthood outcomes depend on the underlying cause.[2]
Hydroceles are common globally, particularly in low and middle income countries.[4] Around 2 to 5% of males may be affected in the first year of life.[6] Males are more commonly affected than females.[6] It is believed that the condition is underreported due to modesty.[4]
Signs and symptoms
_(14597676008).jpg.webp)
A hydrocele feels like a small fluid-filled balloon inside the scrotum. It is smooth, and is mainly in front of the testis. Hydroceles vary greatly in size and are typically painless and harmless. However, as the fluid continues to accumulate and the scrotum further enlarges, more discomfort can be expected. Large hydroceles will cause discomfort because of their size. Sometimes pain can be in both testicles as pressure from the enlarged area puts pressure against the unaffected area which can cause discomfort to the normal testicle. It has also been found to decrease a man's sex drive and makes him less active for fear of enlarging the mass. As the fluid of a hydrocele is transparent, light shone through the hydrocelic region will be visible from the other side. This phenomenon is called transillumination.
Symptoms of a hydrocele can easily be distinguished from testicular cancer, as a hydrocele is soft and fluid-filled, whereas testicular cancer feels hard and rough.
Complications
Among the complications of hydrocele are:
- Rupture usually occurs as a result of trauma but may be spontaneous. On rare occasions cure results after the fluid has been absorbed.
- Transformation into a haematocele occurs if there is spontaneous bleeding into the sac or as a result of trauma. Acute haemorrhage into the tunica vaginalis sometimes results from testicular trauma and it may be difficult without exploration to decide whether the testis has been ruptured. If the haematocele is not drained, a clotted haematocele usually results.
- The sac may calcify. Clotted hydrocele may result from a slow spontaneous ooze of blood into the tunica vaginalis. It is usually painless and by the time the patient seeks help, it may be difficult to be sure that the swelling is not due to a testicular tumour. Indeed, a tumour may present as a haematocele.
- Occasionally, infection can be introduced by aspiration. Simple aspiration, however, often may be used as a temporary measure in those cases where surgery is contraindicated or must be postponed.
- Postherniorrhaphy hydrocele is a relatively rare complication of inguinal hernia repair. It is possibly due to interruption to the lymphatics draining the scrotal contents.
- Infection which may lead to pyocele.
- Atrophy of testis in long standing cases.
A hydrocele testis is not generally thought to affect fertility. However, it may be indicative of other factors that may affect fertility.
Complications are often diagnosed post-operatively, which can be differentiated through duplex ultrasound scanning and are bit observed until 24 to 48 hours for early complications such as drainage, infection, formation of haematocele, rupture, etc., but also for 1 to 6 weeks during follow-up on out-patient basis.
Cause
A hydrocele can be produced in four ways:
- by excessive production of fluid within the sac, e.g. secondary hydrocele
- through defective absorption of fluid
- by interference with lymphatic drainage of scrotal structures as in case of elephantiasis
- by connection with a hernia of the peritoneal cavity in the congenital variety, which presents as hydrocele of the cord
Primary hydroceles may develop in adulthood, particularly in the elderly and in hot countries, by slow accumulation of serous fluid. This is presumably caused by impaired reabsorption. A hydrocele can also result from plugged inguinal lymphatic system caused by chronic infection by Wuchereria bancrofti or Brugia malayi, two mosquito-borne parasites found in Africa and Southeast Asia, respectively.
Primary
The swelling is soft and non-tender, large in size on examination, and the testis cannot usually be felt. The presence of fluid is demonstrated by transillumination. These hydroceles can reach a huge size, containing large amount of fluid, as these are painless and are often ignored. They are otherwise asymptomatic, other than size and weight, causing inconvenience. However the long continued presence of large hydroceles causes atrophy of testis due to compression or by obstructing blood supply. In most cases, the hydrocele, when diagnosed early during complete physical examination, are small and the testis can easily be palpated within a lax hydrocele. However Ultrasound imaging is necessary to visualize the testis if the hydrocele sac is dense to reveal the primary abnormality. But these can become large in cases when left unattended. Hydroceles are usually painless, as are testicular tumors.
Infantile
It does not occur only in infants but it occurs in adults also, a hydrocele is usually an expression of a patent processus vaginalis (PPV). The tunica and the processus vaginalis are distended to the inguinal ring but there is no connection with the peritoneal cavity.
Congenital
The processus vaginalis is patent and connects with the general peritoneal cavity. The communication is usually too small to allow herniation of intra-abdominal contents. Digital pressure on the hydrocele does not usually empty it, but the hydrocele fluid may drain into the peritoneal cavity when the child is lying down. Ascites or even ascitic tuberculous peritonitis should be considered if the swellings are bilateral.
Encysted cord
There is a smooth oval swelling near the spermatic cord which is liable to be mistaken for an inguinal hernia. The swelling moves downwards and becomes less mobile if the testis is pulled gently downwards. Rarely, a hydrocele develops in a remnant of the processus vaginalis somewhere along the course of the spermatic cord. This hydrocele also transilluminates, and is known as an encysted hydrocele of the cord. In females, a related region in females, a multicystic hydrocele of the canal of Nuck[7] sometimes presents as a swelling in the groin. It probably results from cystic degeneration of the round ligament. Unlike a hydrocele of the cord, a hydrocele of the canal of Nuck is always at least partially within the inguinal canal.
The accuracy of the diagnosis must be ascertained. Great care must be taken to differentiate a hydrocele from a scrotal hernia or tumor of the testicle. Ultrasound imaging can be very useful in these cases. A hernia usually can be reduced, transmits a cough impulse, and is not translucent. A hydrocele cannot be reduced into the inguinal canal and gives no impulse on coughing unless a hernia is also present. In young children a hydrocele is often associated with a complete congenital type of hernial sac.
Secondary
This usually occurs as a result of an underlying condition, such as infection (filariasis, tuberculosis of the epididymis, syphilis), injury (trauma, post-herniorrhaphy hydrocele), or cancer.[2] This type of hydrocele tends to be small, with the exception of secondary hydrocele due to filariasis, which can be very large.[2]
Pathophysiology
During embryogenesis, the testis descends through the inguinal canal, drawing a diverticulum of peritoneum into the scrotum as it descends. This peritoneal tissue is known as the processus vaginalis. Normally, the communication between the processus vaginalis and the peritoneum is obliterated, and the tunica vaginalis is the tissue that remains overlying the testis and the epididymis. Congenital hydrocele results when the processus vaginalis remains, allowing fluid from the peritoneum to accumulate in the scrotum.
Diagnosis
A primary hydrocele is described as having the following characteristics:
- Transillumination positive
- Fluctuation positive
- Impulse on coughing negative (positive in congenital hydrocele)
- Reducibility absent
- Testis cannot be palpated separately. (exception - funicular hydrocele, encysted hydrocele)
A common method of diagnosing is by attempting to shine a strong light (transillumination) through the enlarged scrotum. A hydrocele will usually pass light, while a tumor will not (except in the case of a malignancy with reactive hydrocele).
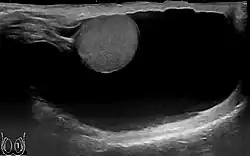 Scrotal ultrasound of a 10 cm large hydrocele, with anechoic (dark) fluid surrounding the testicle.
Scrotal ultrasound of a 10 cm large hydrocele, with anechoic (dark) fluid surrounding the testicle. Communicating hydrocele, caused by the failure of the processus vaginalis closure.
Communicating hydrocele, caused by the failure of the processus vaginalis closure.
Treatment
Most hydroceles appearing in the first year of life seldom require treatment as they resolve without treatment.[8] Hydroceles that persist after the first year or occur later in life require treatment only in selected cases, such as patients who are symptomatic with pain or a pressure sensation, or when the scrotal skin integrity is compromised from chronic irritation; the treatment of choice is surgery and the operation is conducted via an open access technique aiming to excise the hydrocele sac.[9][10] Anesthesia is required for the operation and general anesthesia is of choice in children, while spinal anesthesia is usually sufficient in adults. Local infiltration anesthesi] is not satisfactory because it cannot abolish abdominal pain due to traction on the spermatic cord.[11] In long standing cases, hydrocele fluid may be opalescent with cholesterol and may contain crystals of tyrosine.[12]
After aspiration of a primary hydrocele, fluid reaccumulates over the following months and periodic aspiration or operation is needed. For younger patients, operation is usually preferred. Sclerotherapy is an alternative; after aspiration, 6% aqueous phenol (10-20 ml) together with 1% lidocaine for analgesia can be injected, and this often inhibits reaccumulation. These alternative treatments are generally regarded as unsatisfactory treatment because of the high incidence of recurrences and the frequent necessity for repetition of the procedure.
Surgery
A more permanent alternative is a surgical procedure, generally, an outpatient ambulatory (same-day) procedure, called a hydrocelectomy. There are two surgical techniques available for hydrocelectomy.
Hydrocelectomy with excision of the hydrocele sac: Incision of the hydrocele sac after complete mobilization of the hydrocele. Partial resection of the hydrocele sac, leaving a margin of 1–2 cm. Care is taken not to injure testicular vessels, epididymis or ductus deferens. The edge of the hydrocele sac is oversewn for hemostasis (von Bergmann's technique) or the edges are sewn together behind the spermatic cord (Winkelmann's or Jaboulay's technique). Hydrocele surgery with excision of the hydrocele sac is useful for large or thick-walled hydroceles and multilocular hydroceles.
Hydrocele surgery with plication of the hydrocele sac: The hydrocele is opened with a small skin incision without further preparation. The hydrocele sac is reduced (plicated) by suture Hydrocele surgery: Lord's technique. The plication technique is suitable for medium-sized and thin-walled hydroceles. The advantage of the plication technique is the minimized dissection with a reduced complication rate.[13]
If the hydrocele is not surgically removed, it may continue to grow. The hydrocele fluid can be aspirated. This procedure can be done in a urologist's office or clinic and is less invasive, but recurrence rates are high.[14] Sclerotherapy, the injection of a solution following aspiration of the hydrocele fluid may increase success rates.[15] In many patients, the procedure of aspiration and sclerotherapy is repeated as the hydrocele recurs.[16]
References
- 1 2 "Hydrocele in Adults | Fluid in the Scrotum | Tests & Treatment". patient.info. Archived from the original on 24 March 2022. Retrieved 15 May 2022.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Huzaifa, M; Moreno, MA (January 2022). "Hydrocele". PMID 32644551.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 "Painless Scrotal Mass - Genitourinary Disorders". Merck Manuals Professional Edition. Archived from the original on 25 November 2021. Retrieved 14 May 2022.
- 1 2 3 4 Beard, JH; Ohene-Yeboah, M; devries, CR; Schecter, WP; Debas, HT; Donkor, P; Gawande, A; Jamison, DT; Kruk, ME; Mock, CN (2 April 2015). "Hernia and Hydrocele". doi:10.1596/978-1-4648-0346-8_ch9. PMID 26741001.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Dorland's Illustrated Medical Dictionary. W B Saunders Co. 2000. p. 839. ISBN 9780721662541.
- 1 2 Cabana, Michael (30 August 2018). 5-Minute Pediatric Consult. Lippincott Williams & Wilkins. p. 1997. ISBN 978-1-9751-2684-1.
- ↑ "hydrocele of the canal of Nuck". GPnotebook.
- ↑ "Hydrocele: Symptoms, causes, and treatment". www.medicalnewstoday.com. 2020-03-24. Archived from the original on 2021-01-24. Retrieved 2020-12-17.
- ↑ Zollinger's Atlas of Surgeries
- ↑ "UpToDate". www.uptodate.com. Archived from the original on 2017-07-20. Retrieved 2020-01-06.
- ↑ Manual of Anesthesia for Out Patient Surgical Procedures
- ↑ Bailey and Love-Short Practice of Surgery
- ↑ Ku u.a. 2001 KU, J. H.; KIM, M. E.; LEE, N. K.; PARK, Y. H.:The excisional, plication and internal drainage techniques: a comparison of the results for idiopathic hydrocele.In: BJU Int 87 (2001), Nr. 1, S. 82–4
- ↑ Fracchia, JA; Armenakas, NA; Kohan, AD (1998). "Cost-effective hydrocele ablation". The Journal of Urology. 159 (3): 864–7. doi:10.1016/S0022-5347(01)63755-8. PMID 9474170.
- ↑ Beiko, DT; Kim, D; Morales, A (2003). "Aspiration and sclerotherapy versus hydrocelectomy for treatment of hydroceles". Urology. 61 (4): 708–12. doi:10.1016/S0090-4295(02)02430-5. PMID 12670550.
- ↑ Shan, CJ; Lucon, AM; Arap, S. (2003). "A Comparative study of sclerotherapy with phenol and surgical treatment for hydrocele". J Urol. 169 (3): 1056–9. doi:10.1097/01.ju.0000052680.03705.40. PMID 12576845.
External links
| Classification | |
|---|---|
| External resources |