Varicocele
| Varicocele | |
|---|---|
 | |
| Varicocele on the person's left testicle. Notice the swelling and slight enlargement of the left testicle, which is marked by an arrow. | |
| Pronunciation | |
| Specialty | Urology |
| Symptoms | Enlargement, testicular pain[3] |
| Complications | Infertility[3] |
| Usual onset | Puberty[3] |
| Types | Grade 1 (small) to 3 (large)[3][4] |
| Risk factors | Family history, smoking[3][4] |
| Diagnostic method | Based on examination, ultrasound[3] |
| Differential diagnosis | Epididymitis, hydrocele, inguinal hernia, testicular tumor, spermatocele[4] |
| Treatment | None, surgery, embolization[3] |
| Frequency | 20%[3] |
A varicocele is an abnormal enlargement of the veins from a testicle.[3] It may result in one testicle appearing larger than the other and occasionally testicular pain.[3][4] The left side is more commonly affected, though both may be involved.[3][4] Complications may include infertility.[3]
The cause is usually unknown.[4] They run in families and occur more often in smokers.[3][4] The veins that drain the testicle play an important role in temperature regulation.[3] When they malfunction the testicle may overheat which may decrease sperm quality and testosterone levels.[3] Diagnosis is based on examination, and may be confirmed by ultrasound.[3] The may be classified as small, medium, and large.[4]
In mild cases no specific treatment is required.[3] In those with significant symptoms surgery or embolization may be an option.[3] Treatment improves pain about 80% of the time and fertility about 70% of the time.[3] A varicocele occurs in around 20% of all men; but 40% of those with infertility.[3][4] They often form during puberty and get larger with age.[3]
Signs and symptoms
Varicocele might be noticed as soft lumps, usually above the testicle and mostly on the left side of the scrotum.[5] Right-sided and bilateral varicocele does also occur. Men with varicocele can feel symptoms of pain or heaviness in their scrotum.[5] Large varicoceles present as plexus of veins and may be described as "bag of worms".[6][7] Varicocele is sometimes discovered when investigating the cause of male infertility.[8][9]
Cause
There are three main theories as to the anatomical cause; the first has to do with the geometry of the veins, wherein the vein on the left side connects to the larger outflowing vein at a right angle, which tends to fail; the second is that valves that are supposed to prevent backflow fail (venous insufficiency); the third is due to excessive pressure in upstream arteries, created by nutcracker syndrome.[10]
Pathophysiology

Often the greatest concern with respect to varicocele is its effect on male fertility. The relationship between varicocele and infertility is unclear. Some men with the condition are fertile, some have sperm that are normal in shape and move normally but are compromised in function, and some have sperm with abnormal shapes or that do not move well.[10] Theories as to how varicocele affects sperm function include damage via excess heat caused by the blood pooling and oxidative stress on sperm.[11][10][12][13]
Tobacco smoking and mutations in the gene expressing glutathione S-transferase Mu 1 both put men at risk for infertility; these factors may also exacerbate the risk that varicocele will affect fertility.[10]
Diagnosis
Following discovery of the sign of swelling comprising a mass, varicocele can be confirmed with scrotal ultrasound, which will show dilation of the vessels of the pampiniform plexus to be greater than 2 mm.[14]
 Varicocele in ultrasound (left: testicle)
Varicocele in ultrasound (left: testicle)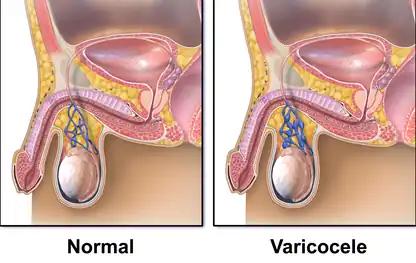 Varicocele
Varicocele
Treatment

The two most common surgical approaches are retroperitoneal (abdominal using laparoscopic surgery), infrainguinal/subinguinal (below the groin) and inguinal (groin using percutaneous embolization).[11] Possible complications of this procedure include hematoma (bleeding into tissues), hydrocele (accumulation of fluid around the affected testicle), infection, or injury to the scrotal tissue or structures. In addition, injury to the artery that supplies the testicle may occur, resulting in a loss of a testicle.[11]
Prognosis
Whether having varicocele surgery or embolization improves male fertility is controversial, as good clinical data is lacking.[9] There is tentative evidence that varicocelectomy may improve fertility in those with obvious findings and abnormal sperm;[11] however, this has a number needed to treat of 7 for varicocelectomy and 17 for embolization.[15][16] There are also studies showing that the regular surgery has no significant effect on infertility.[9] A 2012 Cochrane review (updated in 2021) found tentative but unclear evidence of improved fertility among males treated for varicocele.[17] Evidence for sclerotherapy is unclear as of 2015.[18]
Epidemiology
Around 15% to 20% of all adult males, up to 35% to 40% of men who are evaluated for male infertility, and around 80% of men who are infertile due to some other cause, have varicocele.[19][11][9]
References
- ↑ "Varicocele". Merriam-Webster Dictionary. Retrieved 2016-01-21.
- ↑ "Varicocele". Oxford Dictionaries UK Dictionary. Oxford University Press. Retrieved 2016-01-21.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 Sasson, Daniel C.; Kashanian, James A. (2 June 2020). "Varicoceles". JAMA. 323 (21): 2210–2210. doi:10.1001/jama.2020.0397. ISSN 0098-7484. Archived from the original on 2 July 2020. Retrieved 13 February 2022.
- 1 2 3 4 5 6 7 8 9 Leslie, Stephen W.; Sajjad, Hussain; Siref, Larry E. (2022). "Varicocele". StatPearls. StatPearls Publishing. Archived from the original on 29 November 2020. Retrieved 13 February 2022.
- 1 2 "Testicular lumps and swellings - Causes - NHS Choices". NHS Choices. 7 October 2014. Archived from the original on 24 August 2017. Retrieved 10 January 2022.
- ↑ Cannarella, Rossella; Calogero, Aldo E.; Condorelli, Rosita A.; Giacone, Filippo; Aversa, Antonio; La Vignera, Sandro (8 September 2019). "Management and Treatment of Varicocele in Children and Adolescents: An Endocrinologic Perspective". Journal of Clinical Medicine. 9 (8): 1410. doi:10.3390/jcm8091410. PMC 6780349. PMID 31500355.
- ↑ Leslie, Stephen W.; Sajjad, Hussain; Siref, Larry E. (7 October 2019). Varicocele. StatPearls [Internet]. Archived from the original on 29 November 2020. Retrieved 20 January 2020.
- ↑ "Low sperm count". NHS Choices. 2 August 2016. Archived from the original on 14 September 2017. Retrieved 10 January 2022.
- 1 2 3 4 Baazeem, Abdulaziz; Belzile, Eric; Ciampi, Antonio; Dohle, Gert; Jarvi, Keith; Salonia, Andrea; Weidner, Wolfgang; Zini, Armand (2011-10-01). "Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair". European Urology. 60 (4): 796–808. doi:10.1016/j.eururo.2011.06.018. PMID 21733620.
- 1 2 3 4 Eisenberg, Michael L.; Lipshultz, Larry I. (2011-01-01). "Varicocele-induced infertility: Newer insights into its pathophysiology". Indian Journal of Urology. 27 (1): 58–64. doi:10.4103/0970-1591.78428. ISSN 0970-1591. PMC 3114589. PMID 21716891.
- 1 2 3 4 5 Kupis, Ł; Dobroński, PA; Radziszewski, P (2015). "Varicocele as a source of male infertility - current treatment techniques". Central European Journal of Urology. 68 (3): 365–70. doi:10.5173/ceju.2015.642. PMC 4643713. PMID 26568883.
- ↑ Hayden, Russell P.; Tanrikut, Cigdem (2016-05-01). "Testosterone and Varicocele". The Urologic Clinics of North America. 43 (2): 223–232. doi:10.1016/j.ucl.2016.01.009. ISSN 1558-318X. PMID 27132580.
- ↑ Dabaja, Ali; Wosnitzer, Matthew; Goldstein, Marc (2013-08-01). "Varicocele and hypogonadism". Current Urology Reports. 14 (4): 309–314. doi:10.1007/s11934-013-0339-4. ISSN 1534-6285. PMID 23754533. S2CID 5477034.
- ↑ Salam, MA (2013). Principles and Practice of Urology. New Delhi 110 002, India: Jaypee Brothers Medical Publishers. p. 752. ISBN 978-93-5025-260-4. Archived from the original on 2022-02-13. Retrieved 2022-01-10.
{{cite book}}: CS1 maint: location (link) - ↑ Kroese, A. C. J.; Lange, N. M. de; Collins, J. A.; Evers, J. L. H. (2013-07-01). "Varicocele surgery, new evidence". Human Reproduction Update. 19 (4): 317. doi:10.1093/humupd/dmt004. PMID 23515200.
- ↑ Li, Fuping; Yue, Huanxun; Yamaguchi, Kohei; Okada, Keisuke; Matsushita, Kei; Ando, Makoto; Chiba, Koji; Fujisawa, Masato (2012). "Effect of surgical repair on testosterone production in infertile men with varicocele: A meta-analysis". International Journal of Urology. 19 (2): 149–54. doi:10.1111/j.1442-2042.2011.02890.x. PMID 22059526. S2CID 20329833.
- ↑ Persad, Emma; O'Loughlin, Clare Aa; Kaur, Simi; Wagner, Gernot; Matyas, Nina; Hassler-Di Fratta, Melanie Rosalia; Nussbaumer-Streit, Barbara (2021-04-23). "Surgical or radiological treatment for varicoceles in subfertile men". The Cochrane Database of Systematic Reviews. 4: CD000479. doi:10.1002/14651858.CD000479.pub6. ISSN 1469-493X. PMC 8408310. PMID 33890288. Archived from the original on 2021-12-16. Retrieved 2022-01-10.
- ↑ Macleod, R; Biyani, CS; Cartledge, J; Eardley, I (13 July 2015). "Varicocele". BMJ Clinical Evidence. 2015. PMC 4500994. PMID 26168774.
- ↑ White, Wesley M.; Kim, Edward David; Mobley, Joe D (2 January 2019). "Varicocele: Epidemiology". Medscape. Archived from the original on 24 July 2019. Retrieved 18 September 2019.
Although varicoceles appear in approximately 20% of the general male population, they are much more common in the subfertile population (40%).
External links
| Classification | |
|---|---|
| External resources |