Hypertensive emergency
| Hypertensive emergency | |
|---|---|
 | |
| CT scan of an intracranial hemorrhage, a possible complication of hypertensive emergency. | |
| Specialty | Cardiology |
| Complications | Stroke, hypertensive encephalopathy, acute aortic syndrome, retina disease, kidney problems, heart failure, pulmonary edema, preeclampsia[1] |
| Types | Malignant hypertension (accelerated hypertension), hypertensive encephalopathy, thrombotic microangiopathy[2][3] |
| Risk factors | Not taking BP medication, high salt diet, NSAIDs, stimulants, kidney artery stenosis, phaeochromocytoma, Cushing’s syndrome[2][3] |
| Diagnostic method | Based on blood pressure and symptoms; supported by testing[1] |
| Differential diagnosis | Hypertensive urgency[4] |
| Treatment | Intravenous blood pressure medication[1] |
| Frequency | 0.3% of emergency patients[3] |
| Deaths | 4% risk of death[1] |
Hypertensive emergency is very high blood pressure, generally a systolic above 180 mmHg, which is resulting in organ damage.[4][5] This may include stroke, hypertensive encephalopathy, acute aortic syndrome, acute coronary syndrome, retina disease, kidney problems, heart failure, pulmonary edema, or preeclampsia.[1]
Triggers may include not taking blood pressure medication, a high salt diet, NSAIDs, stimulants, kidney artery stenosis, phaeochromocytoma, or Cushing’s syndrome.[2][3] Diagnosis is based on blood pressure together with symptoms; supported by urine tests, blood tests, and an ECG.[1][4] There are no specific cutoff values for blood pressure.[2] Medical imaging may be carried out based on the symptoms.[4] It differs from hypertensive urgency, where organ damage is lacking.[4]
Initial treatment is with blood pressure medication given by injection into a vein.[1] Labetalol is a commonly used.[1] Other options may include nicardipine, esmolol, or nitroglycerin.[3][4] Over one to two hours, the goal is generally to reduce blood pressure by about 20%.[4] Care is in an intensive care unit.[1] Further measures may be directed at the specific complication.[1]
Hypertensive emergency is present in about 0.3% of people who present to the emergency department.[3] Age of onset is often in peoples 50s or 60s.[6] Risk of death is about 4%.[1] The condition was first described in 1914 by Volhard and Fahr.[7]
Signs and symptoms

Symptoms may include headache, nausea, or vomiting. Chest pain may occur due to increased workload on the heart resulting in inadequate delivery of oxygen to meet the heart muscle's metabolic needs. The kidneys may be affected, resulting in blood or protein in the urine, and acute kidney failure. People can have decreased urine production, fluid retention, and confusion.
Other symptoms can include:
- Chest pain
- Abnormal heart rhythms
- Headache
- Nosebleeds that are difficult to stop
- Dyspnea
- Fainting or the sensation of the world spinning around them (vertigo)
- Severe anxiety
- Agitation
- Altered mental status
- Abnormal sensations
The most common presentations of hypertensive emergencies are cerebral infarction (25%), pulmonary edema (23%), hypertensive encephalopathy (16%), and heart failure (12%).[8] Less common include intracranial bleeding, aortic dissection, and pre-eclampsia or eclampsia.[9]
The eyes may show hypertensive retinopathy with bleeding in the retina, an exudate, cotton-wool spots, scattered splinter hemorrhages, or swelling of the optic disc called papilledema.
Causes
Many factors and contribute to a hypertensive emergency. The most common is people with chronic hypertension who have discontinued their blood pressure medications.[10]
Other causes include pheochromocytoma, collagen-vascular diseases, drug use particularly stimulants such as cocaine and amphetamines, monoamine oxidase inhibitors or food-drug interactions, spinal cord disorders, glomerulonephritis, head trauma, neoplasias, preeclampsia and eclampsia, hyperthyroidism and renovascular hypertension.[11][10] People withdrawing from medications such as clonidine or beta-blockers have been frequently found to develop hypertensive crises.[12] It is important to note that these conditions exist outside of hypertensive emergency, in that patients diagnosed with these conditions are at increased risk of hypertensive emergencies or end organ failure.
Pathophysiology
The pathophysiology of hypertensive emergency is not well understood. Failure of normal autoregulation and an abrupt rise in systemic vascular resistance are typical initial components of the disease process.[9]
Hypertensive emergency pathophysiology includes:
- Abrupt increase in systemic vascular resistance, likely related to humoral vasoconstrictors
- Endothelial injury and dysfunction
- Fibrinoid necrosis of the arterioles
- Deposition of platelets and fibrin
- Breakdown of normal autoregulatory function
The resulting ischemia prompts further release of vasoactive substances including prostaglandins, free radicals, and thrombotic/mitotic growth factors, completing a vicious cycle of inflammatory changes.[9] If the process is not stopped, homeostatic failure begins, leading to loss of cerebral and local autoregulation, organ system ischemia and dysfunction, and myocardial infarction. Single-organ involvement is found in approximately 83% of hypertensive emergency patients, two-organ involvement in about 14% of patients, and multi-organ failure (failure of at least 3 organ systems) in about 3% of patients.
In the brain, hypertensive encephalopathy - characterized by hypertension, altered mental status, and swelling of the optic disc - is a manifestation of the dysfunction of cerebral autoregulation. Cerebral autoregulation is the ability of the blood vessels in the brain to maintain a constant blood flow. People with chronic hypertension can tolerate higher arterial pressure before their autoregulation system is disrupted. Hypertensives also have an increased cerebrovascular resistance which puts them at greater risk of developing cerebral ischemia if the blood flow decreases into a normotensive range. On the other hand, sudden or rapid rises in blood pressure may cause hyperperfusion and increased cerebral blood flow, causing increased intracranial pressure and cerebral edema, with increased risk of intracranial bleeding.[11]
In the heart, increased arterial stiffness, increased systolic blood pressure, and widened pulse pressures, all resulting from chronic hypertension, can cause significant damage. Coronary perfusion pressures are decreased by these factors, which also increase myocardial oxygen consumption, possibly leading to left ventricular hypertrophy. As the left ventricle becomes unable to compensate for an acute rise in systemic vascular resistance, left ventricular failure and pulmonary edema or myocardial ischemia may occur.[9]
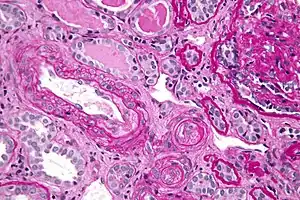
In the kidneys, chronic hypertension has a great impact on the kidney vasculature, leading to pathologic changes in the small arteries of the kidney. Affected arteries develop endothelial dysfunction and impairment of normal vasodilation, which alter kidney autoregulation. When the kidneys' autoregulatory system is disrupted, the intraglomerular pressure starts to vary directly with the systemic arterial pressure, thus offering no protection to the kidney during blood pressure fluctuations. The renin-aldosterone-angiotensin system can be activated, leading to further vasoconstriction and damage. During a hypertensive crisis, this can lead to acute kidney ischemia, with hypoperfusion, involvement of other organs, and subsequent dysfunction. After an acute event, this endothelial dysfunction has persisted for years.[9]
Diagnosis
The term hypertensive emergency is primarily used as a specific term for a hypertensive crisis with a diastolic blood pressure greater than or equal to 120 mmHg or systolic blood pressure greater than or equal to 180 mmHg.[13] Hypertensive emergency differs from hypertensive urgency in that, in the former, there is evidence of acute organ damage.[13] Malignant hypertension is very high blood pressure together with significant retinopathy.[2]
Massive, rapid elevations in blood pressure can trigger any of these symptoms, and warrant further work-up. Physical exam would include measurement of blood pressure in both arms. Laboratory tests to be conducted include urine toxicology, blood glucose, a basic metabolic panel evaluating kidney function, or a complete metabolic panel evaluating liver function, EKG, chest x-rays, and pregnancy screening.[11]
In the pregnancy, the definition of hypertensive emergency (likely secondary to pre-eclampsia or eclampsia) is only a blood pressure exceeding 160 mmHg systolic blood pressure or 110 mmHg diastolic blood pressure.[14]
Treatment
| <1 hr | <25% reduction in mean arterial pressure |
| 2-6 hr | Systolic BP = 160 mmHg; diastolic BP = 110 mmHg |
| 1-2 d | Normal BP |
In a hypertensive emergency, treatment should first stabilize the person's airway, breathing, and circulation. People should generally have their blood pressure slowly lowered over a period of minutes to hours with an antihypertensive. Goals include a reduction in the mean arterial pressure by less than or equal to 25% within the first 1 to 8 hours.[3][11] Certain conditions such as hypertensive heart failure, acute coronary syndrome, phaeochromocytoma, and eclampsia may require lowering systolic blood pressure below 140 mmHg more rapidly.[3] In aortic dissection the recommendation is to rapidly lower below 120 mmHg.[3]
Labetolol at an initial dose of 10 to 20 mg intravenous every 10 minutes; followed by an infusion at 5–20 mg/hour is often used.[1][3] Nitroglycerine is particularly useful in those with heart failure.[1]
If blood pressure is lowered aggressively, people are at increased risk of complications including stroke, blindness, or kidney failure.[9] Several classes of anti hypertensive agents are recommended, with the choice depending on the cause of the hypertensive crisis, the severity of the elevation in blood pressure, and the patient's baseline blood pressure prior to a hypertensive emergency. Physicians will attempt to identify a cause of the patient's hypertension, including chest radiograph, serum laboratory studies evaluating kidney function, urinalysis, as that will alter the treatment approach for a more patient-directed regimen.
Parenteral agents are classified into beta-blockers, calcium channel blockers, systemic vasodilators, or other (fenoldopam, phentolamine, clonidine). Medications include labetalol, nicardipine, hydralazine, sodium nitroprusside, esmolol, nifedipine, isradipine, and clonidine. These medications work through a variety of mechanisms. Labetalol is a beta-blocker with mild alpha antagonism, decreasing the ability of catecholamine activity to increase systemic vascular resistance, while also decreasing heart rate and myocardial oxygen demand. Nicardipine, Nifedipine, and Isradipine are calcium channel blockers that work to decrease systemic vascular resistance and subsequently lower blood pressure. Hydralazine and Sodium nitroprusside are systemic vasodilators, thereby reducing afterload, however can be found to have reflex tachycardia, making them likely second or third line choices. Sodium nitroprusside was previously the first-line choice due to its rapid onset, although now it is less commonly used due to side effects, drastic drops in blood pressure, and cyanide toxicity. Sodium nitroprusside is also contraindicated in myocardial infarction, due to coronary steal.[12] The initial goal in hypertensive emergencies is to reduce the pressure by no more than 25% the mean arterial pressure. Excessive reduction in blood pressure can precipitate coronary, cerebral, or kidney ischemia.
Prognosis
Severe hypertension is a serious and potentially life-threatening medical condition. It is estimated that people who do not receive appropriate treatment only live an average of about three years after the event.[14]
The morbidity and mortality of hypertensive emergencies depend on the extent of end-organ dysfunction and the degree to which blood pressure is controlled afterward. With good blood pressure control and medication compliance, the 5-year survival rate of people with hypertensive crises approaches 55%.[15]
The risks of developing a life-threatening disease affecting the heart or brain increase as the blood flow increases. Commonly, ischemic heart attack and stroke are the causes that lead to death in patients with severe hypertension. It is estimated that for every 20 mm Hg systolic or 10 mm Hg diastolic increase in blood pressures above 115/75 mm Hg, the mortality rate for both ischemic heart disease and stroke doubles.
Consequences of hypertensive emergency result after prolonged elevations in blood pressure and associated end-organ dysfunction. Acute end-organ damage may occur, affecting the neurological, cardiovascular, kidney, or other organ systems. Some examples of neurological damage include hypertensive encephalopathy, cerebral infarction, subarachnoid hemorrhage, and intracranial bleeding. Cardiovascular damage can include myocardial ischemia, acute left ventricular dysfunction, pulmonary edema, and aortic dissection. Other end-organ damage can include acute kidney failure, retinopathy, eclampsia, and microangiopathic hemolytic anemia.
Epidemiology
In 2000, it was estimated that 1 billion people worldwide have hypertension, making it the most prevalent condition in the world.[8] Approximately 60 million Americans have chronic hypertension, with 1% of these individuals having an episode of hypertensive urgency. In emergency departments and clinics around the U.S., the prevalence of hypertensive urgency is suspected to be between 3-5%.[12] 25% of hypertensive crises have been found to be hypertensive emergency versus urgency when presenting to the ER.[14]
Risk factors for hypertensive emergency include age, obesity, noncompliance to anti hypertensive medications, female sex, Caucasian race, preexisting diabetes or coronary artery disease, mental illness, and sedentary lifestyle.[8] Several studies have concluded that African Americans have a greater incidence of hypertension and a greater morbidity and mortality from hypertensive disease than non-Hispanic whites, however hypertensive crises have a greater incidence in Caucasians.[16] Although severe hypertension is more common in the elderly, it may occur in children (though very rarely), likely due to metabolic or hormonal dysfunction. In 2014, a systematic review identified women as having slightly higher increased risks of developing hypertensive crises than do men.[8]
With the usage of anti hypertensives, the rates of hypertensive emergencies has declined from 7% to 1% of those with hypertensive urgency.[8] 16% of people presenting with hypertensive emergency have no known history of hypertension.[9]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Rossi, GP; Rossitto, G; Maifredini, C; Barchitta, A; Bettella, A; Cerruti, L; Latella, R; Ruzza, L; Sabini, B; Vigolo, S; Seccia, TM (January 2022). "Modern Management of Hypertensive Emergencies". High blood pressure & cardiovascular prevention : the official journal of the Italian Society of Hypertension. 29 (1): 33–40. doi:10.1007/s40292-021-00487-1. PMID 34813055.
- 1 2 3 4 5 van den Born B (January 2019). "ESC Council on hypertension position document on the management of hypertensive emergencies". European Heart Journal - Cardiovascular Pharmacotherapy. 5 (1): 37–46. doi:10.1093/ehjcvp/pvy032. PMID 30165588.
- 1 2 3 4 5 6 7 8 9 10 11 Jolly, Hannah; Freel, E Marie; Isles, Chris (19 May 2023). "Management of hypertensive emergencies and urgencies: narrative review". Postgraduate Medical Journal. 99 (1169): 119–126. doi:10.1136/postgradmedj-2021-140899.
- 1 2 3 4 5 6 7 "Hypertensive Emergencies - Cardiovascular Disorders". Merck Manuals Professional Edition. Archived from the original on 30 January 2023. Retrieved 20 June 2023.
- ↑ Williams, Bryan; Mancia, Giuseppe; Spiering, Wilko; Agabiti Rosei, Enrico; Azizi, Michel; Burnier, Michel; Clement, Denis; Coca, Antonio; De Simone, Giovanni; Dominiczak, Anna; Kahan, Thomas; Mahfoud, Felix; Redon, Josep; Ruilope, Luis; Zanchetti, Alberto; Kerins, Mary; Kjeldsen, Sverre; Kreutz, Reinhold; Laurent, Stephane; Lip, Gregory Y.H.; McManus, Richard; Narkiewicz, Krzysztof; Ruschitzka, Frank; Schmieder, Roland; Shlyakhto, Evgeny; Tsioufis, Konstantinos; Aboyans, Victor; Desormais, Ileana (December 2018). "2018 Practice Guidelines for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: ESC/ESH Task Force for the Management of Arterial Hypertension". Journal of Hypertension. 36 (12): 2284–2309. doi:10.1097/HJH.0000000000001961.
- ↑ Shah, Silvi; Thakar, Charuhas V. (17 July 2019). Diabetes/Kidney/Heart Disease, An Issue of Cardiology Clinics. Elsevier Health Sciences. p. 275. ISBN 978-0-323-68122-3. Archived from the original on 1 July 2023. Retrieved 21 June 2023.
- ↑ Varon, Joseph; Marik, Paul E (2003). "[No title found]". Critical Care. 7 (5): 374. doi:10.1186/cc2351. PMID 12974970.
- 1 2 3 4 5 Pak KJ, Hu T, Fee C, Wang R, Smith M, Bazzano LA (2014). "Acute hypertension: a systematic review and appraisal of guidelines". The Ochsner Journal. 14 (4): 655–63. PMC 4295743. PMID 25598731.
A summary of recommendations from the selected guidelines is presented in Table 2.
- 1 2 3 4 5 6 7 Cline, David M.; John Ma, O.; Meckler, Garth D.; Tintinalli, Judith E.; Stephan Stapczynski, J.; Yealy, Donald (2015-11-10). Tintinalli's emergency medicine : a comprehensive study guide. Tintinalli, Judith E.,, Stapczynski, J. Stephan,, Ma, O. John,, Yealy, Donald M.,, Meckler, Garth D.,, Cline, David, 1956- (Eighth ed.). New York. ISBN 9780071794763. OCLC 915775025.
- 1 2 Saguner AM, Dür S, Perrig M, Schiemann U, Stuck AE, Bürgi U, Erne P, Schoenenberger AW (July 2010). "Risk factors promoting hypertensive crises: evidence from a longitudinal study". American Journal of Hypertension. 23 (7): 775–80. doi:10.1038/ajh.2010.71. PMID 20395943.
- 1 2 3 4 Larry Jameson, J.; Fauci, Anthony S.; Kasper, Dennis L.; Hauser, Stephen L.; Longo, Dan L.; Loscalzo, Joseph (2018-08-13). Harrison's principles of internal medicine. Jameson, J. Larry,, Kasper, Dennis L.,, Longo, Dan L. (Dan Louis), 1949-, Fauci, Anthony S., 1940-, Hauser, Stephen L.,, Loscalzo, Joseph (20th ed.). New York. ISBN 9781259644030. OCLC 1029074059.
- 1 2 3 Campos CL, Herring CT, Ali AN, Jones DN, Wofford JL, Caine AL, Bloomfield RL, Tillett J, Oles KS (April 2018). "Pharmacologic Treatment of Hypertensive Urgency in the Outpatient Setting: A Systematic Review". Journal of General Internal Medicine. 33 (4): 539–550. doi:10.1007/s11606-017-4277-6. PMC 5880769. PMID 29340938.
- 1 2 Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. (June 2018). "2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Hypertension. 71 (6): e13–e115. doi:10.1161/HYP.0000000000000065. PMID 29133356.
- 1 2 3 Walls, Ron; Hockberger, Robert; Gausche-Hill, Marianne (2017-03-09). Rosen's emergency medicine : concepts and clinical practice. Walls, Ron M.,, Hockberger, Robert S.,, Gausche-Hill, Marianne (Ninth ed.). Philadelphia, PA. ISBN 9780323390163. OCLC 989157341.
- ↑ Thomas L (October 2011). "Managing hypertensive emergencies in the ED". Canadian Family Physician. 57 (10): 1137–97. PMC 3192077. PMID 21998228.
- ↑ Howard J (1965). "Race Differences in Hypertension Mortality Trends: Differential Drug Exposure as a Theory". Systemic Hypertension. Milbank Mem Fund Q. 43 (2): 202–218. doi:10.2307/3349030. JSTOR 3349030. PMID 14283119.
External links
| Classification | |
|---|---|
| External resources |