Aortoiliac occlusive disease
| Aortoiliac occlusive disease | |
|---|---|
| Other names: Leriche's syndrome, aortic thrombosis, aortic occlusion | |
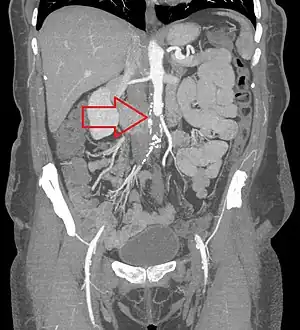 | |
| CT angiogram showing a complete blockage or the aorta (red arrow) with the lower limbs supplied by collaterals | |
| Specialty | Vascular surgery |
| Symptoms | Buttock and thigh pain with exercise, sexual dysfunction, tissue loss[1] |
| Complications | Gangrene, amputation[2] |
| Types | A, B, C, D[1] |
| Causes | Atherosclerosis[2] |
| Risk factors | Diabetes, high blood pressure, high cholesterol, smoking, vasculitis[2] |
| Diagnostic method | Ankle-brachial index < 0.9, CT angiography[1][2] |
| Differential diagnosis | Arterial dissection, giant cell arteritis, venous claudication, neurogenic claudication[2] |
| Treatment | Risk factors, aspirin, clopidogrel, surgery[2] |
| Frequency | Relatively common[3] |
Aortoiliac occlusive disease (AIOD) is the blockage of the abdominal aorta or iliac arteries.[2] Symptoms include buttock and thigh pain with exercise and sexual dysfunction.[1][2] As the disease progresses pain at rest and tissue loss may occur.[1] Complications may include gangrene and amputation.[2]
It generally occurs due to atherosclerosis, with other potential causes including trauma, radiation therapy, and iliac artery endofibrosis.[4] Risk factors include diabetes, high blood pressure, high cholesterol, smoking, and vasculitis.[2] An ankle-brachial index of less than 0.9 supports the diagnosis; which can be confirmed by CT angiography.[1][2] It is a type of peripheral artery disease.[2]
For cases of gradual onsets managing risk factors is important.[2] Either aspirin or clopidogrel is often used.[2] Surgical options may include endovascular or open repair.[1] Cilostazol may be used despite surgery.[2] Up to a third of people have long term complications post surgery.[1]
How commonly it occurs is unclear; though it is relatively common among people with peripheral artery disease.[5][3] It occurs more commonly in males and older people.[2][5] The condition was first described by Robert Graham in 1814.[6][7]
Signs and symptoms
Classically, it is described in male patients as a triad of the following signs and symptoms:
- claudication of the buttocks and thighs
- absent or decreased femoral pulses
- erectile dysfunction
This combination is known as Leriche syndrome. However, any number of symptoms may present, depending on the distribution and severity of the disease, such as muscle atrophy, slow wound healing in the legs, and critical limb ischemia.
Diagnosis
The physical examination usually shows weakened femoral pulses and a reduced ankle-brachial index. The diagnosis can be verified by color duplex scanning, which reveals either a peak systolic velocity ratio ≥2.5 at the site of stenosis and/or a monophasic waveform. MRA and multidetector CTA are often used to determine the extent and type of obstruction. Another technique is digital subtraction angiography which allows verification of the diagnosis and endovascular treatment in a single session.[8]
Angiography provides important information regarding the perfusion and patency of distal arteries (e.g. femoral artery). The presence of collateral arteries in the pelvic and groin area is important in maintaining crucial blood flow and lower limb viability. However, angiography should only be used if symptoms warrant surgical intervention.[8]
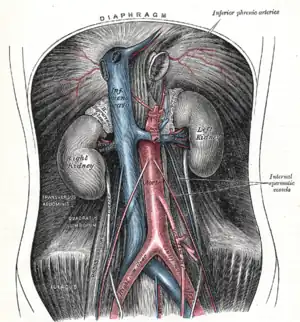 Plate from Gray's Anatomy showing the abdominal aorta and the common iliac arteries.
Plate from Gray's Anatomy showing the abdominal aorta and the common iliac arteries. Fluoroscopic image of an affected aorta
Fluoroscopic image of an affected aorta
Treatment
Treatment involves revascularization typically using either angioplasty or a type of vascular bypass
- Kissing balloon angioplasty +/- stent, so named because the two common iliac stents touch each other in the distal aorta.
- Aorto-iliac bypass graft
- Axillary-bi-femoral[9][10] and femoral-femoral bypass (sometimes abbreviated "ax-fem fem-fem")
History
The condition was first described by Robert Graham in 1814.[6][7] Its three classic symptoms was ascribed to René Leriche.[11] Leriche, a French surgeon, linked the pathophysiology with the anatomy of the condition. John Hunter's dissections of atherosclerotic aortic bifurcations from the late 18th century are preserved at the Hunterian Museum, but Leriche was first to publish on the subject based on a patient he treated with the condition at the age of 30. Following treatment the 30-year-old was able to walk without pain and maintain an erection.[12]
References
- 1 2 3 4 5 6 7 8 Meyermann, K; Caputo, FJ (August 2017). "Treatment of Abdominal Aortic Pathology". Cardiology clinics. 35 (3): 431–439. doi:10.1016/j.ccl.2017.03.009. PMID 28683911.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Heaton, J; Khan, YS (January 2022). "Aortoiliac Occlusive Disease". PMID 32644512.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 "Aortoiliac Occlusive Disease: Practice Essentials, Pathophysiology, Etiology". 16 October 2021. Archived from the original on 31 March 2022. Retrieved 30 March 2022.
- ↑ Cameron, John L.; Cameron, Andrew M. (29 October 2019). Current Surgical Therapy E-Book. Elsevier Health Sciences. p. 968. ISBN 978-0-323-64060-2. Archived from the original on 31 March 2022. Retrieved 30 March 2022.
- 1 2 Brown, KN; Muco, E; Gonzalez, L (January 2022). "Leriche Syndrome". PMID 30855836.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Graham, Robert (1814). "Case of Obstructed Aorta". Med. Chir. Tr. 5: 287–456.9. PMC 2128948. PMID 20895223. Archived from the original on 2019-10-29. Retrieved 2021-10-30.
- 1 2 JAWOR, WJ; PLICE, SG (10 May 1952). "Thrombotic obliteration of the abdominal aorta; report of a case". Journal of the American Medical Association. 149 (2): 142–3. doi:10.1001/jama.1952.72930190007009b. PMID 14917575.
- 1 2 F. Charles Brunicardi; Dana K. Andersen; Timothy R. Billiar (5 June 2014). Schwartz's Principles of Surgery, 10th edition. McGraw-Hill Education. ISBN 978-0-07-180092-1.
- ↑ Lee BY, Guerra J (1994). "Axillofemoral bypass graft in a spinal cord injured patient with impending gangrene". The Journal of the American Paraplegia Society. 17 (4): 171–6. doi:10.1080/01952307.1994.11735932. PMID 7869060.
- ↑ McKinsey JF (1995). "Extra-anatomic reconstruction". Surg. Clin. North Am. 75 (4): 731–40. doi:10.1016/S0039-6109(16)46694-6. PMID 7638717.
- ↑ synd/2747 at Who Named It?
- ↑ Leriche, R; Morel, A (February 1948). "The Syndrome of Thrombotic Obliteration of the Aortic Bifurcation". Annals of Surgery. 127 (2): 193–206. doi:10.1097/00000658-194802000-00001. PMC 1513778. PMID 17859070.
External links
| Classification | |
|---|---|
| External resources |