Thoracic aortic aneurysm
| Thoracic aortic aneurysm | |
|---|---|
| Other names: Aneurysm - thoracic aortic;[1] thoracic aorta aneurysm[2] | |
 | |
| Specialty | Cardiac surgery, vascular surgery |
| Symptoms | Initially none[2] |
| Complications | Aortic dissection, aortic regurgitation, aortic rupture[2] |
| Usual onset | 50s and 60s[2] |
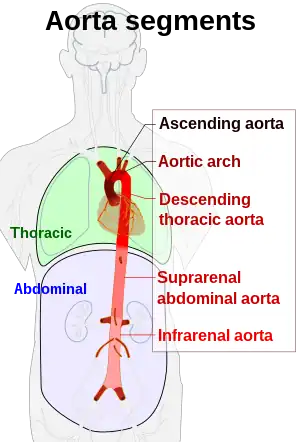
| Types | Root, ascending, arch, descending[2] |
| Risk factors | High blood pressure, smoking, family history, bicuspid aortic valve, connective-tissue disorders[2][3] |
| Diagnostic method | Medical imaging[2] |
| Treatment | Beta blockers, angiotensin-converting enzymes, statins, surgery[2] |
| Frequency | 1 in 10,000 people a year[2] |
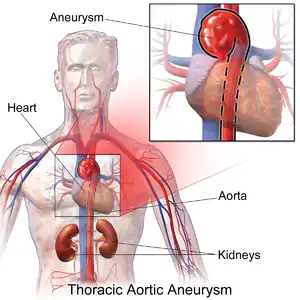
Thoracic aortic aneurysm (TAA) is an aortic aneurysm that occurs above the diaphragm.[4] Initially there are generally no symptoms.[2] Occasionally chest pain, shortness of breath, superior vena cava syndrome, or hoarseness may occur.[2] Complications may include aortic dissection, aortic regurgitation, or aortic rupture.[2]
Risk factors include high blood pressure, smoking, family history of the condition, bicuspid aortic valve, and connective-tissue disorders.[2][3] About 20% of those affected have a family history.[3] Less common causes include syphilis, arteritis, and following major trauma.[2][3] Diagnosis is generally by CT scan.[2]
Management often involves the use of beta blockers.[2] Angiotensin-converting enzymes and statins may also be used.[2] Surgery to replace the aorta is recommended when it becomes larger than 5.0 cm to 6.5 cm.[2] Those with complications may require immediate surgery.[2] Five-year survival following planned surgery is 85%, while in those who require immediate surgery it is less than 40%.[2]
Thoracic aortic aneurysm newly occurs in about 1 in 10,000 people a year.[2] About 0.25% of people are currently affected.[2] Males are affected more often than females.[2] Detection most commonly occurs in peoples 50s and 60s.[2] It is less common than abdominal aortic aneurysm.[3] The condition was first described in the 1500s by Andreas Vesalius.[5] Successful surgery was first completed in 1953.[6]
Signs and symptoms
Complications
The principal causes of death due to thoracic aneurysmal disease are dissection and rupture. Once rupture occurs, the mortality rate is 50–80%. Most deaths in Marfan syndrome are the result of aortic disease.
Causes
There are a number of causes.[7] Aneurysms in people younger than 40 usually involve the ascending aorta due to a weakening of the aortic wall associated with connective tissue disorders like the Marfan and Ehler-Danlos syndromes or bicuspid aortic valve. Younger people may develop aortic aneurysms of the thoracoabdominal aorta after an aortic dissection. It can also be caused by blunt injury. Atherosclerosis is the principal cause of descending aortic aneurysms, while aneurysms of the aortic arch may be due to dissection, atherosclerosis, or inflammation.[8]
Risk factors
High blood pressure and cigarette smoking are the most common risk factors, though the importance of genetics has been increasingly recognized. Approximately 10 percent of people have other family members with aortic aneurysms. Individuals with a history of aneurysms in other parts of the body also have a higher chance of developing a thoracic aortic aneurysm.[9]
Diagnosis
Thoracic aortic aneurysm is defined as a cross-sectional diameter exceeding the following cutoff:
A diameter of 3.5 cm is generally considered dilated.[10] However, average values vary with age and size of the reference population, as well as different segments of the aorta.
| Small and young | Large and elderly | |
| Ascending aorta | 3.3 cm | 4.3 cm |
| Descending aorta | 2.3 cm | 3.2 cm |
 Thoracic aortic aneurysm with arrow marking the lateral border of the aorta
Thoracic aortic aneurysm with arrow marking the lateral border of the aorta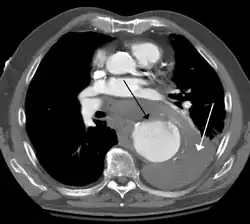 Contrast enhanced CT of a ruptured large (7 cm) thoracic aneurysm, with black arrow indicating the aorta, and white arrow blood in the thorax
Contrast enhanced CT of a ruptured large (7 cm) thoracic aneurysm, with black arrow indicating the aorta, and white arrow blood in the thorax- Ruptured thoracic aortic aneurysm as seen on ultrasound[13]
Screening
Guidelines from 2010 by the American College of Cardiology and the American Heart Association recommends:
- First-degree relatives of people with a genetic cause of thoracic aortic aneurysm or dissection should have aortic imaging to identify asymptomatic disease.
- People with symptoms suggestive of thoracic aortic dissection should be routinely evaluated "to establish a pretest risk of disease that can then be used to guide diagnostic decisions."
- People diagnosed with Marfan syndrome should immediately have an echocardiogram to measure the aorta and followed up six months later to check for aortic enlargement.[14]
Treatment

The size cut off for aortic aneurysm is crucial to its treatment. A thoracic aorta greater than 4.5 cm is generally defined as aneurysmal, while a size greater than 6 cm is the distinction for treatment, which can be either endovascular or surgical, with the former reserved for pathology at the descending aorta.[15]
Indication for surgery may depend upon the size of the aneurysm. Aneurysms in the ascending aorta may require surgery at a smaller size than aneurysms in the descending aorta.[16]
Treatment may be via open or via endovascular means.
Epidemiology
Diagnosis generally occurs in peoples 60s and 70s.[17][18]
Each year in the United States, some 45,000 people die from diseases of the aorta and its branches. Acute aortic dissection, a life-threatening event due to a tear in the aortic wall, affects 5 to 10 per million population each year, most often men between the ages of 50 and 70; of those that occur in women younger than 40, nearly half arise during pregnancy. The majority of these deaths occur as a result of complications of thoracic aneurysmal disease[19]
References
- ↑ "Thoracic aortic aneurysm: MedlinePlus Medical Encyclopedia". medlineplus.gov. Archived from the original on 29 May 2019. Retrieved 29 May 2019.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Faiza, Z; Sharman, T (January 2023). "Thoracic Aorta Aneurysm". PMID 32119454.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 5 Isselbacher, Eric M. (15 February 2005). "Thoracic and Abdominal Aortic Aneurysms". Circulation. 111 (6): 816–828. doi:10.1161/01.CIR.0000154569.08857.7A.
- ↑ "Thoracic aortic aneurysm". Mayo Clinic. Archived from the original on 11 June 2023. Retrieved 12 June 2023.
- ↑ Thompson, Jesse E. (October 1998). "Early history of aortic surgery". Journal of Vascular Surgery. 28 (4): 746–752. doi:10.1016/S0741-5214(98)70107-7.
- ↑ Bobadilla, Joseph L. (1 July 2013). "From Ebers to EVARs: A Historical Perspective on Aortic Surgery". AORTA. 1 (2): 89–95. doi:10.12945/j.aorta.2013.13-004.
- ↑ Aneurysms: Aneurysms and Aortic Dissection at Merck Manual of Diagnosis and Therapy Home Edition
- ↑ Golledge, J.; Norman, P. (June 2010). "Atherosclerosis and abdominal aortic aneurysm: Cause, response or common risk factors?". Arteriosclerosis, Thrombosis, and Vascular Biology. 30 (6): 1075–1077. doi:10.1161/ATVBAHA.110.206573. PMC 2874982. PMID 20484703.
- ↑ Thoracic Aortic Disease - Northwestern Memorial Hospital. Thoracic Aortic Aneurysm Archived 2012-05-02 at the Wayback Machine
- 1 2 Bret P Nelson (2015-10-01). "Thoracic Aneurysm". Medscape. Archived from the original on 2017-09-24. Retrieved 2017-04-16.
- ↑ Cho, In-Jeong; Jang, Sung-Yeol; Chang, Hyuk-Jae; Shin, Sanghoon; Shim, Chi Young; Hong, Geu-Ru; Chung, Namsik (2014). "Aortic Aneurysm Screening in a High-Risk Population: A Non-Contrast Computed Tomography Study in Korean Males with Hypertension". Korean Circulation Journal. 44 (3): 162–169. doi:10.4070/kcj.2014.44.3.162. ISSN 1738-5520. PMC 4037638. PMID 24876857.
- ↑ Wolak, Arik; Gransar, Heidi; Thomson, Louise E.J.; Friedman, John D.; Hachamovitch, Rory; Gutstein, Ariel; Shaw, Leslee J.; Polk, Donna; Wong, Nathan D.; Saouaf, Rola; Hayes, Sean W.; Rozanski, Alan; Slomka, Piotr J.; Germano, Guido; Berman, Daniel S. (2008). "Aortic Size Assessment by Noncontrast Cardiac Computed Tomography: Normal Limits by Age, Gender, and Body Surface Area". JACC: Cardiovascular Imaging. 1 (2): 200–209. doi:10.1016/j.jcmg.2007.11.005. ISSN 1936-878X. PMID 19356429.
- ↑ "UOTW#64 - Ultrasound of the Week". Ultrasound of the Week. 25 November 2015. Archived from the original on 9 May 2017. Retrieved 27 May 2017.
- ↑ Hiratzka LF, Bakris GL, Beckman JA, et al. (April 2010). "2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine". J. Am. Coll. Cardiol. 55 (14): e27–e129. doi:10.1016/j.jacc.2010.02.015. PMID 20359588.
- ↑ Makaroun MS, Dillavou ED, Kee ST, et al. (January 2005). "Endovascular treatment of thoracic aortic aneurysms: results of phase II multicenter trial of the GORE TAG thoracic endoprosthesis". J. Vasc. Surg. 41 (1): 1–9. doi:10.1016/j.jvs.2004.10.046. PMID 15696036.
- ↑ "Treatment Considerations related to Thoracic Aortic Aneurysm". Archived from the original on 2011-08-20. Retrieved 2010-10-23.
- ↑ "Abdominal Aortic Aneurysms". The Lecturio Medical Concept Library. 16 October 2020. Archived from the original on 2021-06-25. Retrieved 2021-06-25.
- ↑ Golledge, J.; Norman, P. (June 2010). "Atherosclerosis and abdominal aortic aneurysm: Cause, response or common risk factors?". Arteriosclerosis, Thrombosis, and Vascular Biology. 30 (6): 1075–1077. doi:10.1161/ATVBAHA.110.206573. PMC 2874982. PMID 20484703.
- ↑ Aggarwal, S.; Qamar, A; Sharma, V; Sharma, A (2011). "Abdominal aortic aneurysm: A comprehensive review". Experimental and Clinical Cardiology. 16 (1): 11–15. PMC 3076160. PMID 21523201.
External links
| Classification | |
|---|---|
| External resources |