Hypoparathyroidism
| Hypoparathyroidism | |
|---|---|
| Other names: Parathyroid hormone deficiency[1] | |
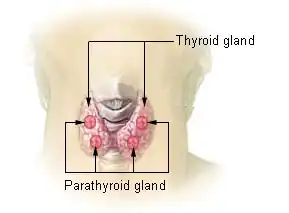 | |
| Location of the four parathyroid glands | |
| Specialty | Endocrinology |
| Symptoms | Muscle cramps, muscle twitching, tingling of the hands and feet, depression, rough skin, loss of hair[2] |
| Complications | Osteoporosis, kidney stones[3][1] |
| Causes | Complication of thyroid removal, DiGeorge syndrome, immune system-related damage, hemochromatosis, radiation therapy, low magnesium[1] |
| Diagnostic method | Low blood calcium and PTH[3] |
| Differential diagnosis | Pseudohypoparathyroidism[1] |
| Treatment | Calcium and vitamin D supplementation[3] |
| Medication | Recombinant parathyroid hormone (rhPTH)[3] |
| Frequency | Rare[2] |
Hypoparathyroidism is when the parathyroid glands underproduction parathyroid hormone (PTH).[2] This results in low blood calcium and high blood phosphorus, with symptoms of muscle cramps and muscle twitching.[2] Other symptoms may include tingling of the hands and feet and depression.[2] There may be poorly developed teeth, rough scaly skin, brittle nails and little hair growth.[4] Complications may include osteoporosis and kidney stones.[3][1]
The most common cause is as a complication of thyroid removal or other surgery to the neck.[1][2] Other causes may include the genetic disorder DiGeorge syndrome, immune system-related damage, hemochromatosis, radiation therapy, and low magnesium.[1] Diagnosis is based on blood tests for PTH and calcium.[3]
The primary treatment is calcium and vitamin D supplementation.[3] Initially large amounts of calcium gluconate may be given by injection.[3][1] If this is not sufficient recombinant parathyroid hormone (rhPTH) may be used.[3] A diet high in calcium and low in phosphorus is also recommended.[2] Outcomes are generally good with treatment.[1]
Hypoparathyroidism is rare.[2] In the United States about 3 per 10,000 people are affected.[1] Males and females are affected equally frequently.[5] The association between thyroid removal and muscle spasms was described in 1884.[6]
Signs and symptoms
The main symptoms of hypoparathyroidism are the result of the low blood calcium level, which interferes with normal muscle contraction and nerve conduction. As a result, people with hypoparathyroidism can experience paresthesia, an unpleasant tingling sensation around the mouth and in the hands and feet, as well as muscle cramps and severe spasms known as "tetany" that affect the hands and feet.[7] Many also report a number of subjective symptoms such as fatigue, headaches, bone pain and insomnia.[8] Crampy abdominal pain may occur.[9] Physical examination of someone with hypocalcemia may show tetany, but it is also possible to provoke tetany of the facial muscles by tapping on the facial nerve (a phenomenon known as Chvostek's sign) or by using the cuff of a sphygmomanometer to temporarily obstruct the blood flow to the arm (a phenomenon known as Trousseau's sign of latent tetany).[9]
A number of medical emergencies can arise in people with low calcium levels. These are seizures, severe irregularities in the normal heart beat, as well as spasm of the upper part of the airways or the smaller airways known as the bronchi (both potentially causing respiratory failure).[8]
Causes
Hypoparathyroidism can have the following causes:[8]
- Removal of, or trauma to, the parathyroid glands due to thyroid surgery (thyroidectomy), parathyroid surgery (parathyroidectomy) or other surgical interventions in the central part of the neck (such as operations on the larynx and/or pharynx) is a recognized cause. It is the most common cause of hypoparathyroidism. Although surgeons generally make attempts to spare normal parathyroid glands at surgery, inadvertent injury to the glands or their blood supply is still common. When this happens, the parathyroids may cease functioning. This is usually temporary but occasionally long term (permanent).
- Kenny-Caffey Syndrome
- Autoimmune invasion and destruction is the most common non-surgical cause. It can occur as part of autoimmune polyendocrine syndromes.
- Hemochromatosis can lead to iron accumulation and consequent dysfunction of a number of endocrine organs, including the parathyroids.
- Absence or dysfunction of the parathyroid glands is one of the components of chromosome 22q11 microdeletion syndrome (other names: DiGeorge syndrome, Schprintzen syndrome, velocardiofacial syndrome).
- Magnesium deficiency
- A defect in the calcium receptor leads to a rare congenital form of the disease
- Idiopathic (of unknown cause), occasionally familial (e.g. Barakat syndrome (HDR syndrome) a genetic development disorder resulting in hypoparathyroidism, sensorineural deafness, and kidney disease)
Mechanism
The parathyroid glands are so named because they are usually located behind the thyroid gland in the neck. They arise during fetal development from structures known as the third and fourth pharyngeal pouch. The glands, usually four in number, contain the parathyroid chief cells that sense the level of calcium in the blood through the calcium-sensing receptor and secrete parathyroid hormone. Magnesium is required for PTH secretion. Under normal circumstances, the parathyroids secrete PTH to maintain a calcium level within normal limits, as calcium is required for adequate muscle and nerve function (including the autonomic nervous system). PTH acts on several organs to increase calcium levels. It increases calcium absorption in the bowel, while in the kidney it prevents calcium excretion and increases phosphate release and in bone it increases calcium through bone resorption.
Diagnosis
Diagnosis is by measurement of calcium, serum albumin (for correction) and PTH in blood. If necessary, measuring cAMP (cyclic AMP) in the urine after an intravenous dose of PTH can help in the distinction between hypoparathyroidism and other causes.
Differential diagnoses are:
- Pseudohypoparathyroidism (normal PTH levels but tissue insensitivity to the hormone, associated with intellectual disability and skeletal deformities) and pseudopseudohypoparathyroidism.
- Vitamin D deficiency or hereditary insensitivity to this vitamin (X-linked dominant).
- Malabsorption
- Kidney disease
- Medication: steroids, diuretics, some antiepileptics.
Other tests include ECG for abnormal heart rhythms, and measurement of blood magnesium levels.
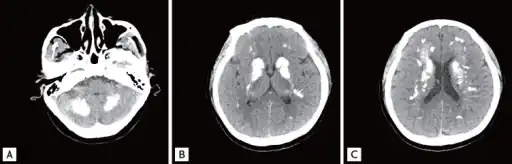 a-c)Brain computed tomography shows diffuse symmetric parenchymal calcifications
a-c)Brain computed tomography shows diffuse symmetric parenchymal calcifications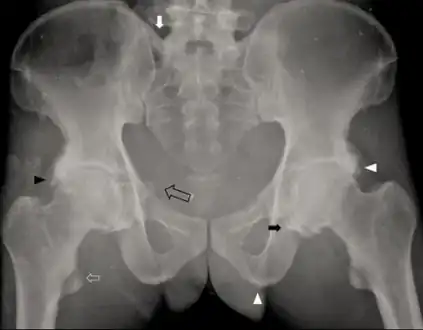 Individual with idiopathic hypoparathyroidism-diffuse osteosclerosis, capsular ossification around bilateral hip joints arrow, ossification of bilateral iliolumbar ligaments arrow, irregular bony excrescences arrowhead, subtle calcification of the right sacrospinous ligament open arrow
Individual with idiopathic hypoparathyroidism-diffuse osteosclerosis, capsular ossification around bilateral hip joints arrow, ossification of bilateral iliolumbar ligaments arrow, irregular bony excrescences arrowhead, subtle calcification of the right sacrospinous ligament open arrow
Related conditions
| Condition | Appearance | PTH levels | Calcitriol | Calcium | Phosphates | Imprinting | |
|---|---|---|---|---|---|---|---|
| Hypoparathyroidism | Normal | Low | Low | Low | High | Not applicable | |
| Pseudohypoparathyroidism | Type 1A | Skeletal defects | High | Low | Low | High | Gene defect from mother (GNAS1) |
| Type 1B | Normal | High | Low | Low | High | Gene defect from mother (GNAS1 and STX16) | |
| Type 2 | Normal | High | Low | Low | High | ? | |
| Pseudopseudohypoparathyroidism | Skeletal defects | Normal | Normal | Normal[10] | Normal | gene defect from father | |
Treatment
Severe hypocalcaemia, a potentially life-threatening condition, is treated as soon as possible with intravenous calcium (e.g. as calcium gluconate). Generally, a central venous catheter is recommended, as the calcium can irritate peripheral veins and cause phlebitis. In the event of a life-threatening attack of low calcium levels or tetany (prolonged muscle contractions), calcium is administered by intravenous (IV) infusion. Precautions are taken to prevent seizures or larynx spasms. The heart is monitored for abnormal rhythms until the person is stable. When the life-threatening attack has been controlled, treatment continues with medicine taken by mouth as often as four times a day.
Long-term treatment of hypoparathyroidism is with vitamin D analogs and calcium supplementation, but may be ineffective in some due to potential renal damage.[11] The N-terminal fragment of parathyroid hormone (PTH 1-34) has full biological activity. The use of pump delivery of synthetic PTH 1-34 provides the closest approach to physiologic PTH replacement therapy.[12] Injections of recombinant human parathyroid hormone are available as treatment in those with low blood calcium levels.[13]
See also
References
- 1 2 3 4 5 6 7 8 9 10 Hans, SK; Levine, SN (January 2022). "Hypoparathyroidism". PMID 28722928.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 5 6 7 8 "Hypoparathyroidism". nhs.uk. 27 February 2018. Archived from the original on 24 March 2022. Retrieved 12 May 2022.
- 1 2 3 4 5 6 7 8 9 "Hypoparathyroidism - Endocrine and Metabolic Disorders". Merck Manuals Professional Edition. Archived from the original on 22 March 2022. Retrieved 13 May 2022.
- ↑ James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "24. Endocrine diseases". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 499. ISBN 978-0-323-54753-6. Archived from the original on 2022-06-14. Retrieved 2022-06-07.
- ↑ "Hypoparathyroidism". NORD (National Organization for Rare Disorders). Archived from the original on 6 December 2018. Retrieved 14 May 2022.
- ↑ Feldman, Edward C.; Nelson, Richard William (1 January 2004). Canine and Feline Endocrinology and Reproduction. Elsevier Health Sciences. p. 716. ISBN 978-0-7216-9315-6. Archived from the original on 14 May 2022. Retrieved 14 May 2022.
- ↑ Shoback D (July 2008). "Hypoparathyroidism". N. Engl. J. Med. 359 (4): 391–403. doi:10.1056/NEJMcp0803050. PMID 18650515.
- 1 2 3 Bilezikian JP, Khan A, Potts JT, et al. (October 2011). "Hypoparathyroidism in the adult: epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment, and challenges for future research". J. Bone Miner. Res. 26 (10): 2317–37. doi:10.1002/jbmr.483. PMC 3405491. PMID 21812031.
- 1 2 Potts Jr JT (2005). "Diseases of the parathyroid gland". In Kasper DL, Braunwald E, Fauci AS, et al. (eds.). Harrison's Principles of Internal Medicine (16th ed.). New York, NY: McGraw-Hill. pp. 2249–68. ISBN 978-0-07-139140-5.
- ↑ Shahid Hussain; Sharif Aaron Latif; Adrian Hall (1 July 2010). Rapid Review of Radiology. Manson Publishing. pp. 262–. ISBN 978-1-84076-120-7. Retrieved 30 October 2010.
- ↑ Winer KK, Yanovski JA, Cutler GB Jr. Synthetic human parathyroid hormone 1-34 vs calcitriol and calcium in the treatment of hypoparathyroidism: Results of a randomized crossover trial" JAMA 1996;276:631-636
- ↑ Winer KK, Zhang B, Shrader J, et al. Synthetic human parathyroid hormone 1-34 replacement therapy: A randomized crossover trial comparing pump versus injections in the treatment of chronic hypoparathyroidism. J Clin Endocrinol Metab. Nov.2011.
- ↑ "FDA approves Natpara to control low blood calcium levels in patients with hypoparathyroidism". fda.gov/. Archived from the original on 30 January 2015. Retrieved 30 January 2015.
External links
| Classification | |
|---|---|
| External resources |