Lumacaftor/ivacaftor
 | |
| Combination of | |
|---|---|
| Lumacaftor | CFTR chaperone |
| Ivacaftor | CFTR potentiator |
| Names | |
| Trade names | Orkambi, Lucaftor |
| Clinical data | |
| Main uses | Cystic fibrosis[1] |
| Side effects | Shortness of breath, nausea, diarrhea, feeling tired, hearing problems, rash[1][2] |
| WHO AWaRe | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Pregnancy category |
|
| Routes of use | By mouth |
| Defined daily dose | not established[4] |
| External links | |
| AHFS/Drugs.com | Monograph |
| Legal | |
| License data | |
| Legal status | |
Lumacaftor/ivacaftor, sold under the brand name Orkambi among others, is a combination of lumacaftor and ivacaftor used to treat people with cystic fibrosis who have two copies of the F508del mutation.[1] It is unclear if it is useful in cystic fibrosis due to other causes.[1] It is taken by mouth.[1]
Common side effects include shortness of breath, nausea, diarrhea, feeling tired, hearing problems, and rash.[1][2] Severe side effects may include liver problems and cataracts.[1] Ivacaftor increases the activity of the CFTR protein, while lumacaftor improves protein folding of the CFTR protein.[1][5]
It was approved for medical use in the United States in 2015 and in Canada in 2016.[1][5] In the United Kingdom the medication costs the NHS more than £4,000 a month as of 2018.[2] In the United States it costs more than $US 22,000 a month as of 2018.[6][7] While its use was not recommended in the United Kingdom as of 2018,[2] pricing was agreed upon in 2019 and it is expected to be covered by November of that year.[8]
Medical use
The combination of lumacaftor/ivacaftor is used to treat people with cystic fibrosis who have two copies of the F508del mutation in the cystic fibrosis transmembrane conductance regulator (CFTR), the defective protein that causes the disease.[3][9] This genetic abnormality is present in about half of cystic fibrosis cases in Canada.[5] Its use is not recommended for anyone with cystic fibrosis in the United Kingdom as of 2018.[2]
While the medication resulted in improvement in the amount of air a person can breath out in one second, the improvement seen did not reach a clinically important amount.[5] The medication also does not appear to change a person's quality of life or the number of times a year a person has a worsening of lung function.[5] Effects on life expectancy are unclear.[5]
Dosage
The defined daily dose is not established.[4]
Side effects
Some people taking the combination drug had elevated transaminases; the combination drug should be used with caution for people with advanced liver disease and liver function should be measured for the first three months for all people starting the combination drug.[3]
People starting the combination have respiratory discomfort, and some children taking the combination drug developed cataracts.[3]
Lumacaftor/ivacaftor may interfere with hormonal contraceptives. Dosage of the combination drug should be reduced if the person is taking a drug that inhibits CYP3A, and inducers of CYP3A should not be used concomitantly.[3]
Mechanism of action
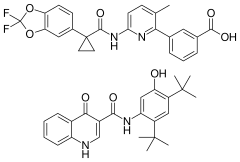
F508del is a mutation that causes the CFTR protein to misfold and cells destroy such proteins soon after they are made; lumacaftor acts as a chaperone during protein folding and increases the number of CFTR proteins that are trafficked to the cell surface.[10][11] Ivacaftor is a potentiator of CFTR that is already at the cell surface, increasing the probability that the defective channel will be open and allow chloride ions to pass through the channel pore.[9] The two drugs have synergistic effects.[9]
Physical properties
Each of lumacaftor and ivacaftor is a white to off-white powder that is practically insoluble in water. The combination drug is a single pill containing 200 mg of lumacaftor and 125 mg of ivacaftor.[3]
History
Lumacaftor/ivacaftor was approved by the FDA in July 2015 under breakthrough therapy status and under a priority review.[12] Previously approved for adults and pre-teens, approved on 8-7-18 for children age 2–5.
Society and culture
As of March 2016 the combination drug cost $259,000 a year in the United States.[13]
In Denmark, it was estimated in August 2015 that if the drug were introduced, the cost would amount to 2 million Danish krones (approximately 270,000 euro) each year per person.[14]
The Dutch Minister of Health announced in October 2017 that the drug would not be admitted to the public health insurance package, making it impossible to have treatment with the drug covered by Dutch health insurance. The minister stated that the price for the drug, negotiated to 170,000 euro per patient per year, is "unacceptably high in relation to the relatively modest effect, as determined by the (Dutch) Healthcare Institute". Approximately 750 patients are affected by this decision.[15] On 25 October, the Dutch Minister of Health announced that an agreement had been brokered with Vertex Pharmaceuticals, the company that manufactures the drug, resulting in admittance to the Dutch public health insurance package. Part of the agreement is that the end result of the negotiation about the price of the treatment will not be disclosed.[16]
Protracted discussions within the United Kingdom were brought to a conclusion in September and October 2019 as NHS Scotland and NHS England both struck deals with Vertex respectively. This followed discussions where Vertex had wanted £105 000 per patient for Orkambi.[8]
The drug was not patented in Argentina, so can be made by other companies. Buyers' clubs in the UK have been buying the generic version from the Argentinian company Gador.[17]
References
- 1 2 3 4 5 6 7 8 9 "Orkambi Monograph for Professionals". Drugs.com. AHFS. Archived from the original on 9 January 2019. Retrieved 8 January 2019.
- 1 2 3 4 5 British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 293–294. ISBN 9780857113382. Archived from the original on 2021-08-28. Retrieved 2019-02-04.
- 1 2 3 4 5 6 "Orkambi" (PDF). www.accessdata.fda.gov. 2015. Archived (PDF) from the original on 20 September 2018. Retrieved 8 January 2019.
- 1 2 "WHOCC - ATC/DDD Index". www.whocc.no. Archived from the original on 1 July 2021. Retrieved 9 September 2020.
- 1 2 3 4 5 6 "[116] New drug for cystic fibrosis: Regulatory approval, clinical uncertainty?". Therapeutics Initiative. Therapeutics Initiative. 28 December 2018. Archived from the original on 9 January 2019. Retrieved 8 January 2019.
- ↑ Ferkol T, Quinton P (September 2015). "Precision Medicine: At What Price?". American Journal of Respiratory and Critical Care Medicine. 192 (6): 658–9. doi:10.1164/rccm.201507-1428ED. PMID 26207804.
- ↑ Thomas, Katie (24 June 2018). "A Drug Costs $272,000 a Year. Not So Fast, Says New York State". The New York Times. Archived from the original on 9 January 2019. Retrieved 8 January 2019.
- 1 2 Kmietowicz Z (October 2019). "Cystic fibrosis drugs to be available on NHS in England within 30 days". BMJ. 367: l6206. doi:10.1136/bmj.l6206. PMID 31649013. S2CID 204883523. Archived from the original on 2019-10-25. Retrieved 2019-10-25.
- 1 2 3 Kuk K, Taylor-Cousar JL (December 2015). "Lumacaftor and ivacaftor in the management of patients with cystic fibrosis: current evidence and future prospects". Therapeutic Advances in Respiratory Disease. 9 (6): 313–26. doi:10.1177/1753465815601934. PMID 26416827.
- ↑ "Orkambi (lumacaftor and ivacaftor)". CenterWatch. Archived from the original on 19 March 2016. Retrieved 24 March 2016.
- ↑ Ren HY, Grove DE, De La Rosa O, Houck SA, Sopha P, Van Goor F, et al. (October 2013). "VX-809 corrects folding defects in cystic fibrosis transmembrane conductance regulator protein through action on membrane-spanning domain 1". Molecular Biology of the Cell. 24 (19): 3016–24. doi:10.1091/mbc.E13-05-0240. PMC 3784376. PMID 23924900.
- ↑ "FDA approves new treatment for cystic fibrosis". United States Food and Drug Administration. July 2, 2015. Archived from the original on January 26, 2018. Retrieved December 16, 2019.
- ↑ Wasserman, Emily (March 23, 2016). "NICE gives initial thumbs-down to Vertex's CF combo med Orkambi, citing costs". FiercePharma. Archived from the original on 2016-03-28. Retrieved 2016-03-25.
- ↑ Kjeldtoft, Sebastian Stryhn (1 August 2015). "10-årige Elisabeth spiser 33 piller om dagen" (in Danish). Information. Archived from the original on 3 August 2015. Retrieved 1 August 2015.
{{cite news}}: CS1 maint: unrecognized language (link) - ↑ "Onderhandelingen over taaislijmziekte weer mislukt" [Negotiations over throat gland disease failed again] (in Dutch). NOS. Algemeen Nederlands Persbureau. 9 August 2017. Archived from the original on 10 October 2017. Retrieved 11 October 2017.
{{cite news}}: CS1 maint: unrecognized language (link) - ↑ Zenthis R (25 August 2017). "Medicijn tegen taaislijmziekte toch opgenomen in basispakket" [Cystic Fibrosis medicine approved for basic insurance package] (in Dutch). Nu.nl. Algemeen Nederlands Persbureau/Nu.nl. Archived from the original on 25 October 2017. Retrieved 25 October 2017.
{{cite news}}: CS1 maint: unrecognized language (link) - ↑ Boseley, Sarah (4 June 2019). "Families create buyers club for cut-price cystic fibrosis drug". www.theguardian.com. Archived from the original on 18 May 2020. Retrieved 29 January 2020.
External links
| Identifiers: |
|---|