Pituitary stalk interruption syndrome
| Pituitary stalk interruption syndrome (PSIS) | |
|---|---|
| Other names: Ectopic neurohypophysis | |
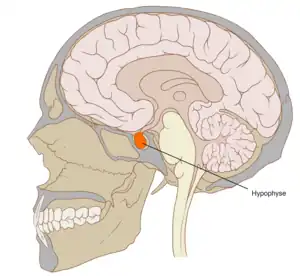 | |
| The location of the pituitary gland within the skull (indicated in orange) | |
| Specialty | Endocrinology, neurology, neonatology, paediatrics |
| Symptoms | Hypoglycaemia, jaudice, micropenis, cryptorchidism, etc. |
| Complications | Seizures, retarded physical and intellectual development, delayed puberty, death, etc. |
| Types | Congenital |
| Risk factors | Genetic predisposition (relative(s) with the condition) |
| Diagnostic method | MRI scan |
| Treatment | Hormone replacement |
| Frequency | Unclear, ~1,000 cases reported |
Pituitary stalk interruption syndrome (PSIS) is a congenital disorder characterised by the triad of an absent or exceedingly thin pituitary stalk, an ectopic or absent posterior pituitary and/or absent or hypoplastic anterior pituitary.[1][2]
Signs and symptoms
Affected individuals may present with hypoglycaemia during the neonatal period, or with growth retardation during childhood (those diagnosed in the neonatal period appear to be affected by a particularly severe form of the disorder). PSIS is a common cause of congenital hypopituitarism, and causes a permanent growth hormone deficit. Some PSIS-affected individuals may also present with adrenal hypoplasia (5-29%), diabetes insipidus (5-29%), primary amenorrhea (5-29%), hypothyroidism (30-79%), failure to thrive (80-99%), septooptic dysplasia (5-29%), and Fanconi anaemia. PSIS may be isolated, or, commonly, present with extra-pituitary malformations.[1][2][3]
PSIS features in neonates (may) include:[1][2][3]
- hypoglycaemia (30-79%)
- (prolonged) jaundice
- micropenis (30-79%)
- cryptorchidism (5-29%)
- delayed intellectual development
- death in infancy (5-29%)
- congenital abnormalities
PSIS features in later childhood (may) include:[1][2][3]
- short stature (80-99%)
- seizures (5-29%)
- hypotension
- delayed intellectual development
- delayed puberty (30-79%)
PSIS is associated with a higher frequency of breech presentation, Caeserian section, and/or low Apgar score, though these are likely consequences rather than causes.[3]
Cause
The cause of the condition is as of yet unknown. Rare genetic mutations may cause familial cases, however, these account for less than 5% of cases.[2]
Diagnosis

Management
Treatment should commence as soon as a diagnosis is established to avoid complications, and consists of hormone replacement, particularly with growth hormone.[1]
Prognosis
Prognosis is generally good in cases of prompt diagnosis and management. Delays may lead to seizures (due to hypoglycaemia), hypotension (due to cortisol deficiency), and/or intellectual disability (due to thyroid endocrine deficits). Due to the before-mentioned factors, mortality and morbidity is higher than that of the general population, particularly during the first 2 years of life.[3]
Epidemiology
The prevalence of PSIS is unknown, however, some 1,000 cases have been reported either with or without the full triad.[3]
References
- 1 2 3 4 5 "Pituitary stalk interruption syndrome". Genetic and Rare Diseases Information Center (GARD) – an NCATS Program. U.S. National Institutes of Health. Archived from the original on 2018-08-12. Retrieved 2018-08-11.
- 1 2 3 4 5 6 Bar C, Zadro C, Diene G, Oliver I, Pienkowski C, Jouret B, et al. (November 2015). "Pituitary Stalk Interruption Syndrome from Infancy to Adulthood: Clinical, Hormonal, and Radiological Assessment According to the Initial Presentation". PLOS ONE. 10 (11): e0142354. Bibcode:2015PLoSO..1042354B. doi:10.1371/journal.pone.0142354. PMC 4643020. PMID 26562670.
- 1 2 3 4 5 6 Brauner R. "Pituitary stalk interruption syndrome". Orphanet. Archived from the original on 2018-08-12. Retrieved 2018-08-11.
External links
| External resources |
|
|---|