Post-kala-azar dermal leishmaniasis
| Post-kala-azar dermal leishmaniasis | |
|---|---|
| Other names: Post-kala-azar dermatosis[1] | |
 | |
| PKDL rash on the hand | |
| Specialty | Infectious disease, dermatology |
| Symptoms | White areas of skin, nodular lesions[2] |
| Usual onset | Within a few months to years post VL[3] |
| Causes | Possibly immune related following visceral leishmaniasis[2] |
| Diagnostic method | Generally based on symptoms[2] |
| Differential diagnosis | Leprosy, xanthoma, systemic lupus erythematosus, sarcoidosis, syphilis[2][4] |
| Treatment | Miltefosine, sodium stibogluconate, amphotericin B[2][3] |
| Frequency | 2.5% to 20% post VL[3] |
Post-kala-azar dermal leishmaniasis (PKDL) is a complication following visceral leishmaniasis (VL) characterized by white areas of skin.[2] There may also be smaller or larger bumps.[2] The rash usually begins around the mouth and spreads to the face and upper trunk.[2][4] There are generally few other symptoms.[2]
Onset in India is generally within months to years of treatment of VL, while onset is more rapid in Africa.[3][4] In India, cases may also occur in those who have not been diagnosed with VL and these people are infectious for the Leishmania donovani parasite, thus potentially perpetuating the disease.[3] Diagnosis is usually based on symptoms.[2] The underlying mechanism is believed to involve an immune reaction.[2]
Treatment is often with miltefosine, sodium stibogluconate or amphotericin B; though in Sudan it may resolve on their own.[2][3] These medications are taken for months.[3] Following treatment a long time is required for the skin to return to normal.[1]
PKDL mainly occurs in Sudan and India, areas affected by Leishmania donovani.[2] It occurs in between 2.5 and 20% of people who have had VL.[3] Adults and children are affected with similar frequency.[5] It was first described in 1922 by Sir Upendranath Brahmachari, who called it dermal leishmanoid.[4][6]
Signs and symptoms
The presentation is consistent with:[4][7]
- Hypopigmented patches
- Erythematous succulent papulo-plaques
- Nodular lesions
- Photosensitivity
- Verrucous
- Xanthomatous
- Ulcerative lesions
 Presentation of PKDL with prominent skin and mucosal lesions
Presentation of PKDL with prominent skin and mucosal lesions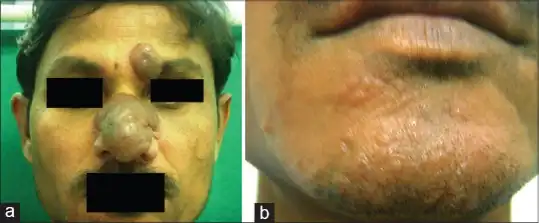 a) Image shows erythematous lobulated nodules b) hypopigmented plaque on chin
a) Image shows erythematous lobulated nodules b) hypopigmented plaque on chin Hypopigmented papules are seen on the patient's back. The lesions are roughly symmetrical, a common characteristic of post-kala-azar dermal leishmaniasis (PKDL), and are painless and non- pruritic.
Hypopigmented papules are seen on the patient's back. The lesions are roughly symmetrical, a common characteristic of post-kala-azar dermal leishmaniasis (PKDL), and are painless and non- pruritic.
Cause
The cause is uncertain. The possible reasons Post-kala-azar dermal leishmaniasis occurs include:[8][3]
- Use of antimonial drugs
- Sunburn
- Reinfection with kala-azar
- Memory T cell responses failing in certain organs
- Genetic susceptibility
Mechanism
There is increasing evidence that the pathogenesis is largely immunologically mediated; high concentrations of interleukin 10 in the peripheral blood of VL patients predict the development of PKDL. During VL, interferon gamma is not produced by peripheral blood mononuclear cells. [8][9][10]
After treatment of VL, PBMCs start producing interferon gamma, which coincides with the appearance of PKDL lesions due to interferon-gamma-producing cells causing skin inflammation as a reaction to persisting parasites in the skin.[10][8][9]
Diagnosis

Post-kala-azar dermal leishmaniasis is difficult to diagnose.[11]
Diagnosis is mainly clinical, but parasites can be seen by microscopy in smears with limited sensitivity.[11] PCR and monoclonal antibodies may detect parasites in a high percentage of cases. Serological tests and the leishmanin skin test are of limited value.[12][13][14]
Differential diagnosis
The DDX of the condition Post-kala-azar dermal leishmaniasis is as follows:[4]
- Lepromatous leprosy
- Lepromatous leprosy, xanthoma
- Systemic lupus erythematosus
- Lepromatous leprosy, sarcoidosis
Treatment
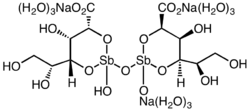
Treatment is always needed in Indian PKDL; in Sudan, most cases are self-limited but severe and chronic cases are treated. Sodium stibogluconate is given at 20 mg/kg for 2 months in Sudan and for 4 months in India.However a recent article by Datta et al, indicated "sodium stibogluconate is being discouraged because of multiple documented reports of treatment failure "[15] Liposomal amphotericine B seems effective, although research has brought many new insights in pathogenesis and management of PKDL, several issues in particular in relation to control remain unsolved and deserve urgent attention.[15][16]
Miltefosine is the only available oral medication available for VL and PKDL.[17] While the drug works for short term treatment of VL, PKDL would require a longer treatment of more than 28 days with this drug.[17]
Miltefosine is not recommended for use as a monotherapy to treat PKDL.[17]
Epidemiology
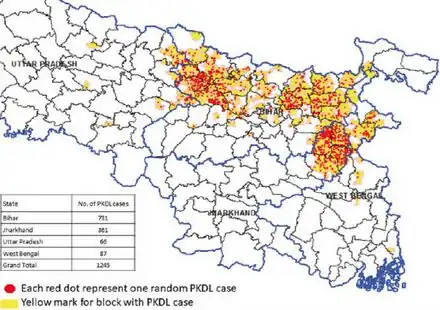
Post-kala-azar dermal leishmaniasis occurs in the following south eastern Asian countries:[18]
- India -75%
- Bangladesh -7%
- Nepal -1%
- Sudan -9%
- Ethiopia -1%
- South Sudan-8%
- Bangladesh -7%
Furthermore, cases for Post-kala-azar dermal leishmaniasis have also been witnessed in: [18]
- Iran
- Brazil
- China
- Japan
Society and culture
People with PKDL are a reservoir of leishmaniasis.[19] To eliminate leishmaniasis from a population, people with PKDL must get treatment.[19] The government of India has an kala-azar elimination program ongoing which entered a consolidation phase in 2017.[20]
The Indian medical practitioner Upendra Nath Brahmachari was nominated for the Nobel Prize in Physiology or Medicine in 1929 for his discovery of ureastibamine (an antimonial compound for the treatment of kala-azar) and a new disease, post kala-azar dermal leishmaniasis.[21]
See also
References
- 1 2 Tan, Cheng; Zhu, Wen-Yuan (1 January 2023). Atlas of Pigmentary Skin Disorders. Springer Nature. p. 76. ISBN 978-981-19-5634-8. Archived from the original on 15 July 2023. Retrieved 14 July 2023.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Passeron, Thierry; Ortonne, Jean-Paul (2016). "Kala-azar". Atlas of Pigmentary Disorders. Switzerland: Springer. p. 144. ISBN 978-3-319-10897-1. Archived from the original on 12 July 2023. Retrieved 11 July 2023.
- 1 2 3 4 5 6 7 8 9 Gedda, MR; Singh, B; Kumar, D; Singh, AK; Madhukar, P; Upadhyay, S; Singh, OP; Sundar, S (July 2020). "Post kala-azar dermal leishmaniasis: A threat to elimination program". PLoS neglected tropical diseases. 14 (7): e0008221. doi:10.1371/journal.pntd.0008221. PMID 32614818.
- 1 2 3 4 5 6 Kumar, Piyush; Chatterjee, Mitali; Das, Nilay Kanti (2021). "Post Kala-Azar Dermal Leishmaniasis: Clinical Features and Differential Diagnosis". Indian Journal of Dermatology. 66 (1): 24–33. doi:10.4103/ijd.IJD_602_20. ISSN 0019-5154. PMC 8061484. PMID 33911290.
- ↑ Pathania, Y S; Budania, A (5 January 2022). "Post-kala-azar dermal leishmaniasis". QJM: An International Journal of Medicine. 114 (11): 824–825. doi:10.1093/qjmed/hcab236.
- ↑ Brahmachari, U. N. (April 1922). "A New Form of Cutaneous Leishmaniasis—Dermal Leishmanoid". The Indian Medical Gazette. 57 (4): 125–127. ISSN 0019-5863. PMC 5186533. PMID 29008368.
- ↑ Prevention, CDC-Centers for Disease Control and (13 June 2023). "CDC - Leishmaniasis - Resources for Health Professionals". www.cdc.gov. Archived from the original on 23 April 2023. Retrieved 15 July 2023.
- 1 2 3 Mukhopadhyay, Debanjan; Dalton, Jane E.; Kaye, Paul M.; Chatterjee, Mitali (February 2014). "Post kala-azar dermal leishmaniasis: an unresolved mystery". Trends in Parasitology. 30 (2): 65–74. doi:10.1016/j.pt.2013.12.004. PMC 3919212. PMID 24388776.
- 1 2 Haldar, J P; Ghose, S; Saha, K C; Ghose, A C (November 1983). "Cell-mediated immune response in Indian kala-azar and post-kala-azar dermal leishmaniasis". Infection and Immunity. 42 (2): 702–707. doi:10.1128/iai.42.2.702-707.1983. ISSN 0019-9567. PMC 264486. PMID 6642649.
- 1 2 Volpedo, G; Pacheco-Fernandez, T; Holcomb, EA; Cipriano, N; Cox, B; Satoskar, AR (2021). "Mechanisms of Immunopathogenesis in Cutaneous Leishmaniasis And Post Kala-azar Dermal Leishmaniasis (PKDL)". Frontiers in Cellular and Infection Microbiology. 11: 685296. doi:10.3389/fcimb.2021.685296. PMC 8217655. PMID 34169006.
- 1 2 Zijlstra, EE (2019). "Biomarkers in Post-kala-azar Dermal Leishmaniasis". Frontiers in Cellular and Infection Microbiology. 9: 228. doi:10.3389/fcimb.2019.00228. PMC 6685405. PMID 31417876.
- ↑ Dixit, KK; Singh, R; Salotra, P (November 2020). "Advancement in Molecular Diagnosis of Post Kala-Azar Dermal Leishmaniasis". Indian Journal of Dermatology. 65 (6): 465–472. doi:10.4103/ijd.IJD_311_19 (inactive 2023-07-13). PMC 7810074. PMID 33487701.
{{cite journal}}: CS1 maint: DOI inactive as of July 2023 (link) - ↑ Bhandare, P; Shukla, P; Bhobe, M; Pai, VV (December 2014). "Post-kala-Azar dermal leishmaniasis: A diagnostic dilemma in a nonendemic area". Indian Dermatology Online Journal. 5 (Suppl 2): S122-4. doi:10.4103/2229-5178.146190. PMC 4290175. PMID 25593802.
- ↑ Zijlstra, Ee; Musa, Am; Khalil, Eag; El Hassan, Im; El-Hassan, Am (February 2003). "Post-kala-azar dermal leishmaniasis". The Lancet Infectious Diseases. 3 (2): 87–98. doi:10.1016/S1473-3099(03)00517-6. Archived from the original on 20 November 2022. Retrieved 16 July 2023.
- 1 2 Datta, Adrija; Podder, Indrashis; Das, Anupam; Sil, Amrita; Das, Nilay Kanti (2021). "Therapeutic Modalities in Post Kala-azar Dermal Leishmaniasis: A Systematic Review of the Effectiveness and Safety of the Treatment Options". Indian Journal of Dermatology. 66 (1): 34–43. doi:10.4103/ijd.IJD_264_20. ISSN 1998-3611. Archived from the original on 17 June 2022. Retrieved 15 July 2023.
- ↑ "Post-kala-azar dermal leishmaniasis: a manual for case management and control". www.who.int. Archived from the original on 20 January 2022. Retrieved 10 July 2023.
- 1 2 3 Pijpers, J; den Boer, ML; Essink, DR; Ritmeijer, K (February 2019). "The safety and efficacy of miltefosine in the long-term treatment of post-kala-azar dermal leishmaniasis in South Asia - A review and meta-analysis". PLOS Neglected Tropical Diseases. 13 (2): e0007173. doi:10.1371/journal.pntd.0007173. PMC 6386412. PMID 30742620.
- 1 2 Ghosh, Pramit; Roy, Pritam; Chaudhuri, Surya Jyati; Das, Nilay Kanti (2021). "Epidemiology of Post-Kala-azar Dermal Leishmaniasis". Indian Journal of Dermatology. 66 (1): 12–23. doi:10.4103/ijd.IJD_651_20. ISSN 1998-3611. PMC 8061485. PMID 33911289.
- 1 2 Ganguly, S; Das, NK; Barbhuiya, JN; Chatterjee, M (August 2010). "Post-kala-azar dermal leishmaniasis--an overview". International Journal of Dermatology. 49 (8): 921–31. doi:10.1111/j.1365-4632.2010.04558.x. PMID 21128917. S2CID 23294429.
- ↑ Zijlstra, EE; Alves, F; Rijal, S; Arana, B; Alvar, J (November 2017). "Post-kala-azar dermal leishmaniasis in the Indian subcontinent: A threat to the South-East Asia Region Kala-azar Elimination Programme". PLOS Neglected Tropical Diseases. 11 (11): e0005877. doi:10.1371/journal.pntd.0005877. PMC 5689828. PMID 29145397.
- ↑ Nobel Foundation (2008).The Nomination Database for the Nobel Prize in Physiology or Medicine, 1901-1951 Archived 2016-05-08 at the Wayback Machine