Proton therapy
| Proton therapy | |
|---|---|
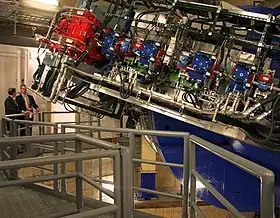 Proton therapy equipment at the Mayo Clinic in Rochester, Minnesota | |
| Other names | Proton beam therapy |
| ICD-10-PCS | Z92.3 |
In the field of medical treatment, proton therapy, or proton radiotherapy, is a type of particle therapy that uses a beam of protons to irradiate diseased tissue, most often to treat cancer. The chief advantage of proton therapy over other types of external beam radiotherapy (e.g., radiation therapy) is that the dose of protons is deposited over a narrow range of depth, which results in minimal entry, exit, or scattered radiation dose to healthy nearby tissues.
When evaluating whether to treat a tumor with photon or proton therapy, physicians may choose proton therapy if it is important to deliver a higher radiation dose to targeted tissues while significantly decreasing radiation to nearby organs at risk.[1] The American Society for Radiation Oncology Model Policy for Proton Beam therapy states that proton therapy is considered reasonable in instances where sparing the surrounding normal tissue "cannot be adequately achieved with photon-based radiotherapy" and can benefit the patient.[2] Like photon radiation therapy, proton therapy is often used in conjunction with surgery and/or chemotherapy to most effectively treat cancer.
Description
Proton therapy is a type of external beam radiotherapy that uses ionizing radiation. In proton therapy, medical personnel use a particle accelerator to target a tumor with a beam of protons.[4][5] These charged particles damage the DNA of cells, ultimately killing them by stopping their reproduction and thereby eliminating the tumor. Cancerous cells are particularly vulnerable to attacks on DNA because of their high rate of division and their limited abilities to repair DNA damage. Some cancers with specific defects in DNA repair may be more sensitive to proton radiation.[6]
Proton therapy offers physicians the ability to deliver a highly conformal beam, i.e., delivering radiation that conforms to the shape and depth of the tumor and sparing much of the surrounding, normal tissue.[7] For example, when comparing proton therapy to the most advanced types of photon therapy—intensity-modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT)—proton therapy can deliver similar or higher radiation doses to the tumor with a 50%-60% lower total body radiation dose.[8][1]
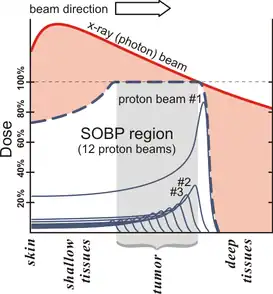
Protons have the ability to focus energy delivery to conform to the tumor shape, delivering only low-dose radiation to surrounding tissue. As a result, the patient experiences fewer side effects. All protons of a given energy have a certain penetration range; very few protons penetrate beyond that distance.[9] Furthermore, the dose delivered to tissue is maximized only over the last few millimeters of the particle's range; this maximum is called the spread out Bragg peak, often referred to as the SOBP (see visual).[10]
To treat tumors at greater depths, the proton accelerator must produce a beam with higher energy, typically given in eV (electron volts). Accelerators used for proton therapy typically produce protons with energies in the range of 70 to 250 MeV. Adjusting proton energy during the treatment maximizes the cell damage the proton beam causes within the tumor. Tissue closer to the surface of the body than the tumor receives reduced radiation, and therefore reduced damage. Tissues deeper in the body receive very few protons, so the dosage becomes immeasurably small.[9]
In most treatments, protons of different energies with Bragg peaks at different depths are applied to treat the entire tumor. These Bragg peaks are shown as thin blue lines in the figure in this section. It is important to understand that, while tissues behind (or deeper than) the tumor receive almost no radiation from proton therapy, the tissues in front of (shallower than) the tumor receive radiation dosage based on the SOBP.
Equipment
Most installed proton therapy systems utilise isochronous cyclotrons.[11][12] Cyclotrons are considered simple to operate, reliable and can be made compact, especially with the use of superconducting magnets.[13] Synchrotrons can also be used, with the advantage of easier production at varying energies.[14] Linear accelerators, as used for photon radiation therapy, are becoming commercially available as limitations of size and cost are resolved.[15] Modern proton systems incorporate high-quality imaging for daily assessment of tumor contours, treatment planning software illustrating 3D dose distributions, and various system configurations, e.g. multiple treatment rooms connected to one accelerator. Partly because of these advancements in technology, and partly because of the continually increasing amount of proton clinical data, the number of hospitals offering proton therapy continues to increase.
FLASH radiotherapy is a technique under development for photon and proton treatments, utilising very high dose rates (necessitating large beam currents). If applied clinically, it could shorten treatment time to just one to three one-second sessions, while further reducing side effects.[16][17][18]
History
The first suggestion that energetic protons could be an effective treatment method was made by Robert R. Wilson[19] in a paper published in 1946 while he was involved in the design of the Harvard Cyclotron Laboratory (HCL).[20] The first treatments were performed with particle accelerators built for physics research, notably Berkeley Radiation Laboratory in 1954 and at Uppsala in Sweden in 1957. In 1961, a collaboration began between HCL and the Massachusetts General Hospital (MGH) to pursue proton therapy. Over the next 41 years, this program refined and expanded these techniques while treating 9,116 patients[21] before the cyclotron was shut down in 2002. In the USSR a therapeutic proton beam with energies up to 200 MeV was obtained at the synchrocyclotron of the JINR in Dubna in 1967. The ITEP center in Moscow, Russia, which began treating patients in 1969, is the oldest proton center still in operation. The Paul Scherrer Institute in Switzerland was the world's first proton center to treat ocular tumors beginning in 1984. In addition, they invented pencil beam scanning in 1996, which is now the state-of-the art form of proton therapy. [22]
The world's first hospital-based proton therapy center was a low energy cyclotron centre for ocular tumours at the Clatterbridge Centre for Oncology in the UK, opened in 1989,[23] followed in 1990 at the Loma Linda University Medical Center (LLUMC) in Loma Linda, California. Later, the Northeast Proton Therapy Center at Massachusetts General Hospital was brought online, and the HCL treatment program was transferred to it during 2001 and 2002. At the beginning of 2020, there were 37 proton therapy centers in the United States alone,[24] and a total of 89 worldwide.[25] As of 2020, five manufacturers make proton therapy systems: Mevion Medical Systems, Ion Beam Applications, Hitachi, ProTom International and Varian Medical Systems.
Types of proton therapy
The newest form of proton therapy, pencil beam scanning, delivers therapy by sweeping a proton beam laterally over the target so that it delivers the required dose while closely conforming to shape of the targeted tumor. Prior to the use of pencil beam scanning, oncologists used a scattering method to direct a wide beam toward the tumor. [26]
Passive scattering beam delivery
The first commercially available proton delivery systems used a scattering process, also known as passive scattering, to deliver the therapy. With scattering proton therapy the proton beam is spread out by scattering devices, and the beam is then shaped by placing items such as collimators and compensators into the path of the protons.[27] Passive scattering delivers homogenous dose along the target volume. Consequently, passive scattering provides more limited control over dose distributions proximal to the target. Over time many scattering therapy systems have been upgraded to deliver pencil beam scanning. However, because scattering therapy was the first type of proton therapy available, most clinical data available on proton therapy—especially long-term data as of 2020—were acquired via scattering technology.
Pencil beam scanning beam delivery
A newer and more flexible delivery method for proton therapy is pencil beam scanning, using a beam that sweeps laterally over the target so that it delivers the required dose while closely conforming to shape of the targeted tumor. This conformal delivery is achieved by shaping the dose through magnetic scanning of thin beamlets of protons without the need for apertures and compensators. Multiple beams are delivered from different directions, and magnets in the treatment nozzle steer the proton beam to conform to the target volume layer as the dose is painted layer by layer. This type of scanning delivery provides greater flexibility and control, allowing the proton dose to conform more precisely to the shape of the tumor.[27]
Delivery of protons via pencil beam scanning, which has been in use since 1996 at the Paul Scherrer Institute,[27] allows for the most precise type of proton delivery known as intensity-modulated proton therapy (IMPT). IMPT is to proton therapy what IMRT is to conventional photon therapy—treatment that more closely conforms to the target tumor while avoiding surrounding structures.[28] Virtually all new proton systems now provide pencil beam scanning exclusively. A study led by Memorial Sloan Kettering Cancer Center suggests that IMPT can improve local control when compared to passive scattering for patients with nasal cavity and paranasal sinus malignancies.[29]
Application
It was estimated that by the end of 2019, a total of ~200,000 patients had been treated with proton therapy. Physicians use protons to treat conditions in two broad categories:
- Disease sites that respond well to higher doses of radiation, i.e., dose escalation. In some instances, dose escalation has demonstrated a higher probability of "cure" (i.e., local control) than conventional radiotherapy.[30] These include, among others, uveal melanoma (ocular tumors), skull base and paraspinal tumors (chondrosarcoma and chordoma), and unresectable sarcomas. In all these cases proton therapy achieves significant improvements in the probability of local control over conventional radiotherapy.[31][32][33] In treatment of ocular tumors, proton therapy also has high rates of maintaining the natural eye.[34]
- Treatments where proton therapy's increased precision reduces unwanted side effects by lessening the dose to normal tissue. In these cases, the tumor dose is the same as in conventional therapy, so there is no expectation of an increased probability of curing the disease. Instead, the emphasis is on reducing the integral dose to normal tissue, thus reducing unwanted effects.[30]
Two prominent examples are pediatric neoplasms (such as medulloblastoma) and prostate cancer.
Pediatric treatments
Irreversible long-term side effects of conventional radiation therapy for pediatric cancers have been well documented and include growth disorders, neurocognitive toxicity, ototoxicity with subsequent effects on learning and language development, and renal, endocrine and gonadal dysfunctions. Radiation-induced secondary malignancy is another very serious adverse effect that has been reported. As there is minimal exit dose when using proton radiation therapy, the dose to surrounding normal tissues can be significantly limited, reducing the acute toxicity which positively impacts the risk for these long-term side effects. Cancers requiring craniospinal irradiation, for example, benefit from the absence of exit dose with proton therapy: dose to the heart, mediastinum, bowel, bladder and other tissues anterior to the vertebrae is eliminated, resulting in a reduction of acute thoracic, gastrointestinal and bladder side effects.[35][36][37]
Eye tumors
Proton therapy for ocular (eye) tumors is a special case since this treatment requires only comparatively low energy protons (about 70 MeV). Owing to this low energy requirement, some particle therapy centers only treat ocular tumors.[21] Proton, or more generally, hadron therapy of tissue close to the eye affords sophisticated methods to assess the alignment of the eye that can vary significantly from other patient position verification approaches in image guided particle therapy.[38] Position verification and correction must ensure that the radiation spares sensitive tissue like the optic nerve to preserve the patient's vision.
For ocular tumors, selecting the type of radiotherapy depends on tumor location and extent, tumor radioresistance (calculating the dose needed to eliminate the tumor), and the radiotherapy's potential toxic side effects of nearby critical structures.[39] For example, proton therapy is an option for retinoblastoma [40] and intraocular melanoma.[41] The advantage of using a proton beam is that it has the potential to effectively treat the tumor while sparing sensitive structures of the eye.[42] Given its effectiveness, proton therapy has been described as the "gold standard" treatment for ocular melanomas.[43][44]
Base of skull cancer
When receiving radiation for skull base tumors, side effects of the radiation can include pituitary hormone dysfunction and visual field deficit—after radiation for pituitary tumors—as well as cranial neuropathy (nerve damage), radiation-induced osteosarcomas (bone cancer), and osteoradionecrosis, which occurs when radiation causes part of the bone in the jaw or skull base to die.[45] Proton therapy has been very effective for people with base of skull tumors.[46] Unlike conventional photon radiation, protons do not penetrate beyond the tumor. Proton therapy lowers the risk of treatment-related side effects caused when healthy tissue receives radiation. Clinical studies have found proton therapy to be effective for skull base tumors.[47][48][49]
Head and neck tumors
Proton particles do not deposit exit dose, which allows proton therapy to spare normal tissues distal to the tumor target. This is particularly useful for treating head and neck tumors because of the anatomic constraints encountered in nearly all cancers in this region. The dosimetric advantage unique to proton therapy translates into toxicity reduction. For recurrent head and neck cancer requiring reirradiation, proton therapy is able to maximize a focused dose of radiation to the tumor while minimizing dose to surrounding tissues which results in a minimal acute toxicity profile, even in patients who have received multiple prior courses of radiotherapy.[50]
Left-sided breast cancer
When breast cancer — especially cancer in the left breast — is treated with conventional radiation, the lung and heart, which are near the left breast, are particularly susceptible to photon radiation damage. Such damage can eventually cause lung problems (e.g., lung cancer) or various heart problems. Depending on the location of the tumor, damage can also occur to the esophagus, or to the chest wall (which can potentially lead to leukemia).[51] One recent study revealed that proton therapy has low rates of toxicity to nearby healthy tissues and similar rates of disease control compared with conventional radiation.[52] Other researchers found that proton pencil beam scanning techniques can reduce both the mean heart dose and the internal mammary node dose to essentially zero.[53]
Small studies have found that, compared to conventional photon radiation, proton therapy delivers minimal toxic dose to healthy tissues[54] and specifically decreased dose to the heart and lung.[55] Large-scale trials are underway to examine other potential benefits of proton therapy to treat breast cancer.[56]
Lymphoma (Tumors of lymphoid tissue)
Although chemotherapy is the primary treatment for patients with lymphoma, consolidative radiation is often used in Hodgkin lymphoma and aggressive non-Hodgkin lymphoma, while definitive treatment with radiation alone is used in a small fraction of lymphoma patients. Unfortunately, treatment-related toxicities caused by chemotherapy agents and radiation exposure to healthy tissues are major concerns for lymphoma survivors. Advanced radiation therapy technologies such as proton therapy may offer significant and clinically relevant advantages such as sparing important organs at risk and decreasing the risk for late normal tissue damage while still achieving the primary goal of disease control. This is especially important for lymphoma patients who are being treated with curative intent and have long life expectancies following therapy.[57]
Prostate cancer
In prostate cancer cases, the issue is less clear. Some published studies found a reduction in long term rectal and genito-urinary damage when treating with protons rather than photons (meaning X-ray or gamma ray therapy). Others showed a small difference, limited to cases where the prostate is particularly close to certain anatomical structures.[58][59] The relatively small improvement found may be the result of inconsistent patient set-up and internal organ movement during treatment, which offsets most of the advantage of increased precision.[59][60][61] One source suggests that dose errors around 20% can result from motion errors of just 2.5 mm (0.098 in). and another that prostate motion is between 5–10 mm (0.20–0.39 in).[62]
However, the number of cases of prostate cancer diagnosed each year far exceeds those of the other diseases referred to above, and this has led some, but not all, facilities to devote a majority of their treatment slots to prostate treatments. For example, two hospital facilities devote roughly 65%[63] and 50%[64] of their proton treatment capacity to prostate cancer, while a third devotes only 7.1%.[65]
Overall worldwide numbers are hard to compile, but one example states that in 2003 roughly 26% of proton therapy treatments worldwide were for prostate cancer.[66]
Gastrointestinal malignancy
An increasing amount of data has shown that proton therapy has great potential to increase therapeutic tolerance for patients with GI malignancies. The possibility of decreasing radiation dose to organs at risk may also help facilitate chemotherapy dose escalation or allow for new chemotherapy combinations. Proton therapy will play a decisive role in the context of ongoing intensified combined modality treatments for GI cancers. The following review presents the benefits of proton therapy in treating hepatocellular carcinoma, pancreatic cancer and esophageal cancer.[67]
Hepatocellular carcinoma
Post-treatment liver decompensation, and subsequent liver failure, is a risk when delivering radiotherapy for hepatocellular carcinoma, the most common type of primary liver cancer. Research shows that use of proton therapy results in favorable results related to local tumor control, progression-free survival, and overall survival.[68][69][70][71] Other studies, which examined proton therapy compared with conventional photon therapy, show that proton therapy is associated with improved survival and/or fewer side effects; therefore proton therapy has the potential to significantly improve clinical outcomes for some patients with liver cancer.[72][73]
Reirradiation for recurrent cancer
For patients who develop local or regional recurrences after their initial radiation therapy, physicians are limited in their treatment options due to their reluctance to deliver additional photon radiation therapy to tissues that have already been irradiated. Re-irradiation is a potentially curative treatment option for patients with locally recurrent head and neck cancer. In particular, pencil beam scanning may be ideally suited for reirradiation.[74] Research has shown the feasibility of using proton therapy with acceptable side effects, even in patients who have had multiple prior courses of photon radiation.[75][76][77]
Comparison with other treatments
A large study on comparative effectiveness of proton therapy was published by teams of the University of Pennsylvania and Washington University in St. Louis in JAMA Oncology, assessing whether proton therapy in the setting of concurrent chemoradiotherapy is associated with fewer 90-day unplanned hospitalizations and overall survival compared with concurrent photon therapy and chemoradiotherapy.[78] The study included 1483 adult patients with nonmetastatic, locally advanced cancer treated with concurrent chemoradiotherapy with curative intent and concluded that 'proton chemoradiotherapy was associated with significantly reduced acute adverse events that caused unplanned hospitalizations, with similar disease-free and overall survival'. A significant number of randomized controlled trials is currently recruiting, but only a limited number have been completed to date (August 2020). A phase III randomized controlled trial of proton beam therapy versus radiofrequency ablation (RFA) for recurrent hepatocellular carcinoma organized by the National Cancer Center in Korea showed better 2-year local progression free survival for the proton arm and concluded that proton beam therapy (PBT) is 'not inferior to RFA in terms of local progression-free survival and safety, denoting that either RFA or PBT can be applied to recurrent small HCC patients'.[68] A phase IIB randomized controlled trial of proton beam therapy versus IMRT for locally advanced esophageal cancer organized by the University of Texas MD Anderson Cancer Center concluded that proton beam therapy reduced the risk and severity of adverse events compared with IMRT while maintaining similar Progression Free Survival.[79] Another Phase II Randomized Controlled Trial comparing photons versus protons for Glioblastoma concluded that patients at risk of severe lymphopenia could benefit from proton therapy.[80] A team from Stanford University assessed the risk of secondary cancer after primary cancer treatment with external beam radiation using data from the National Cancer Database from 9 tumor types: head and neck, gastrointestinal, gynecologic, lymphoma, lung, prostate, breast, bone/soft tissue, and brain/central nervous system.[81] The study included a total of 450,373 patients and concluded that proton therapy was associated with a lower risk of second cancer.
The issue of when, whether, and how best to apply this technology is still under discussion by physicians and researchers. One recently introduced method called 'model-based selection' uses comparative treatment plans for IMRT and IMPT in combination with normal tissue complication probability (NTCP) models to identify patients that may benefit most from proton therapy.[82][83]
Clinical trials are underway to examine the comparative efficacy of proton therapy (vs photon radiation) for the following:
- Pediatric cancers—by St. Jude Children's Research Hospital,[84] Samsung Medical Center [85]
- Base of skull cancer—by Heidelberg University [86]
- Head and neck cancer—by MD Anderson,[87] Memorial Sloan Kettering and other centers[88]
- Brain and spinal cord cancer—by Massachusetts General Hospital,[89] Uppsala University and other centers,[90] NRG Oncology[91][92]
- Hepatocellular carcinoma (liver)—by NRG Oncology,[93] Chang Gung Memorial Hospital,[94] Loma Linda University [95]
- Lung cancer—by Radiation Therapy Oncology Group (RTOG),[96] Proton Collaborative Group (PCG),[97] Mayo Clinic[98]
- Esophageal cancer—by NRG Oncology,[99] Abramson Cancer Center, University of Pennsylvania[100]
- Breast cancer—by University of Pennsylvania,[101] Proton Collaborative Group (PCG)[102]
- Pancreatic cancer—by University of Maryland,[103] Proton Collaborative Group (PCG)[104]
X-ray radiotherapy
_and_IMRT_(left).jpg.webp)
The figure at the right of the page shows how beams of X-rays (IMRT; left frame) and beams of protons (right frame), of different energies, penetrate human tissue. A tumor with a sizable thickness is covered by the IMRT spread out Bragg peak (SOBP) shown as the red lined distribution in the figure. The SOBP is an overlap of several pristine Bragg peaks (blue lines) at staggered depths.
Megavoltage X-ray therapy has less "skin scarring potential" than proton therapy: X-ray radiation at the skin, and at very small depths, is lower than for proton therapy. One study estimates that passively scattered proton fields have a slightly higher entrance dose at the skin (~75%) compared to therapeutic megavoltage (MeV) photon beams (~60%).[3] X-ray radiation dose falls off gradually, unnecessarily damaging tissue deeper in the body and damaging the skin and surface tissue opposite the beam entrance. The differences between the two methods depends on the:
- Width of the SOBP
- Depth of the tumor
- Number of beams that treat the tumor
The X-ray advantage of reduced damage to skin at the entrance is partially counteracted by damage to skin at the exit point.
Since X-ray treatments are usually done with multiple exposures from opposite sides, each section of skin is exposed to both entering and exiting X-rays. In proton therapy, skin exposure at the entrance point is higher, but tissues on the opposite side of the body to the tumor receive no radiation. Thus, X-ray therapy causes slightly less damage to the skin and surface tissues, and proton therapy causes less damage to deeper tissues in front of and beyond the target.[5]
An important consideration in comparing these treatments is whether the equipment delivers protons via the scattering method (historically, the most common) or a spot scanning method. Spot scanning can adjust the width of the SOBP on a spot-by-spot basis, which reduces the volume of normal (healthy) tissue inside the high dose region. Also, spot scanning allows for intensity modulated proton therapy (IMPT), which determines individual spot intensities using an optimization algorithm that lets the user balance the competing goals of irradiating tumors while sparing normal tissue. Spot scanning availability depends on the machine and the institution. Spot scanning is more commonly known as pencil-beam scanning and is available on IBA, Hitachi, Mevion (known as HYPERSCAN[105] which became US FDA approved in 2017) and Varian.
Surgery
Physicians base the decision to use surgery or proton therapy (or any radiation therapy) on the tumor type, stage, and location. In some instances, surgery is superior (such as cutaneous melanoma), in some instances radiation is superior (such as skull base chondrosarcoma), and in some instances they are comparable (for example, prostate cancer). In some instances, they are used together (e.g., rectal cancer or early stage breast cancer).
The benefit of external beam proton radiation lies in the dosimetric difference from external beam X-ray radiation and brachytherapy in cases where the use of radiation therapy is already indicated, rather than as a direct competition with surgery.[30] However, in the case of prostate cancer, the most common indication for proton beam therapy, no clinical study directly comparing proton therapy to surgery, brachytherapy, or other treatments has shown any clinical benefit for proton beam therapy. Indeed, the largest study to date showed that IMRT compared with proton therapy was associated with less gastrointestinal morbidity.[106]
Side effects and risks
Proton therapy is a type of external beam radiotherapy, and shares risks and side effects of other forms of radiation therapy. However the dose outside of the treatment region can be significantly less for deep-tissue tumors than X-ray therapy, because proton therapy takes full advantage of the Bragg peak. Proton therapy has been in use for over 40 years, and is a mature treatment technology. However, as with all medical knowledge, understanding of the interaction of radiation (proton, X-ray, etc.) with tumor and normal tissue is still imperfect.[107]
Costs
Historically, proton therapy has been expensive. An analysis published in 2003 determined the relative cost of proton therapy is approximately 2.4 times that of X-ray therapies.[108] Newer, less expensive, and dozens more proton treatment centers are driving costs down and they offer more accurate three-dimensional targeting. Higher proton dosage over fewer treatments sessions (1/3 fewer or less) is also driving costs down.[109][110] Thus the cost is expected to reduce as better proton technology becomes more widely available. An analysis published in 2005 determined that the cost of proton therapy is not unrealistic and should not be the reason for denying patients access to the technology.[111] In some clinical situations, proton beam therapy is clearly superior to the alternatives.[112][113]
A study in 2007 expressed concerns about the effectiveness of proton therapy for treating prostate cancer,[114] but with the advent of new developments in the technology, such as improved scanning techniques and more precise dose delivery ('pencil beam scanning'), this situation may change considerably.[115] Amitabh Chandra, a health economist at Harvard University, stated, "Proton-beam therapy is like the Death Star of American medical technology... It's a metaphor for all the problems we have in American medicine."[116] Proton therapy is cost-effective for some types of cancer, but not all.[117][118] In particular, some other treatments offer better overall value for treatment of prostate cancer.[117]
As of 2018, the cost of a single-room particle therapy system is US$40 million, with multi-room systems costing up to US$200 million.[119][120]
Treatment centers

As of August 2020, there are over 89 particle therapy facilities worldwide,[121] with at least 41 others under construction.[122] As of August 2020, there are 34 operational proton therapy centers in the United States. As of the end of 2015 more than 154,203 patients had been treated worldwide.[123]
One hindrance to universal use of the proton in cancer treatment is the size and cost of the cyclotron or synchrotron equipment necessary. Several industrial teams are working on development of comparatively small accelerator systems to deliver the proton therapy to patients.[124] Among the technologies being investigated are superconducting synchrocyclotrons (also known as FM Cyclotrons), ultra-compact synchrotrons, dielectric wall accelerators,[124] and linear particle accelerators.[110]
United States
Proton treatment centers in the United States as of 2020 (in chronological order of first treatment date) include:[23][125]
| Institution | Location | Year of first treatment | Comments |
|---|---|---|---|
| Loma Linda University Medical Center[126] | Loma Linda, CA | 1990 | First hospital-based facility in USA; uses Spread Out Bragg's Peak (SOBP) |
| Crocker Nuclear Laboratory[127] | Davis, CA | 1994 | Ocular treatments only (low energy accelerator); at University of California, Davis |
| Francis H. Burr Proton Center | Boston, MA | 2001 | At Massachusetts General Hospital and formerly known as NPTC; continuation of Harvard Cyclotron Laboratory/MGH treatment program that began in 1961; Manufactured by Ion Beam Applications[128] |
| University of Florida Health Proton Therapy Institute-Jacksonville[129] | Jacksonville, FL | 2006 | The UF Health Proton Therapy Institute is a part of a non-profit academic medical research facility affiliated with the University of Florida College of Medicine-Jacksonville. It is the first treatment center in the Southeast U.S. to offer proton therapy. Manufactured by Ion Beam Applications[128] |
| University of Texas MD Anderson Cancer Center[130] | Houston, TX | ||
| Oklahoma Proton Center[131] | Oklahoma City, OK | 2009 | 4 treatment rooms, Proteus PLUS system manufactured by Ion Beam Applications[128] |
| Northwestern Medicine Chicago Proton Center | Warrenville, IL | 2010 | 4 treatment rooms, Proteus PLUS system manufactured by Ion Beam Applications[128] |
| Roberts Proton Therapy Center[132] | Philadelphia, PA | The largest proton therapy center in the world, the Roberts Proton Therapy Center, which is a part of Penn's Abramson Cancer Center, University of Pennsylvania Health System; 5 treatment rooms, Proteus PLUS system manufactured by Ion Beam Applications[128] | |
| Hampton University Proton Therapy Institute | Hampton, VA | 5 treatment rooms, Proteus PLUS system manufactured by Ion Beam Applications[128] | |
| ProCure Proton Therapy Center[133] | Somerset, NJ | 2012 | 4 treatment rooms, Proteus PLUS system manufactured by Ion Beam Applications[128] |
| SCCA Proton Therapy Center | Seattle, WA | 2013 | At Seattle Cancer Care Alliance; part of Fred Hutchinson Cancer Research Center; 4 treatment rooms, Proteus PLUS system manufactured by Ion Beam Applications[128] |
| Siteman Cancer Center[109] | St. Louis, MO | First of the new single suite, ultra-compact, superconducting synchrocyclotron,[134] lower cost facilities to treat a patient using the Mevion Medical System's S250.[135] | |
| Provision Proton Therapy Center[136] | Knoxville, TN | 2014 | 3 treatment rooms, Proteus PLUS system manufactured by Ion Beam Applications[128] |
| California Protons Cancer Therapy Center[137] | San Diego, CA | 5 treatment rooms, manufactured by Varian Medical Systems[138] | |
| Ackerman Cancer Center | Jacksonville, FL | 2015 | Ackerman Cancer Center is the world's first private, physician-owned practice to provide proton therapy, in addition to conventional radiation therapy and on-site diagnostic services. |
| The Laurie Proton Therapy Center | New Brunswick, NJ | The Laurie Proton Therapy Center, part of Robert Wood Johnson University Hospital, is home to the world's third MEVION S250 Proton Therapy System. | |
| Texas Center for Proton Therapy | Dallas Fort Worth, TX | A collaboration by "Texas Oncology and The US Oncology Network, supported by McKesson Specialty Health, and Baylor Health Enterprises"; three pencil beam rooms and cone beam CT imaging.[139] 3 treatment rooms, Proteus PLUS system manufactured by Ion Beam Applications[128] | |
| Mayo Clinic Jacobson Building | Rochester, MN | 4 treatment rooms.[140] Manufactured by Hitachi.[141] | |
| St. Jude Red Frog Events Proton Therapy Center | Memphis, TN | 3 treatment rooms | |
| Mayo Clinic Cancer Center | Phoenix, AZ | 2016 | 4 treatment rooms.[142] Manufactured by Hitachi.[143] |
| The Marjorie and Leonard Williams Center for Proton Therapy | Orlando, FL | http://www.ufhealthcancerorlando.com/centers/proton-therapy-center | |
| Cancer and Blood Diseases Institute | Liberty Township, OH | Collaboration of University of Cincinnati Cancer Institute and Cincinnati Children's Hospital Medical Center,[144][145] manufactured by Varian Medical Systems | |
| Maryland Proton Treatment Center | Baltimore, MD | 5 treatment rooms, affiliated with the University of Maryland Greenebaum Comprehensive Cancer Center, manufactured by Varian Medical Systems. | |
| Proton Therapy Center at University Hospitals Seidman Cancer Center | Cleveland, OH | Only proton therapy center in Northern Ohio. One treatment room with the Mevion S250 Proton Therapy System. Part of the NCI-designated Case Comprehensive Cancer Center, University Hospitals Seidman Cancer Center is one of the nation's leading freestanding cancer hospitals. | |
| Miami Cancer Institute | Miami, FL | 2017 | 3 treatment rooms, all using pencil-beam scanning[146] Manufactured by Ion Beam Applications[128] |
| Beaumont Proton Therapy Center | Royal Oak, MI | Single treatment room, Proteus ONE system manufactured by Ion Beam Applications[128] | |
| Emory Proton Therapy Center | Atlanta, GA | 2018 | Five treatment rooms, ProBeam Superconducting Cyclotron[147] manufactured by Varian Medical Systems |
| Provision CARES Proton Therapy Center | Nashville, TN | Three treatment rooms, Two Gantries and One Fixed Beam, All Pencil Beam Scanning, manufactured by ProNova Solutions, LLC | |
| McLaren Proton Therapy Center | Flint, MI | The McLaren Proton Therapy System uses the industry's highest energy 330 MeV proton synchrotron to accelerate and deliver proton beam to two treatment rooms, with an opportunity to extend into a planned third room. Both operating treatment rooms are equipped with proton pencil beam scanning, cone beam computed tomography for image guidance, patient positioning system with 6-degrees of freedom that coupled with 180-degree partial gantry allows for complete flexibility of treatment angles. | |
| New York Proton Center | New York, NY | 2019 | A partnership between Memorial Sloan Kettering, Montefiore Health, and Mount Sinai Health System. 4 treatment rooms, manufactured by Varian Medical Systems |
| Johns Hopkins Proton Therapy Center | Washington, DC | 3 treatment rooms and 1 research gantry. Manufactured by Hitachi. | |
| South Florida Proton Therapy Institute | Delray Beach, FL | One treatment room, manufactured by Varian Medical Systems | |
| UAB Proton Therapy Center | Birmingham, AL | 2020 | One treatment room, manufactured by Varian Medical Systems |
| Dwoskin PTC - University of Miami | Miami, FL | One treatment room, manufactured by Varian Medical Systems | |
| The University of Kansas Cancer Center | Kansas City, KS | 2021 (Estimated) | Announced Feb 2019[148] |
| Penn Medicine Lancaster General Health Ann B. Barshinger Cancer Institute | Lancaster, PA | One treatment room, manufactured by Varian Medical Systems | |
| Penn Medicine Virtua Health | Voorhees, NJ | 2022 (Estimated) | One treatment room, manufactured by Varian Medical Systems |
| Mayo Clinic Florida | Jacksonville, FL | 2023 (Estimated) | Announced June 2019[149] |
| Ohio State, Nationwide Children's Hospital | Columbus, OH | Three treatment rooms, manufactured by Varian Medical Systems |
The Indiana University Health Proton Therapy Center in Bloomington, Indiana opened in 2004 and ceased operations in 2014.
Outside the US
| Institution | Maximum energy (MeV) | Year of first treatment | Location |
|---|---|---|---|
| Paul Scherrer Institute | 250 | 1984 | Villigen, Switzerland |
| Clatterbridge Cancer Centre NHS Foundation Trust, low-energy for ocular[150] | 62 | 1989 | Liverpool, United Kingdom |
| Centre de protonthérapie de l'Institut Curie | 235 | 1991 | Orsay, France |
| Centre Antoine Lacassagne | 63 | 1991 | Nice, France |
| Research Center for Charged Particle Therapy | 350–400 | 1994 | Chiba, Japan |
| TRIUMF[151] | 74 | 1995 | Vancouver, Canada |
| Helmholtz-Zentrum Berlin | 72 | 1998 | Berlin, Germany |
| Proton Medical Research Center University of Tsukuba | 250 | 2001 | Tsukuba, Japan |
| Centro di adroterapia oculare | 60 | 2002 | Catania, Italy |
| Wanjie Proton Therapy Center | 230 | 2004 | Zibo, China |
| Proton Therapy Center, Korea National Cancer Center | 230 | 2007 | Seoul, Korea |
| Heidelberg Ion-Beam Therapy Center (HIT) | 230 | 2009 | Heidelberg, Germany |
| Rinecker Proton Therapy Center | 250 | 2009 | Munich, Germany |
| Medipolis Proton Therapy and Research Center | 235 | 2011 | Kagoshima, Japan |
| Instytut Fizyki Jądrowej | 230 | 2011 | Kraków, Poland |
| Centro Nazionale di Adroterapia Oncologica | 250 | 2011 | Pavia, Italy |
| Protonové centrum v Praze (PTC, Prague) | 230 | 2012 | Prague, Czech Republic |
| Westdeutsches Protonentherapiezentrum Essen | 230 | 2013 | Essen, Germany |
| PTC Uniklinikum Dresden | 230 | 2014 | Dresden, Germany |
| Centro di Protonterapia, APSS Trento[152] | 230 | 2014 | Trento, Italy |
| Shanghai Proton and Heavy Ion Center | 230 | 2014 | Shanghai, China |
| Centrum Cyklotronowe Bronowice | 230 | 2015 | Kraków, Poland |
| SMC Proton Therapy Center | 230 | 2015 | Seoul, Korea |
| Proton and Radiation Therapy Center, Linkou Chang Gung Memorial Hospital | 230 | 2015 | Taipei, Taiwan |
| Yung-Ching Proton Center, Kaohsiung Chang Gung Memorial Hospital[153] | 230 | 2018 | Kaohsiung, Taiwan |
| Skandionkliniken[154] | 230 | 2015 | Uppsala, Sweden |
| A. Tsyb Medical Radiological Research Centre | 250 | 2016 | Obninsk, Russia |
| MedAustron | 250 | 2016 | Wiener Neustadt, Austria |
| Clinical Proton Therapy Center Dr. Berezin Medical Institute[155] | 250 | 2017 | Saint-Petersburg, Russia |
| Holland Proton Therapy Center[156] | 250 | 2018 | Delft, Netherlands |
| UMC Groningen Protonen Therapie Centrum[157] | 230 | 2018 | Groningen, Netherlands |
| The Christie[158] | 250 | 2018 | Manchester, United Kingdom |
| Danish Centre for Particle Therapy[159] | 250 | 2019 | Aarhus, Denmark |
| Apollo Proton Cancer Centre[160] | 230 | 2019 | Chennai, India |
| MAASTRO Clinic Proton Therapy[161] | 230 | 2019 | Maastricht, Netherlands |
| Clínica Universidad de Navarra | 230 | 2019 | Madrid, Spain |
| Centro de Protonterapia de Quirónsalud[162] | 230 | 2019 | Madrid, Spain |
| King Chulalongkorn Memorial Hospital [163] | 250 | 2021 | Bangkok, Thailand |
| University College London Hospitals[164] | 250 | 2021 | London, United Kingdom |
| Singapore Institute of Advanced Medicine[165] | 250 | 2021 | Singapore |
| Hefei Ion Medical Center[166] | 250 | 2021 | Hefei, China |
| Australian Bragg Centre for Proton Therapy & Research[167][168] | 330 | 2023–2025 | Adelaide, Australia |
Australia
In July 2020, construction began for "SAHMRI 2", the second building for the South Australian Health and Medical Research Institute. The building will house the Australian Bragg Centre for Proton Therapy & Research, a A$500+ million addition to the largest health and biomedical precinct in the Southern Hemisphere, Adelaide's BioMed City. The proton therapy unit is being supplied by ProTom International, which will install its Radiance 330 proton therapy system, the same system used at Massachusetts General Hospital. When in full operation, it will have the ability to treat approximately 600-700 patients per year with around half of these expected to be children and young adults. The facility is expected to be completed in late 2023, with its first patients treated in 2025.[168]
India
Apollo Proton Cancer Centre (APCC) in Chennai, Tamil Nadu, a unit under Apollo Hospitals, is a Cancer specialty hospital.[169] APCC is the only cancer hospital in India with Joint Commission International accreditation.[170]
Israel
In January 2020, it was announced that a proton therapy center would be built in Ichilov Hospital, at the Tel Aviv Sourasky Medical Center. The project's construction was fully funded by donations. It will have two treatment rooms.[171]
Spain
In October 2021, the Amancio Ortega Foundation arranged with the Spanish government and several autonomous communities to donate 280 million euros to install ten proton accelerators in the public health system.[172]
United Kingdom
In 2013 the British government announced that £250 million had been budgeted to establish two centers for advanced radiotherapy: The Christie NHS Foundation Trust ( the Christie Hospital) in Manchester, which opened in 2018, and University College London Hospitals NHS Foundation Trust, which opened in 2021. These offer high-energy proton therapy, as well as other types of advanced radiotherapy, including intensity-modulated radiotherapy (IMRT) and image-guided radiotherapy (IGRT).[173] In 2014, only low-energy proton therapy was available in the UK, at the Clatterbridge Cancer Centre NHS Foundation Trust in Merseyside. But NHS England has paid to have suitable cases treated abroad, mostly in the US. Such cases have risen from 18 in 2008 to 122 in 2013, 99 of whom were children. The cost to the National Health Service averaged around £100,000 per case.[174]
See also
- Particle therapy
- Charged particle therapy
- Hadron
- Microbeam
- Fast neutron therapy
- Boron neutron capture therapy
- Linear energy transfer
- Electromagnetic radiation and health
- Dosimetry
- Ionizing radiation
- List of oncology-related terms
References
- 1 2 Tai-Ze Yuan (2019). "New frontiers in proton therapy: applications in cancers". Cancer Commun. 39 (61): 61. doi:10.1186/s40880-019-0407-3. PMC 6805548. PMID 31640788.
- ↑ "PROTON BEAM THERAPY (PBT)" (PDF). astro.org. American Medical Association. 2013. Retrieved 1 February 2021.
- 1 2 Adapted, Levin W. P., Kooy H., Loeffler J. S., DeLaney T. F. (2005). "Proton Beam Therapy". British Journal of Cancer. 93 (8): 849–854. doi:10.1038/sj.bjc.6602754. PMC 2361650. PMID 16189526.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Jakel O (2007). "State of the Art in Hadron Therapy". AIP Conference Proceedings. 958 (1): 70–77. Bibcode:2007AIPC..958...70J. doi:10.1063/1.2825836.
- 1 2 "Zap! You're Not Dead". The Economist, 8 September 2007. 384 (8545):13–14.
- ↑ Liu Q (2015). "Lung Cancer Cell Line Screen Links Fanconi Anemia/BRCA Pathway Defects to Increased Relative Biological Effectiveness of Proton Radiation". Int J Radiation Oncol Biol Phys. 91 (5): 1081–1089. doi:10.1016/j.ijrobp.2014.12.046. PMID 25832698.
- ↑ Slater Jason M (2019). "Hypofractionated Proton Therapy in Early Prostate Cancer: Results of a Phase I/II Trial at Loma Linda University". Int J Particle Ther. 6 (1): 1–9. doi:10.14338/IJPT-19-00057. PMC 6871628. PMID 31773043.
- ↑ Kandula Shravan (2013). "Spot-scanning beam proton therapy vs intensity-modulated radiation therapy for ipsilateral head and neck malignancies: a treatment planning comparison". Med Dosim. 38 (4): 390–394. doi:10.1016/j.meddos.2013.05.001. PMID 23916884.
- 1 2 Metz, James (2006-07-31). "Differences Between Protons and X-rays". Abramson Cancer Center of the University of Pennsylvania. Archived from the original on 2008-12-17. Retrieved 2008-02-04.
the beam then stops, resulting in virtually no radiation to the tissue beyond the target – or no 'exit dose'
- ↑ Camphausen, K. A.; Lawrence, R. C. (2008). "Principles of Radiation Therapy". In Pazdur, R.; Wagman, L. D.; Camphausen, K. A.; Hoskins, W. J. (eds.) Cancer Management: A Multidisciplinary Approach. 11th ed. Archived 2013-10-04 at the Wayback Machine
- ↑ Smith, Alfred R. (26 January 2009). "Vision 20/20: Proton therapy". Medical Physics. 36 (2): 556–568. Bibcode:2009MedPh..36..556S. doi:10.1118/1.3058485. PMID 19291995. S2CID 1490932.
- ↑ Degiovanni, Alberto; Amaldi, Ugo (June 2015). "History of hadron therapy accelerators". Physica Medica. 31 (4): 322–332. doi:10.1016/j.ejmp.2015.03.002. PMID 25812487.
- ↑ Peach, K; Wilson, P; Jones, B (December 2011). "Accelerator science in medical physics". The British Journal of Radiology. 84 (special_issue_1): S4–S10. doi:10.1259/bjr/16022594. PMC 3473892. PMID 22374548.
- ↑ Liu, Hui; Chang, Joe Y. (5 May 2011). "Proton therapy in clinical practice". Chinese Journal of Cancer. 30 (5): 315–326. doi:10.5732/cjc.010.10529. PMC 4013396. PMID 21527064.
- ↑ Owen, Hywel; Lomax, Antony; Jolly, Simon (February 2016). "Current and future accelerator technologies for charged particle therapy". Nuclear Instruments and Methods in Physics Research Section A: Accelerators, Spectrometers, Detectors and Associated Equipment. 809: 96–104. Bibcode:2016NIMPA.809...96O. doi:10.1016/j.nima.2015.08.038.
- ↑ "FLASH radiotherapy with protons protects normal tissue while killing cancer". Physics World. 15 January 2020.
- ↑ Vozenin, M.-C.; Hendry, J.H.; Limoli, C.L. (July 2019). "Biological Benefits of Ultra-high Dose Rate FLASH Radiotherapy: Sleeping Beauty Awoken". Clinical Oncology. 31 (7): 407–415. doi:10.1016/j.clon.2019.04.001. PMC 6850216. PMID 31010708.
- ↑ Wilson, Joseph D.; Hammond, Ester M.; Higgins, Geoff S.; Petersson, Kristoffer (17 January 2020). "Ultra-High Dose Rate (FLASH) Radiotherapy: Silver Bullet or Fool's Gold?". Frontiers in Oncology. 9: 1563. doi:10.3389/fonc.2019.01563. PMC 6979639. PMID 32010633.
- ↑ "Radiological Use of Fast Protons", R. R. Wilson, Radiology, 47:487–91 (1946)
- ↑ Richard Wilson, A Brief History of the Harvard University Cyclotrons, Harvard University Press, 2004, p. 9
- 1 2 "PTCOG: Particle Therapy Co-Operative Group". Ptcog.web.psi.ch. Retrieved 2009-09-03.
- ↑ "Treating Cancer with Proton Therapy" (PDF). Paul Scherrer Institute. Retrieved 2020-08-01.
- 1 2 3 "Particle therapy facilities in operation". Particle Therapy Co-Operative Group. 2013-08-27. Retrieved 2014-09-01.
- ↑ "Proton Therapy Centers in the United States". Proton Beam Therapy. Retrieved 2020-08-01.
- ↑ "Particle therapy facilities in operation". Particle Therapy Co-Operative Group. Retrieved 2010-04-27.
- ↑ "ASTRO model policies PBT" (PDF). ASTRO. 2017-06-01. Retrieved 2020-08-01.
- 1 2 3 Radhe Mohan (2017). "Proton Therapy – Present and Future". Advanced Drug Delivery Reviews. 109: 26–44. doi:10.1016/j.addr.2016.11.006. PMC 5303653. PMID 27919760.
- ↑ Eric S Wisenbaugh (2014). "Proton Beam Therapy for Localized Prostate Cancer 101: Basics, Controversies, and Facts". Rev. Urol. 16.
- ↑ Ming Fan (2020). "Outcomes and Toxicities of Definitive Radiotherapy and Reirradiation Using 3-Dimensional Conformal or Intensity-Modulated (Pencil Beam) Proton Therapy for Patients With Nasal Cavity and Paranasal Sinus Malignancies". Cancer. 126 (9): 1905–1916. doi:10.1002/cncr.32776. PMC 7304541. PMID 32097507.
- 1 2 3 Levy, Richard P.; Blakely, Eleanor A.; et al. (March 2009). "The current status and future directions of heavy charged particle therapy in medicine". AIP Conference Proceedings. 1099 (410): 410–425. Bibcode:2009AIPC.1099..410L. doi:10.1063/1.3120064.
- ↑ Hug E. B.; et al. (1999). "Proton radiation therapy for chordomas and chondrosarcomas of the skull base". J. Neurosurg. 91 (3): 432–439. doi:10.3171/jns.1999.91.3.0432. PMID 10470818.
- ↑ Gragoudas, Evangelos; et al. (2002). "Evidence-based estimates of outcomes in patients treated for intraocular melenoma". Arch. Ophthalmol. 120 (12): 1665–1671. doi:10.1001/archopht.120.12.1665. PMID 12470140.
- ↑ Munzenrider J. E.; Liebsch N. J. (1999). "Proton radiotherapy for tumors of the skull base". Strahnlenther. Onkol. 175: 57–63. doi:10.1007/bf03038890. PMID 10394399. S2CID 34755628.
- ↑ "Proton Therapy for Ocular Tumors". ucsf.edu. Department of Radiation Oncology; University of California, San Francisco. Retrieved 2017-10-05.
- ↑ Lisa S Kahalley (2019). "Superior Intellectual Outcomes After Proton Radiotherapy Compared With Photon Radiotherapy for Pediatric Medulloblastoma". Journal of Clinical Oncology. 38 (5): 454–461. doi:10.1200/JCO.19.01706. PMC 7007288. PMID 31774710.
- ↑ Bree R Eaton (2016). "Endocrine outcomes with proton and photon radiotherapy for standard risk medulloblastoma". Neuro-Oncol. 18 (6): 881–7. doi:10.1093/neuonc/nov302. PMC 4864263. PMID 26688075.
- ↑ Christine E Hill-Kayser (2019). "Outcomes after Proton Therapy for Treatment of Pediatric High-Risk Neuroblastoma". International Journal of Radiation Oncology, Biology, Physics. 104 (2): 401–408. doi:10.1016/j.ijrobp.2019.01.095. PMID 30738983. S2CID 73417717.
- ↑ Selby, Boris Peter; et al. (2007). "Pose estimation of eyes for particle beam treatment of tumors". Bildverarbeitung für die Medizin (Medical Image Processing). Munich: Springer Berlin Heidelberg: 368–373.
- ↑ Juliette Thariat (2019). "Which irradiation technique for which ocular tumor". Acta Ophthalmologica. 97 (263). doi:10.1111/j.1755-3768.2019.8284.
- ↑ "Retinoblastoma Treatment". www.cancers.gov. 27 Aug 2020.
- ↑ "Treatment Options for Intraocular (Uveal) Melanoma". www.cancers.gove. 27 Aug 2020.
- ↑ Thanos Papakostas (2017). "Long-term Outcomes After Proton Beam Irradiation in Patients With Large Choroidal Melanomas". JAMA Ophthalmol. 135 (11): 1191–1196. doi:10.1001/jamaophthalmol.2017.3805. PMC 5710395. PMID 29049518.
- ↑ Kavita K Mishra (2016). "Proton therapy for the management of uveal melanoma and other ocular tumors". Chinese Clinical Oncology. 5 (4): 50. doi:10.21037/cco.2016.07.06. PMID 27558251.
- ↑ "Proton Therapy for Ocular Tumors". radonc.ucsf.edu. 27 Aug 2020.
- ↑ K J Stelzer (2000). "Acute and long-term complications of therapeutic radiation for skull base tumors". Neurosurg Clin N Am. 11 (4): 597–604. doi:10.1016/S1042-3680(18)30085-8. PMID 11082170.
- ↑ "Skull Base Tumors". www.mskcc.org. 27 Aug 2020.
- ↑ Maurizio Amichetti (2010). "A systematic review of proton therapy in the treatment of chondrosarcoma of the skull base". Neurosurg Rev. 33 (2): 155–165. doi:10.1007/s10143-009-0235-z. PMID 19921291. S2CID 10849293.
- ↑ Damien Weber (2016). "Long term outcomes of patients with skull-base low-grade chondrosarcoma and chordoma patients treated with pencil beam scanning proton therapy". Radiother Oncol. 120 (1): 169–174. doi:10.1016/j.radonc.2016.05.011. PMID 27247057.
- ↑ Jinpeng Zhou (2018). "Comparison of the Effectiveness of Radiotherapy with Photons and Particles for Chordoma After Surgery: A Meta-Analysis". World Neurosurg. 117: 46–53. doi:10.1016/j.wneu.2018.05.209. PMID 29879512.
- ↑ "TREATING HEAD AND NECK CARCINOMA WITH PROTON THERAPY". IBA White Paper. 2016-10-04.
- ↑ Zachary Brownlee (2018). "Late complications of radiation therapy for breast cancer: evolution in techniques and risk over time". Gland Surgery. 7 (4): 371–378. doi:10.21037/gs.2018.01.05. PMC 6107587. PMID 30175054.
- ↑ Rachel B. Jimenez (2019). "Phase II Study of Proton Beam Radiation Therapy for Patients With Breast Cancer Requiring Regional Nodal Irradiation". Journal of Clinical Oncology. 37 (30): 2778–2785. doi:10.1200/JCO.18.02366. PMC 7351324. PMID 31449469.
- ↑ Line B. Stick (2016). "Joint Estimation of Cardiac Toxicity and Recurrence Risks After Comprehensive Nodal Photon Versus Proton Therapy for Breast Cancer". International Journal of Radiation Oncology, Biology, Physics. 97 (4): 754–761. doi:10.1016/j.ijrobp.2016.12.008. PMC 5625081. PMID 28244411.
- ↑ David A Bush (2014). "Partial breast radiation therapy with proton beam: 5-year results with cosmetic outcomes". Int J Radiat Oncol Biol Phys. 90 (3): 501–505. doi:10.1016/j.ijrobp.2014.05.1308. PMID 25084608.
- ↑ Julie A Bradley (2015). "Initial Report of a Prospective Dosimetric and Clinical Feasibility Trial Demonstrates the Potential of Protons to Increase the Therapeutic Ratio in Breast Cancer Compared With Photons". Int J Radiat Oncol Biol Phys. 95 (5): 411–421. doi:10.1016/j.ijrobp.2015.09.018. PMID 26611875.
- ↑ "Pragmatic Randomized Trial of Proton vs. Photon Therapy for Patients With Non-Metastatic Breast Cancer: A Radiotherapy Comparative Effectiveness (RADCOMP) Consortium Trial". ClinicalTrials.gov. 21 August 2020.
- ↑ "TREATING HODGKIN AND NON-HODGKIN LYMPHOMA WITH PROTON THERAPY". IBA White Paper. September 2016.
- ↑ Slater, J. D.; et al. (2004). "Proton therapy for prostate cancer; the initial Loma Linda University experience". Int. J. Radiat. Oncol. Biol. Phys. 59 (2): 348–352. doi:10.1016/j.ijrobp.2003.10.011. PMID 15145147.
- 1 2 Zietman, A. L.; et al. (2005). "Comparisons of conventional-dose vs. high-dose conformal radiation therapy in clinically localized adenocarcinoma of the prostate: a randomized controlled trial". JAMA. 294 (10): 1233–1239. doi:10.1001/jama.294.10.1233. PMID 16160131.
- ↑ deCrevoisier, R.; et al. (2005). "Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy". Int. J. Radiat. Oncol. Biol. Phys. 62 (4): 965–973. doi:10.1016/j.ijrobp.2004.11.032. PMID 15989996.
- ↑ Lambert; et al. (2005). "Intrafractional motion during proton beam scanning". Phys. Med. Biol. 50 (20): 4853–4862. Bibcode:2005PMB....50.4853L. doi:10.1088/0031-9155/50/20/008. PMID 16204877.
- ↑ Byrne, Thomas E. (2005). "A Review of Prostate Motion with Considerations for the Treatment of Prostate Cancer". Medical Dosimerty. 30 (3): 155–161. doi:10.1016/j.meddos.2005.03.005. PMID 16112467.
- ↑ Van Dyk, Jacob (1999). The modern technology of radiation oncology: A Compendium for Medical Physicists and Radiation Oncologists. Medical Physics Publishing Corporation. p. 826. ISBN 978-0944838389.
Proton Patient Summary – Inception Through December 1998...Prostate...2591 64.3%
- ↑ "The Promise of Proton-Beam Therapy". U.S. News and World Report. 2008-04-16. Retrieved 2008-02-20.
- ↑ Delaney, T (2011). Francis H. Burr Proton Therapy Center (PDF of PowerPoint presentation). Massachusetts General Hospital; Harvard Medical School. Bibcode:2012ibt..book..597F – via Particle Therapy Co-Operative Group.
- ↑ Sisterson, Janet (December 2005). "Ion beam therapy in 2004". Nuclear Instruments and Methods in Physics Research Section B: Beam Interactions with Materials and Atoms. 241 (1–4): 713–716. Bibcode:2005NIMPB.241..713S. doi:10.1016/j.nimb.2005.07.121.
- ↑ "TREATING GASTROINTESTINAL MALIGNANCY WITH PROTON THERAPY". IBA White Paper. September 2016.
- 1 2 Tae Hyung Kim (2020). "Proton beam radiotherapy vs. radiofrequency ablation for recurrent hepatocellular carcinoma: a randomized phase III trial". Journal of Hepatology. 74 (3): 603–612. doi:10.1016/j.jhep.2020.09.026. PMID 33031846.
- ↑ Kuniaki Fuduka (2016). "Long-term outcomes of proton beam therapy in patients with previously untreated hepatocellular carcinoma". Cancer Science. 108 (3): 497–503. doi:10.1111/cas.13145. PMC 5378259. PMID 28012214.
- ↑ Jeong Il Yu (2018). "Initial clinical outcomes of proton beam radiotherapy for hepatocellular carcinoma". Radiat Oncol J. 36 (1): 25–34. doi:10.3857/roj.2017.00409. PMC 5903361. PMID 29580046.
- ↑ Awalpreet S Chadha (2019). "Proton beam therapy outcomes for localized unresectable hepatocellular carcinoma". Radiotherapy and Oncology. 133: 54–61. doi:10.1016/j.radonc.2018.10.041. PMC 6446916. PMID 30935582.
- ↑ Nina N Sanford (2018). "Protons versus Photons for Unresectable Hepatocellular Carcinoma: Liver Decompensation and Overall Survival". Int J Radiation Oncol Biol Phys. 105 (1): 64–72. doi:10.1016/j.ijrobp.2019.01.076. PMID 30684667.
- ↑ Chuong (2019). "Consensus Report From the Miami Liver Proton Therapy Conference". Front. Oncol. 9: 457. doi:10.3389/fonc.2019.00457. PMC 6557299. PMID 31214502.
- ↑ Shaed N Badiyan (2019). "Clinical Outcomes of Patients With Recurrent Lung Cancer Reirradiated With Proton Therapy on the Proton Collaborative Group and University of Florida Proton Therapy Institute Prospective Registry Studies". Pract Radiat Oncol. 9 (4): 280–288. doi:10.1016/j.prro.2019.02.008. PMID 30802618. S2CID 73499968.
- ↑ Paul B Romesser (2016). "Proton Beam Reirradiation for Recurrent Head and Neck Cancer: Multi-institutional Report on Feasibility and Early Outcomes". International Journal of Radiation Oncology, Biology, Physics. 95 (1): 386–395. doi:10.1016/j.ijrobp.2016.02.036. PMC 4997784. PMID 27084656.
- ↑ Vivek Verma (2017). "Systematic assessment of clinical outcomes and toxicities of proton radiotherapy for reirradiation". Radiotherapy and Oncology. 125 (1): 21–30. doi:10.1016/j.radonc.2017.08.005. PMID 28941560.
- ↑ Hann-Hsiang Chao (2017). "Multi-Institutional Prospective Study of Reirradiation with Proton Beam Radiotherapy for Locoregionally Recurrent Non-Small Cell Lung Cancer". J Thorac Oncol. 12 (2): 281–292. doi:10.1016/j.jtho.2016.10.018. PMID 27826034.
- ↑ Baumann BC (2020). "Comparative Effectiveness of Proton vs Photon Therapy as Part of Concurrent Chemoradiotherapy for Locally Advanced Cancer". JAMA Oncology. 6 (2): 237–246. doi:10.1001/jamaoncol.2019.4889. PMC 6990870. PMID 31876914.
- ↑ Steven H Lin (2020). "Randomized Phase IIB Trial of Proton Beam Therapy Versus Intensity-Modulated Radiation Therapy for Locally Advanced Esophageal Cancer". Journal of Clinical Oncology. 38 (14): 1569–1579. doi:10.1200/JCO.19.02503. PMC 7213588. PMID 32160096.
- ↑ Radhe Mohan (2020). "Proton Therapy Reduces the Likelihood of High-Grade Radiation-Induced Lymphopenia in Glioblastoma Patients: Phase II Randomized Study of Protons vs. Photons". Neuro-Oncology. 23 (2): 284–294. doi:10.1093/neuonc/noaa182. PMC 7906048. PMID 32750703.
- ↑ Michael Xiang (2020). "Second cancer risk after primary cancer treatment with three-dimensional conformal, intensity-modulated, or proton beam radiation therapy". Cancer. 126 (15): 3560–3568. doi:10.1002/cncr.32938. PMID 32426866. S2CID 218690280.
- ↑ Makbule Tambas (2020). "First experience with model-based selection of head and neck cancer patients for proton therapy". Radiotherapy and Oncology. 126 (15): 206–213. doi:10.1016/j.radonc.2020.07.056. PMID 32768508.
- ↑ Johannes A Langendijk (2013). "Selection of patients for radiotherapy with protons aiming at reduction of side effects: The model-based approach". Radiotherapy and Oncology. 107 (3): 267–273. doi:10.1016/j.radonc.2013.05.007. PMID 23759662.
- ↑ "Evaluation of Proton Therapy in Pediatric Cancer Patients". ClinicalTrials.gov. August 2020.
- ↑ "Registry for Analysis of Quality of Life, Normal Organ Toxicity and Survival of Pediatric Patients Treated With Proton Therapy". ClinicalTrials.gov. August 2020.
- ↑ "Trial of Proton Versus Carbon Ion Radiation Therapy in Patients With Chordoma of the Skull Base (HIT-1)". ClinicalTrials.gov. August 2020.
- ↑ "Intensity-Modulated Proton Therapy for Oropharyngeal Cancer". mdanderson.org. August 2020.
- ↑ "Study of Proton Versus Photon Beam Radiotherapy in the Treatment of Head and Neck Cancer". ClinicalTrials.gov. August 2020.
- ↑ Md, Helen A. Shih (August 2020). "A Trial of Increased Dose Intensity Modulated Proton Therapy (IMPT) for High-Grade Meningiomas". ClinicalTrials.gov.
- ↑ "Proton Radiotherapy for Primary Central Nervous System Tumours in Adults (PRO-CNS)". ClinicalTrials.gov. August 2020.
- ↑ "Dose-Escalated Photon IMRT or Proton Beam Radiation Therapy Versus Standard-Dose Radiation Therapy and Temozolomide in Treating Patients With Newly Diagnosed Glioblastom". ClinicalTrials.gov. August 2020.
- ↑ "Proton Beam or Intensity-Modulated Radiation Therapy in Preserving Brain Function in Patients With IDH Mutant Grade II or III Glioma". ClinicalTrials.gov. August 2020.
- ↑ "Radiation Therapy With Protons or Photons in Treating Patients With Liver Cancer". ClinicalTrials.gov. August 2020.
- ↑ Lin, Shi-Ming (August 2020). "Proton Radiotherapy Versus Radiofrequency Ablation for Patients With Medium or Large Hepatocellular Carcinoma". ClinicalTrials.gov.
- ↑ Md, Michael Devera (August 2020). "Transarterial Chemoembolization Versus Proton Beam Radiotherapy for the Treatment of Hepatocellular Carcinoma". ClinicalTrials.gov.
- ↑ "Comparing Photon Therapy To Proton Therapy To Treat Patients With Lung Cancer". ClinicalTrials.gov. August 2020.
- ↑ "A Phase I/II Study of Hypofractionated Proton Therapy for Stage II-III Non-Small Cell Lung Cancer". ClinicalTrials.gov. August 2020.
- ↑ Schild, Steven (August 2020). "Phase II Trial of Standard Chemotherapy (Carboplatin & Paclitaxel) +Various Proton Beam Therapy (PBT) Doses". ClinicalTrials.gov.
- ↑ "Comparing Proton Therapy to Photon Radiation Therapy for Esophageal Cancer". ClinicalTrials.gov. August 2020.
- ↑ "Dose Escalation of Neoadjuvant Proton Beam Radiotherapy With Concurrent Chemotherapy in Locally Advanced Esophageal Cancer". ClinicalTrials.gov. August 2020.
- ↑ "Pragmatic Randomized Trial of Proton vs. Photon Therapy for Patients With Non-Metastatic Breast Cancer: A Radiotherapy Comparative Effectiveness (RADCOMP) Consortium Trial". ClinicalTrials.gov. August 2020.
- ↑ "Phase II Protocol of Proton Therapy for Partial Breast Irradiation in Early Stage Breast Cancer". ClinicalTrials.gov. August 2020.
- ↑ "Phase I Nab-Paclitaxel Plus Gemcitabine With Proton Therapy for Locally Advanced Pancreatic Cancer (LAPC)". ClinicalTrials.gov. August 2020.
- ↑ "Proton Radiation for Unresectable, Borderline Resectable, or Medically Inoperable Carcinoma of the Pancreas". ClinicalTrials.gov. August 2020.
- ↑ "Introducing Hyperscan". mevion.com. Mevion Medical Systems. 2015-04-19.
- ↑ Sheets, NC; Goldin, GH; Meyer, AM; Wu, Y; et al. (April 18, 2012). "Intensity-modulated radiation therapy, proton therapy, or conformal radiation therapy and morbidity and disease control in localized prostate cancer". The Journal of the American Medical Association. 307 (15): 1611–20. doi:10.1001/jama.2012.460. PMC 3702170. PMID 22511689.
- ↑ Tepper, Joel E.; Blackstock, A. William (20 October 2009). "Editorial: Randomized Trials and Technology Assessment". Annals of Internal Medicine. 151 (8): 583–584. doi:10.7326/0003-4819-151-8-200910200-00146. PMID 19755346.
- ↑ Goitein, M.; Jermann, M. (2003). "The Relative Costs of Proton and X-ray Radiation Therapy". Clinical Oncology. 15 (1): S37–50. doi:10.1053/clon.2002.0174. PMID 12602563.
- 1 2 Bassett, Anne. "Siteman Cancer Center Treats First Patient With First-of-Its-Kind Proton Therapy System". PRWeb.com (Press release). Barnes-Jewish Hospital. Retrieved 2017-10-05.
- 1 2 Roland, Denise (September 25, 2013). "God particle technology to cancer patients". The Telegraph. Retrieved 2017-10-05.
- ↑ Lievens, Y.; Van den Bogaert, W; et al. (2005). "Proton beam therapy: Too expensive to become true?". Radiotherapy and Oncology. 75 (2): 131–133. doi:10.1016/j.radonc.2005.03.027. PMID 15890422.
- ↑ St Clair, W. H.; Adams, J. A.; Bues, M.; Fullerton, B. C.; La Shell, S.; Kooy, H. M.; Loeffler, J. S.; Tarbell, N. J. (2004). "Advantage of protons compared to conventional X-ray or IMRT in the treatment of a pediatric patient with medulloblastoma". Int. J. Radiat. Oncol. Biol. Phys. 58 (3): 727–734. doi:10.1016/S0360-3016(03)01574-8. PMID 14967427.
- ↑ Merchant, T. E.; Hua, C. H.; Shukla, H.; Ying, X.; Nill, S.; Oelfke, U. (2008). "Proton versus photon radiotherapy for common pediatric brain tumors: comparison of models of dose characteristics and their relationship to cognitive function". Pediatr. Blood Cancer. 51 (1): 110–117. doi:10.1002/pbc.21530. PMID 18306274. S2CID 36735536.
- ↑ Konski A.; Speier W.; Hanlon A.; Beck J. R.; Pollack A. (2007). "Is proton beam therapy cost effective in the treatment of adenocarcinoma of the prostate?". J. Clin. Oncol. 25 (24): 3603–3608. doi:10.1200/jco.2006.09.0811. PMID 17704408.
- ↑ Nguyen, P. L.; Trofimov, A.; Zietman, A. L. (June 22, 2008). "Proton-Beam vs. Intensity-Modulated Radiation Therapy, Which Is Best for Treating Prostate Cancer?". Oncology (Williston Park). 22 (7): 748–754, discussion 754, 757. PMID 18619120.
- ↑ Langreth, Robert (March 26, 2012). "Prostate Cancer Therapy Too Good to Be True Explodes Health Cost". Bloomberg.com. Retrieved 2013-05-16.
- 1 2 Muralidhar, Vinayak; Nguyen, Paul L. (February 2017). "Maximizing resources in the local treatment of prostate cancer: A summary of cost-effectiveness studies". Urologic Oncology. 35 (2): 76–85. doi:10.1016/j.urolonc.2016.06.003. ISSN 1873-2496. PMID 27473636.
- ↑ Yuan, Tai-Ze; Zhan, Ze-Jiang; Qian, Chao-Nan (22 October 2019). "New frontiers in proton therapy: applications in cancers". Cancer Communications. 39 (1): 61. doi:10.1186/s40880-019-0407-3. ISSN 2523-3548. PMC 6805548. PMID 31640788.
- ↑ Hancock, Jay (April 27, 2018). "For Cancer Centers, Proton Therapy's Promise Is Undercut by Lagging Demand". The New York Times.
- ↑ "Wise Buy? Proton Beam Therapy". www.medpagetoday.com. May 19, 2017.
- ↑ "Particle therapy facilities in operation". PTCOG.ch. Particle Therapy Co-Operative Group. August 2020. Retrieved 2020-08-01.
- ↑ "Particle therapy facilities under construction". PTCOG.ch. Particle Therapy Co-Operative Group. June 2017. Retrieved 2017-10-06.
- ↑ "Statistics of patients treated in particle therapy facilities worldwide". PTCOG.ch. Particle Therapy Co-Operative Group. 2016. Retrieved 2017-10-06.
- 1 2 Matthews, J. N. A. (March 2009). "Accelerators shrink to meet growing demand for proton therapy". Physics Today. p. 22.
- ↑ Nafziger, Brendon (March 20, 2012). "N.J. proton therapy center opens today". DotMed.com. Retrieved 2012-03-30.
- ↑ "Proton Therapy Treatment and Research Center". Loma Linda University Medical Center. Retrieved 2013-11-05.
- ↑ "Cyclotron Services". crocker.udavis.edu. University of California, Davis, Crocker Nuclear Laboratory. Retrieved 2017-10-05.
- 1 2 3 4 5 6 7 8 9 10 11 12 "Best proton therapy centers – IBA proton therapy". iba-worldwide.com. Retrieved 2018-03-16.
- ↑ "Proton Therapy Jacksonville | Cancer Treatment". University of Florida Proton Therapy Institute. Retrieved 2013-11-05.
- ↑ "Proton Therapy Center". University of Texas MD Anderson Cancer Center. Retrieved 2013-11-05.
- ↑ "Oklahoma Proton Therapy Treatment Center". ProCure. Retrieved 2013-11-05.
- ↑ "Proton Therapy at Penn Medicine". Perelman Center for Advanced Medicine. Retrieved 2013-11-05.
- ↑ "New Jersey Proton Therapy Treatment Center". ProCure. Archived from the original on 2010-11-26. Retrieved 2013-11-05.
- ↑ "Elegant and Precise". Mevion Medical Systems. Archived from the original on 2015-04-14. Retrieved 2015-04-19.
- ↑ "Introducing the Mevion S250". Mevion. Archived from the original on 2015-04-14. Retrieved 2015-04-19.
- ↑ "Proton therapy cancer treatment center opens, first of its kind in Tennessee". WATE-TV. Archived from the original on 2014-01-26. Retrieved 2014-01-25.
{{cite web}}: CS1 maint: bot: original URL status unknown (link) - ↑ "California Protons Cancer Therapy Center". California Protons Cancer Therapy Center. Retrieved 2017-12-18.
- ↑ "Oncology, Solutions, Proton Therapy". Varian Medical Systems. Archived from the original on 2019-01-07. Retrieved 2015-04-19.
- ↑ "Texas Center for Proton Therapy Treats First Patient with Isocentric Cone Beam CT and Pencil Beam Scanning" (Press release). Irving, Texas: McKesson. May 9, 2016. Retrieved 2017-10-05.
- ↑ "Mayo Clinic launches Proton Beam Therapy Program". mayoclinic.org. Mayo Clinic. Retrieved 2017-10-05.
- ↑ "Hitachi's Advanced Proton Beam Therapy System "PROBEAT-V" Begins Treatments at Mayo Clinic in Rochester, MN" (Press release). Tokyo, Japan: Hitachi. September 15, 2015. Retrieved 2018-05-01.
- ↑ "Mayo Clinic Cancer Center". mayoclinic.org. Mayo Clinic.
- ↑ "Hitachi "PROBEAT-V" Advanced Proton Beam Therapy System Now In Use at Mayo Clinic in Arizona" (Press release). Tokyo, Japan: Hitachi. March 15, 2016. Retrieved 2018-05-01.
- ↑ "Proton Therapy at University of Cincinnati Medical Center". uchealth.com. University of Cincinnati Cancer Institute, UC Health. Retrieved 2017-10-05.
- ↑ "Pediatric Proton Therapy Center". cincinnatichildrens.org. Cincinnati Children's Hospital Medical Center. Retrieved 2017-10-05.
- ↑ "Proton Therapy at Miami Cancer Institute". baptisthealth.net. Baptist Health South Florida. Retrieved 2017-10-05.
- ↑ "Emory Proton Therapy Center Fact Sheet" (PDF). winshipcancer.emory.edu. Emory Winship Cancer Institute. Retrieved 2018-03-05.
- ↑ "KU Health System to offer innovative, new proton therapy cancer treatment". 26 February 2019. Retrieved 2019-05-29.
- ↑ "Integrated oncology facility with proton beam therapy planned for Mayo Clinic's Florida campus". newsnetwork.mayoclinic.org.
- ↑ "Proton therapy". clatterbridgecc.nhs.uk. Clatterbridge Cancer Centre NHS Foundation Trust. Archived from the original on 2014-01-15. Retrieved 2017-10-05.
- ↑ "Proton Therapy". TRIUMF.ca. Archived from the original on 2017-06-27. Retrieved 2017-10-05.
- ↑ "Proton Therapy Center - Trento". protonterapia.provincia.tn.it.
- ↑ "Kaohsiung Branch-Yung-Ching Proton Center". www.chang-gung.org.
- ↑ "Skandionkliniken — Nordens första klinik för protonstrålning". Startsida.
- ↑ "Протонный центр МИБС". protherapy.ru.
- ↑ "Welkom bij HollandPTC". HPTC.
- ↑ "Corporate information". www.umcg.nl.
- ↑ "The Christie".
- ↑ "Danish Centre for Particle Therapy". www.en.auh.dk.
- ↑ Proton Therapy Centre Apollo Hospitals
- ↑ "Maastro is the first true compact proton therapy system in Europe" (PDF). www.maastro.nl/.
- ↑ "Proton therapy delivered to patient for the first time in Spain". 15 January 2020.
- ↑ King Chulalongkorn Memorial Hospital
- ↑ University College London Hospitals
- ↑ "Singapore Institute of Advanced Medicine Holdings". www.advancedmedicine.sg.
- ↑ "Hefei Ion Medical Center". hefeihightech.chinadaily.com.cn.
- ↑ "Australian Bragg Centre for Proton Therapy". Australian Bragg Centre for Proton Therapy.
- 1 2 Spence, Andrew (10 June 2020). "Proton therapy focus of 'SAHMRI 2'". InDaily. Retrieved 6 July 2020.
- ↑ www.ETHealthworld.com. "Modern cancer treatments ensure that every single mm of the tissue beyond the tumor is preserved: Dr.Rakesh Jalali - ET HealthWorld". ETHealthworld.com. Retrieved 2021-12-06.
- ↑ "Apollo Proton Centre gets JCI accreditation". The Hindu. Special Correspondent. 2020-07-04. ISSN 0971-751X. Retrieved 2021-12-06.
{{cite news}}: CS1 maint: others (link) - ↑ Israel to Establish National Center for Proton Radiation Cancer Therapy
- ↑ Programme for the implementation of proton therapy in the Spanish public health system
- ↑ "Manchester and London proton beam therapy units confirmed", Press release, Press Association, Cancer Research UK, 1 August 2013
- ↑ "Ashya King case: What is proton beam therapy?" BBC news story with NHS England figures, 31 August 2014
Further reading
- Greco C.; Wolden S. (Apr 2007). "Current status of radiotherapy with proton and light ion beams". Cancer. 109 (7): 1227–1238. doi:10.1002/cncr.22542. PMID 17326046. S2CID 36256866.
- "Use of Protons for Radiotherapy", A.M. Koehler, Proc. of the Symposium on Pion and Proton Radiotherapy, Nat. Accelerator Lab., (1971).
- A.M. Koehler, W.M. Preston, "Protons in Radiation Therapy: comparative Dose Distributions for Protons, Photons and Electrons Radiology 104(1):191–195 (1972).
- "Bragg Peak Proton Radiosurgery for Arteriovenous Malformation of the Brain" R.N. Kjelberg, presented at First Int. Seminar on the Use of Proton Beams in Radiation Therapy, Moskow (1977).
- Austin-Seymor, M.J. Munzenrider, et al. "Fractionated Proton Radiation Therapy of Cranial and Intracrainial Tumors" Am. J. of Clinical Oncology 13(4):327–330 (1990).
- "Proton Radiotherapy", Hartford, Zietman, et al. in Radiotheraputic Management of Carcinoma of the Prostate, A. D'Amico and G.E. Hanks. London, UK, Arnold Publishers: 61–72 (1999).
External links
| Wikimedia Commons has media related to Proton therapy. |
- The Intrepid Proton-Man, educational comic books by Steve Englehart and Michael Jaszewski for pediatric patients
- 2019 BBC Horizon documentary
- 2019 Jove video by the University of Maryland School of Medicine explaining the treatment process: Proton Therapy Delivery and Its Clinical Application in Select Solid Tumor Malignancies
- 2019 The NHS Proton Beam Therapy Programme
- Proton Therapy Collaborative Group PTCOG
- Alliance for Proton Therapy
- CARES Cancer Network
- National Association for Proton Therapy
- American Society for Radiation Oncology Model Policy – Proton Beam Therapy
- Proton therapy – MedlinePlus Medical Encyclopedia
- Proton Therapy
- What is Proton Therapy