Chondrosarcoma
| Chondrosarcoma | |
|---|---|
.jpg.webp) | |
| Chondrosarcoma long bone of thigh near knee | |
Chondrosarcoma is a canerous bone tumor of the cartilaginous type.[1][2]
It is a bone sarcoma, a primary cancer composed of cells derived from transformed cells that produce cartilage.[3] A chondrosarcoma is a member of a category of tumors of bone and soft tissue known as sarcomas. About 30% of bone sarcomas are chondrosarcomas.[4] It is resistant to chemotherapy and radiotherapy. Unlike other primary bone sarcomas that mainly affect children and adolescents, a chondrosarcoma can present at any age. It more often affects the axial skeleton than the appendicular skeleton.[5]
Types
| Subtype | Percentage of cases % | |
|---|---|---|
| Conventional | Primary Central | ~75%[6] |
| Secondary Peripheral | ~10%[6] | |
| Periosteal (aka juxtacortical)[7][8] | <1%[6] | |
| Rare | Dedifferentiated | ~10%[6] |
| Mesenchymal | ~2%[6] | |
| Clear-cell | ~2%[8] |
Signs and symptoms
Causes
The cause is unknown. Patients may have a history of enchondroma or osteochondroma. A small minority of secondary chondrosarcomas occur in patients with Maffucci syndrome and Ollier disease.[9]
It has been associated with faulty isocitrate dehydrogenase 1 and 2 enzymes, which are also associated with gliomas and leukemias.[10]
Diagnosis

Imaging studies - including radiographs ("x-rays"), computerized tomography (CT), and magnetic resonance imaging (MRI) - are often used to make a presumptive diagnosis of chondrosarcoma.[11] However, a definitive diagnosis depends on the identification of malignant cancer cells producing cartilage in a biopsy specimen that has been examined by a pathologist. In a few cases, usually of highly anaplastic tumors, immunohistochemistry (IHC) is required.
There are no blood tests currently available to enable an oncologist to render a diagnosis of chondrosarcoma. The most characteristic imaging findings are usually obtained with CT.
Nearly all chondrosarcoma patients appear to be in good health. Often, patients are not aware of the growing tumor until there is a noticeable lump or pain. Earlier diagnosis is generally accidental, when a patient undergoes testing for another problem and physicians discover the cancer. Occasionally the first symptom will be a broken bone at the cancerous site. Any broken bone that occurs from mild trauma warrants further investigation, although there are many conditions that can lead to weak bones, and this form of cancer is not a common cause of such breaks.
Imaging
.jpg.webp) Chondrosarcoma spine
Chondrosarcoma spine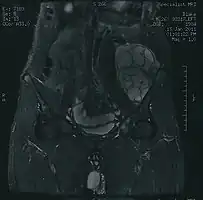 MRI of a left-pelvis chondrosarcoma in a 26-year-old male
MRI of a left-pelvis chondrosarcoma in a 26-year-old male
Histopathology
Treatment
Treatment depends on the location of the disease and the aggressiveness of the tumors.[12] Because chondrosarcomas are rare, they are treated at specialist hospitals with Sarcoma Centers.
Surgery is the main form of treatment for chondrosarcoma. Musculoskeletal tumor specialists or orthopedic oncologists are usually chosen to treat chondrosarcoma, unless it is located in the skull, spine, or chest cavity, in which case, a neurosurgeon or thoracic surgeon experienced with sarcomas is chosen. Often, a limb-sparing operation can be performed, but in some cases amputation is unavoidable. Amputation of the arm, leg, jaw, or half of the pelvis (called a hemipelvectomy) may be necessary in some cases.
There are two kinds of hemipelvectomy - internal and external.
- External hemipelvectomy - is removal of that half of the pelvis with the amputation of the leg. It is also called the hindquarter amputation.
- Internal hemipelvectomy - is removal of that half of the pelvis, but the leg is left intact.
Amputation at the hip is called hip disarticulation and amputees who have had this amputation are also called hip disartics.
Chemotherapy or traditional radiotherapy are not very effective for most chondrosarcomas, although proton therapy is showing promise with local tumor control at over 80%.[13]
Complete surgical ablation is the most effective treatment, but sometimes this is difficult. Proton therapy radiation can be useful in awkward locations to make surgery more effective.
Recent studies have shown that induction of apoptosis in high-grade chondrosarcoma, both directly and by enhancement of response to chemotherapy and radiation, is a valid therapeutic strategy.[14]
Prognosis
Prognosis depends on how early the cancer is discovered and treated. For the least aggressive grade, about 90% of patients survive more than five years after diagnosis. People usually have a good survival rate at the low grade volume of cancer.[5] For the most aggressive grade, only 10% of patients will survive one year. Tumors may recur in the future. Follow up scans are extremely important for chondrosarcoma to make sure there has been no recurrence or metastasis, which usually occurs in the lungs.
References
- ↑ Chow, Warren A (20 November 2018). "Chondrosarcoma: biology, genetics, and epigenetics". F1000Research. 7: F1000 Faculty Rev–1826. doi:10.12688/f1000research.15953.1. ISSN 2046-1402. PMID 30519452. Archived from the original on 18 March 2021. Retrieved 19 October 2021.
- ↑ Soft Tissue and Bone Tumours: WHO Classification of Tumours. International Agency for Research on Cancer. 2020. p. 338. ISBN 978-92-832-4502-5. Archived from the original on 2021-06-13. Retrieved 2021-10-19.
- ↑ Gelderblom H, Hogendoorn PC, Dijkstra SD, et al. (March 2008). "The clinical approach towards chondrosarcoma". Oncologist. 13 (3): 320–9. doi:10.1634/theoncologist.2007-0237. PMID 18378543.
- ↑ "Archived copy". Archived from the original on 2012-04-30. Retrieved 2011-10-30.
{{cite web}}: CS1 maint: archived copy as title (link) - 1 2 "Chondrosarcoma: Overview - eMedicine Radiology". Archived from the original on 2008-11-22. Retrieved 2009-02-14.
- 1 2 3 4 5 Gelderblom, Hans; Hogendoorn, Pancras C. W.; Dijkstra, Sander D.; van Rijswijk, Carla S.; Krol, Augustinus D.; Taminiau, Antonie H. M.; Bovée, Judith V. M. G. (March 2008). "The clinical approach towards chondrosarcoma". The Oncologist. 13 (3): 320–329. doi:10.1634/theoncologist.2007-0237. ISSN 1083-7159. PMID 18378543. Archived from the original on 2021-08-28. Retrieved 2020-12-24.
- ↑ Schajowicz, F. (November 1977). "Juxtacortical chondrosarcoma". The Journal of Bone and Joint Surgery. British Volume. 59-B (4): 473–480. ISSN 0301-620X. PMID 270475. Archived from the original on 2021-08-28. Retrieved 2020-12-24.
- 1 2 Pathology and genetics of tumours of soft tissue and bone. Fletcher, Christopher D. M., Unni, K. Krishnan, 1941-, Mertens, Fredrik., World Health Organization., International Agency for Research on Cancer. Lyon: IARC Press. 2002. ISBN 978-92-832-2413-6. OCLC 51001831. Archived from the original on 2021-08-28. Retrieved 2020-12-24.
{{cite book}}: CS1 maint: others (link) - ↑ Lin, Patrick P.; Moussallem, Charbel D.; Deavers, Michael T. (Oct 2010). "Secondary chondrosarcoma". The Journal of the American Academy of Orthopaedic Surgeons. 18 (10): 608–615. doi:10.5435/00124635-201010000-00004. ISSN 1067-151X. PMID 20889950.
- ↑ Amary, M. Fernanda; Bacsi, Krisztian; Maggiani, Francesca; Damato, Stephen; Halai, Dina; Berisha, Fitim; Pollock, Robin; O'Donnell, Paul; Grigoriadis, Anita (Jul 2011). "IDH1 and IDH2 mutations are frequent events in central chondrosarcoma and central and periosteal chondromas but not in other mesenchymal tumours". The Journal of Pathology. 224 (3): 334–343. doi:10.1002/path.2913. ISSN 1096-9896. PMID 21598255.
- ↑ CT scan and gross pathology of a chondrosarcoma Archived 2020-04-27 at the Wayback Machine 2012-12-18
- ↑ "Chondrosarcoma : Cancerbackup". Archived from the original on 2008-09-05. Retrieved 2009-02-14.
- ↑ "Proton Therapy at PSI (Protonentherapie)". Archived from the original on 2009-02-14. Retrieved 2009-02-14.
- ↑ Jamil N, Howie S, Salter DM. Therapeutic molecular targets in human chondrosarcoma .Int J Exp Pathol 2010; 91:387-93
External links
| Classification | |
|---|---|
| External resources |
.jpg.webp)
.jpg.webp)
.jpg.webp)
.jpg.webp)