Superior ganglion of vagus nerve
| Superior ganglion of vagus nerve | |
|---|---|
 Plan of upper portions of glossopharyngeal, vagus, and accessory nerves. The superior ganglion of the vagus nerve is labeled as ‘jugular gang.’ | |
| Details | |
| From | vagus nerve |
| To | auricular branch of vagus nerve or meningeal branch of vagus nerve |
| Innervates | dura mater of posterior cranial fossa, parts of the auricle, external auditory canal and external surface of tympanic membrane |
| Identifiers | |
| Latin | ganglion superius nervi vagi, ganglion jugulare |
| TA98 | A14.2.01.154 |
| TA2 | 6333 |
| FMA | 6229 |
| Anatomical terms of neuroanatomy | |
The superior ganglion of the vagus nerve, (jugular ganglion) is a sensory ganglion of the peripheral nervous system. It is located within the jugular foramen, where the vagus nerve exits the skull. It is smaller than and proximal to the inferior ganglion of the vagus nerve.[1][2]
Structure
The neurons in the superior ganglion of the vagus nerve are pseudounipolar and provide sensory innervation (general somatic afferent) through either the auricular or meningeal branch. The axons of these neurons synapse in the spinal trigeminal nucleus of the brainstem.[1] Peripherally, the neurons found in the superior ganglion form two branches, the auricular and meningeal branch.
Function
Auricular branch of the vagus nerve
The superior ganglion contains neurons which innervate the concha of the auricle,[3] the posteroinferior surface of the external auditory canal and posteroinferior surface of the tympanic membrane all via the auricular branch of the vagus nerve.[4][5]
Meningeal branch of the vagus nerve
The superior ganglion contains neurons which innervate some of the dura mater lining the posterior cranial fossa via the meningeal branch of the vagus nerve.[6][7]
Development
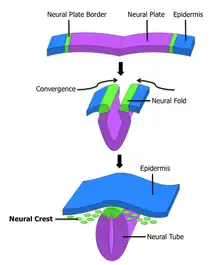
The neurons in the superior ganglion of the vagus nerve are embryonically derived from the neural crest.[8]
Clinical significance
Vagal neuralgia
Pain in the external auditory canal (otalgia) can in rare cases be due to vagal neuralgia because of vascular compression of the vagus nerve (often by the posterior inferior cerebellar artery). The affected neurons are found in the superior ganglion and innervate the ear via the auricular branch of the vagus. The condition is treated by microvascular decompression of the vagus nerve where it exits the brainstem.[5]
References
- 1 2 Rubin, Michael (2016). Netter's Concise Neuroanatomy. Safdieh, Joseph E.,, Netter, Frank H. (Frank Henry), 1906-1991 (Updated 1st ed.). Philadelphia, PA: Elsevier. pp. 259–260. ISBN 9780323480918. OCLC 946698976.
- ↑ Burt, Alvin M. (1993). Textbook of Neuroanatomy (1st ed.). Philadelphia: W.B. Saunders. pp. 423-427. ISBN 0721621996. OCLC 24503849.
- ↑ Mercante B, Ginatempo F, Manca A, Melis F, Enrico P, Deriu F (June 2018). "Anatomo-Physiologic Basis for Auricular Stimulation". Medical Acupuncture. 30 (3): 141–150. doi:10.1089/acu.2017.1254. PMC 6011382. PMID 29937968.
- ↑ Tekdemir I, Aslan A, Elhan A (1998). "A clinico-anatomic study of the auricular branch of the vagus nerve and Arnold's ear-cough reflex". Surgical and Radiologic Anatomy. 20 (4): 253–7. PMID 9787391.
- 1 2 Watanabe, Kentaro; Tubbs, R. Shane; Satoh, Shunsuke; Zomorodi, Ali R.; Liedtke, Wolfgang; Labidi, Moujahed; Friedman, Allan H.; Fukushima, Takanori (December 2016). "Isolated Deep Ear Canal Pain: Possible Role of Auricular Branch of Vagus Nerve-Case Illustrations with Cadaveric Correlation". World Neurosurgery. 96: 293–301. doi:10.1016/j.wneu.2016.08.102. ISSN 1878-8769. PMID 27593717.
- ↑ Kemp WJ, Tubbs RS, Cohen-Gadol AA (November 2012). "The innervation of the cranial dura mater: neurosurgical case correlates and a review of the literature". World Neurosurgery. 78 (5): 505–10. doi:10.1016/j.wneu.2011.10.045. PMID 22120554.
- ↑ Keller JT, Saunders MC, Beduk A, Jollis JG (January 1985). "Innervation of the posterior fossa dura of the cat". Brain Research Bulletin. 14 (1): 97–102. doi:10.1016/0361-9230(85)90181-9. PMID 3872702. S2CID 4763767.
- ↑ Thompson H, Blentic A, Watson S, Begbie J, Graham A (February 2010). "The formation of the superior and jugular ganglia: insights into the generation of sensory neurons by the neural crest". Developmental Dynamics. 239 (2): 439–45. doi:10.1002/dvdy.22179. PMID 20014097.