This article was co-authored by Rebecca Levy-Gantt, MPT, DO and by wikiHow staff writer, Janice Tieperman. Dr. Rebecca Levy-Gantt is a board certified Obstetrician and Gynecologist running a private practice based in Napa, California. Dr. Levy-Gantt specializes in menopause, peri-menopause and hormonal management, including bio-Identical and compounded hormone treatments and alternative treatments. She is also a Nationally Certified Menopause Practitioner and is on the national listing of physicians who specialize in menopausal management. She received a Masters of Physical Therapy from Boston University and a Doctor of Osteopathic Medicine (DO) from the New York College of Osteopathic Medicine.
There are 24 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 90% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 41,220 times.
Nervous about your first period? That’s totally fair, especially if you’ve heard your fair share of horror stories from friends and family members. You have nothing to worry about, though. There’s nothing strange, scary, or embarrassing about getting your first period, especially if you prepare yourself ahead of time. We’re here to walk you through all of the period supplies you’ll need, as well as how to use them. We’ve even answered some of your most common questions, so you can stay as informed as possible during this new chapter of your life.
Steps
Securing Supplies
-
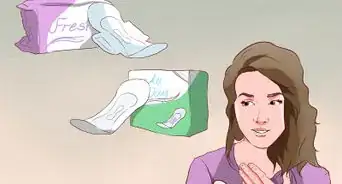
1Stock up on pads and tampons. Pads and tampons are 2 of the most common ways to soak up your menstrual flow without getting your clothes dirty in the process. [1] You can find these sanitary supplies at your local drugstore or big-box retail store.
- Pads are long, flat rectangles of absorbent material that stick to the center of your underwear. They soak up any extra period flow that leaves your vagina.
- Tampons are cylindrical pieces of cotton wool that go directly into your vaginal canal. They absorb your period flow at the source.[2]
-
2Make a period kit that you can bring with you to different places. This kit contains everything you need for your period and keeps you feeling clean and protected if you run into an accident at school or some other place away from home. Be sure to include:[3]
- Pads
- Tampons
- Clean, period-proof underwear
- Painkillers
- Think about making 2 period kits: one that you keep at school and one that you keep at home.
Advertisement -
3Store some spare pants and underwear in a safe place at school. Feel free to stash them in your locker or backpack, so you can grab them easily. If you end up leaking during the school day, head over to the bathroom and change.[4]
- You can also conceal leaks by wrapping a sweatshirt around your waist.
- Pack some dark pants or skirts, if you can. These are better at concealing leaks.[5]
-
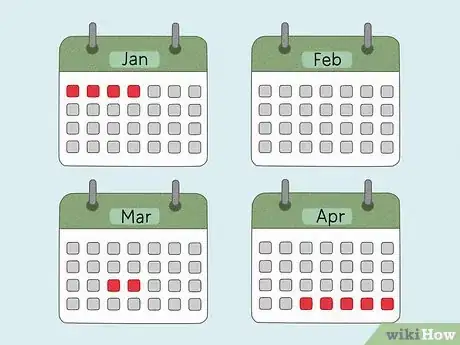
4Grab a calendar so you can track your period. Your period happens on a fairly regular schedule, and a calendar can help you time and predict your cycles more accurately. It’s also a great way to track any symptoms you experience during your period.[6]
- A calendar can also help you find any irregular period patterns, which you can report to your doctor.
- You can also use a phone app to track your period. “Me V PMDD,” “Flo Period & Ovulation,” “Period Diary,” and “Cycles” are a few free apps you can try.[7]
Using a Pad
-
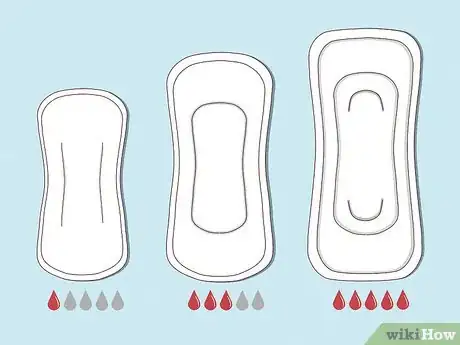
1Choose a pad that’s absorbent enough for your period flow. Pads come in all shapes and sizes, ranging from thin pantyliners to thick, extra-absorbent “maxi” pads. Pick an absorbency level that best lines up with your flow, so you can stay comfortable and protected throughout the day. Here’s a quick guide to help you choose:[8]
- Light flow: pantyliners
- Moderate flow: regular pads
- Heavy flow: maxi pads
-
2Peel off any paper strips from the back and sides of the pad. Remove the pad from its wrapper and look for a long, rectangular strip of paper going down the center—this covers the pad’s backing adhesive. Then, remove any backing paper from the wings (side sections) of the pad if it has them.[9]
- You can double-check your pad container to see if your pads have wings or not.
-
3Secure the pad in place along the center of your underwear. Cover the entire middle section of your underwear with the sticky pad, pressing it in place to make sure it’s secure. If your pad has wings, wrap and press them along the very bottom of your panties.[10]
- Remember—there’s nothing weird or strange about using a pad. Lots of people use them to manage their periods!
-
4Replace your pad once every few hours or whenever it’s soaked. Gently peel the pad off of your underwear and cover it with a section of toilet paper. Then, throw the pad out in the trash or in the disposal box along the side of a public bathroom stall. Grab a new pad and secure it in place on your underwear, so you stay protected and covered.[11]
- Feel free to change your pad earlier if it gets soaked really quickly. In this case, it might be worth switching to a more absorbent pad.
- Don’t flush your used pad down the toilet. These products aren’t designed to be flushed, and will likely back up the toilet.
Inserting a Tampon
-
1Wash your hands thoroughly with soap and water. You’ll be inserting the tampon directly into your vaginal canal with your bare hands, so it’s really important to wash them before you get started.[12] Always scrub your hands with soap and warm water for at least 20 seconds, and be sure to dry them off before you begin.[13]
-
2Choose a tampon absorbency that meets your needs. Tampons come in 5 different absorbency levels: light, regular, super, super plus, and ultra.[14] Medical professionals recommend starting with a lighter absorbency tampon, and working your way up as needed.[15]
- The higher the absorbency you use, the higher risk you have of developing Toxic Shock Syndrome, an uncommon but dangerous condition associated with tampons.[16]
-
3Squat, get seated on the toilet, or prop one of your legs up. Some people prefer to sit on the toilet when putting a tampon in, while other people prefer to squat. Other people find it even easier to sit or squat while propping a leg up to the side. Try out these different positions and see which one feels the most secure and comfortable for you.[17]
- Spread your knees out if you stay seated. This will make it a lot easier to get the tampon in.
-
4Grip the tampon with your thumb and middle finger. Pull the tampon out of its wrapper and hold it in one hand. The tampon itself is typically stuffed inside a plastic or cardboard applicator—this is the plunger-like device that helps push the tampon further into your vagina. Hold the bottom of the tampon’s long, vertical barrel in between your thumb and middle finger. Then, place your pointer finger beneath the plunger on the bottom.[18]
- There are also non-applicator tampons, which you insert with only your fingers. Some people really like them, while other people find them really difficult to work with.[19] An applicator tampon is likely easier to work with when you first learn the ropes.[20]
-
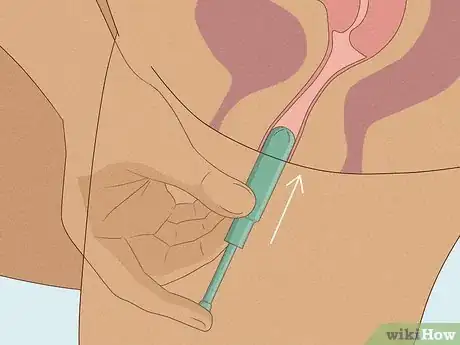
5Slide the tampon into your vagina at an angle. Point the tip of your tampon toward your spine instead of holding it completely straight. Then, guide the barrel of the tampon into your vagina using your fingers. Try to relax while you do this—it’s a lot easier to get your tampon in place when your muscles aren’t tense.[21]
- Remember: your vagina is behind your urethra (the tiny opening for peeing) and in front of your anus.[22] When your fingers touch the vaginal opening, they may come away looking bloody.
- A tampon might feel a bit strange and uncomfortable at first, but it should never feel painful going in. Be sure to let your doctor know if you start experiencing a lot of pain.[23]
-
6Press the applicator with your pointer finger to release the tampon into your vaginal canal. Push the plunger all the way up until it’s inside the top portion of the applicator. This helps push the tampon a little further into your vaginal canal, so it can do a better job soaking up your period flow.[24]
- This process might feel a little weird at first, but you won’t actually feel the tampon once it’s inside you.
-
7Remove the plastic or cardboard applicator and throw it away. Pull the empty applicator out of your vagina and toss it in the nearest wastebasket or disposal box, along with the empty wrapper. At this point, look for a long, white string dangling out from your vagina.[25]
- This string helps you pull out your tampon later on.
-
8Leave the tampon in place for 4-6 hours. Tampons help provide long-term support and protection, but they shouldn’t be left in your vagina indefinitely. Check your underwear around the 4-hour mark to see how the tampon is holding up. If it’s leaking, remove the old tampon and replace it with a new one. If you don’t notice any leaks, leave it in for 2 more hours.[26]
- You can keep your tampon in for as long as 8 hours, but most experts suggest following the 4-6 hour rule.[27]
-
9Tug on the dangling string to remove the tampon. Firmly grab the string and pull with a moderate amount of pressure. In a matter of moments, the tampon will slide out.[28] Don’t panic if you can’t find the string; instead, grab the tampon with your fingers and pull it out manually.[29]
- Visit your doctor’s office or a nearby reproductive health clinic if you’re having trouble removing the tampon on your own.
-
10Throw out your tampon instead of flushing it down the toilet. Tampons can mess with your plumbing, even if they’re labeled as safe to flush. Instead, cover the used tampon with a section of clean toilet paper and toss it in the nearest trash can or bathroom disposal box.[30]
- Practice makes perfect! The more you use tampons, the more confident and comfortable you’ll feel during your future periods.
Learning about Menstruation
-
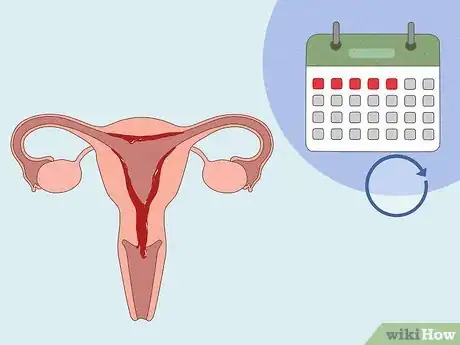
1Menstruation is a monthly cycle. As you get older, your body starts to mature and develop during a process called “puberty.” One of these developments is your menstrual cycle, a monthly process where your body gets ready to potentially have a baby. This cycle causes blood and other bodily fluids to flow out of your vagina for a short period of days.[31]
- Each month, the walls of your uterus thicken with extra blood and tissue and your ovaries release an egg. This egg moves down one of your two fallopian tubes and into the uterus.
- If fertilized by a sperm cell (through sex), the egg will remain in the uterus and grow into a fetus. If this does not occur, the lining of the uterus breaks down, and bleeding occurs. This is what is referred to as your monthly period.
-
2Your period starts sometime during your teen or preteen years. Not all women begin menstruation around the same time. While the average age is 12, some girls start as late as 16 and others as early as 8.[32]
- Many people first get their period about 2 years after their breasts begin developing.
- Your period may start 6 months after you spot any clear, off-white, or white discharge appearing on your underwear.
-
3Many women experience physical and emotional symptoms during menstruation. Periods are not always painful, but some women do experience physical symptoms like cramps and tender breasts. You may have some emotional side effects, such as mood swings, as well.[33]
- While period symptoms can be a bit uncomfortable, they’re nothing to stress over. Over-the-counter painkillers like ibuprofen can be used to treat cramping and physical symptoms, along with a heating pad. Plus, exercising regularly, even during your period, can help regulate your mood, and make you feel healthier in general.
-
4The average period lasts between 2 and 7 days. When you first start getting your period, it may only last a few days, and your bleeding may be inconsistent or very light. Ask some female family members how long their periods last, because chances are, yours will be a similar length.[34]
-
5Periods tend to be irregular when you’re first starting out. Many girls are surprised and alarmed by their first periods as they may be irregular. However, menstrual irregularities are really common when you're first having your period.[35]
- It's common to miss a period here and there, and you may not have your period for a few months in a row. It can take up to 2 years for your menstrual cycle to become regular, so don’t worry if your current cycle is a bit inconsistent.
- Your first few periods may be very light or very heavy. You may also start bleeding, stop, and then start again.[36]
Expert Q&A
-
QuestionWhat are the signs of starting your first period?
 Rebecca Levy-Gantt, MPT, DODr. Rebecca Levy-Gantt is a board certified Obstetrician and Gynecologist running a private practice based in Napa, California. Dr. Levy-Gantt specializes in menopause, peri-menopause and hormonal management, including bio-Identical and compounded hormone treatments and alternative treatments. She is also a Nationally Certified Menopause Practitioner and is on the national listing of physicians who specialize in menopausal management. She received a Masters of Physical Therapy from Boston University and a Doctor of Osteopathic Medicine (DO) from the New York College of Osteopathic Medicine.
Rebecca Levy-Gantt, MPT, DODr. Rebecca Levy-Gantt is a board certified Obstetrician and Gynecologist running a private practice based in Napa, California. Dr. Levy-Gantt specializes in menopause, peri-menopause and hormonal management, including bio-Identical and compounded hormone treatments and alternative treatments. She is also a Nationally Certified Menopause Practitioner and is on the national listing of physicians who specialize in menopausal management. She received a Masters of Physical Therapy from Boston University and a Doctor of Osteopathic Medicine (DO) from the New York College of Osteopathic Medicine.
Board Certified Obstetrician & Gynecologist It depends! You may also see hair growing under your arms and in your pubic area before your first period. You may develop acne and your skin might get oilier too.
It depends! You may also see hair growing under your arms and in your pubic area before your first period. You may develop acne and your skin might get oilier too.
References
- ↑ https://www.nhs.uk/conditions/periods/
- ↑ https://www.nhs.uk/conditions/periods/
- ↑ https://raisingchildren.net.au/pre-teens/development/periods-hygiene/periods
- ↑ http://kidshealth.org/kid/grow/girlstuff/five_period.html?tracking=K_RelatedArticle#
- ↑ http://www.mayoclinic.org/healthy-lifestyle/tween-and-teen-health/in-depth/menstruation/art-20046004?pg=2
- ↑ https://www.womenshealth.gov/menstrual-cycle/your-menstrual-cycle
- ↑ https://www.cosmopolitan.com/sex-love/a18210028/best-period-tracker-fertility-app/
- ↑ https://www.plannedparenthood.org/learn/health-and-wellness/menstruation/how-do-i-use-tampons-pads-and-menstrual-cups
- ↑ https://kidshealth.org/en/teens/supplies.html
- ↑ https://kidshealth.org/en/teens/supplies.html
- ↑ https://kidshealth.org/en/teens/supplies.html
- ↑ https://kidshealth.org/en/kids/pads-tampons.html
- ↑ https://www.cdc.gov/handwashing/when-how-handwashing.html
- ↑ https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=801.430
- ↑ https://www.childrenspeds.com/health-resources/just-for-teens/education/tampon-safety
- ↑ https://www.childrenspeds.com/health-resources/just-for-teens/education/tampon-safety
- ↑ https://www.plannedparenthood.org/learn/health-and-wellness/menstruation/how-do-i-use-tampons-pads-and-menstrual-cups
- ↑ https://obgyn.coloradowomenshealth.com/health-info/teens/how-to-insert-tampon
- ↑ https://metro.co.uk/2017/01/17/applicator-vs-non-applicator-the-war-of-the-tampons-6386906/
- ↑ https://www.plannedparenthood.org/learn/teens/ask-experts/how-do-i-put-a-tampon-in
- ↑ https://obgyn.coloradowomenshealth.com/health-info/teens/how-to-insert-tampon
- ↑ https://www.plannedparenthood.org/learn/health-and-wellness/sexual-and-reproductive-anatomy/what-are-parts-female-sexual-anatomy
- ↑ https://www.plannedparenthood.org/learn/health-and-wellness/menstruation/how-do-i-use-tampons-pads-and-menstrual-cups
- ↑ https://obgyn.coloradowomenshealth.com/health-info/teens/how-to-insert-tampon
- ↑ https://obgyn.coloradowomenshealth.com/health-info/teens/how-to-insert-tampon
- ↑ https://kidshealth.org/en/kids/pads-tampons.html
- ↑ https://kidshealth.org/en/teens/supplies.html
- ↑ https://kidshealth.org/en/kids/pads-tampons.html
- ↑ https://www.nhs.uk/common-health-questions/womens-health/what-if-i-forget-to-remove-my-tampon/
- ↑ https://kidshealth.org/en/teens/supplies.html
- ↑ http://www.acog.org/Patients/FAQs/Your-First-Period-Especially-for-Teens
- ↑ http://kidshealth.org/kid/talk/qa/when_period.html
- ↑ https://www.acog.org/womens-health/faqs/your-first-period?utm_source=redirect&utm_medium=web&utm_campaign=otn
- ↑ http://www.acog.org/Patients/FAQs/Your-First-Period-Especially-for-Teens
- ↑ https://kidshealth.org/en/teens/irregular-periods.html
- ↑ http://www.mayoclinic.org/healthy-lifestyle/tween-and-teen-health/in-depth/menstruation/art-20046004?pg=2
- ↑ https://www.nhs.uk/common-health-questions/womens-health/can-a-tampon-get-lost-inside-me/
- ↑ https://kidshealth.org/en/teens/use-tampon.html
- ↑ https://www.plannedparenthood.org/learn/health-and-wellness/menstruation/how-do-i-use-tampons-pads-and-menstrual-cups
- ↑ https://www.kidshealth.org/en/kids/when-period.html