This article was co-authored by Anthony Stark, EMR. Anthony Stark is a certified EMR (Emergency Medical Responder) in British Columbia, Canada. With over 11 years of experience, he has worked as an industrial medic and provided urban and rural paramedic services. He currently works for Mountain View Safety Services and previously worked for the British Columbia Ambulance Service. Anthony has a Bachelor of Engineering in Electrical, Electronics, and Communications Engineering from the Georgia Institute of Technology. He has completed the EMP Canada EMT Course and Swiftwater Awareness Training associated with the British Columbia Ambulance Service.
This article has been viewed 197,267 times.
Steps
Measuring Someone's Breathing Rate
-
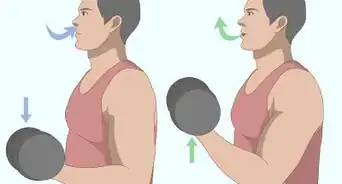
1Count the breaths. Breathing is measured in breaths per minute or bpm. To get an accurate measurement, the person must be at rest. This means she is not breathing faster than usual due to exercising. She should be still for at least 10 minutes before you count her breaths.[3]
- Have the person sit up straight. If you are measuring an infant, lay the baby flat on her back on a firm surface.
- Use a stop watch to time one minute. Count the number of times the person's chest rises and falls during that minute.
- If you tell the person that you are going to measure her breathing, she is likely to change her breathing rate without realizing it. Tell her to breathe normally. To improve the accuracy of your result, you can take the measurement three times and average the answers.
- If you are pressed for time, count the breaths in a 15 second window, then multiply the number of breaths by 4. This gives a close approximation of breaths per minute and is useful in emergency situations.
-
2Determine whether the breathing rate is within the normal range. Children breathe faster than adults so you need to compare your number to the normal number of breaths per minute for the person's age group. The rates are as follows[4]
- 30 to 60 bpm for an infant who is 0 to 6 months old
- 24 to 30 bpm for an infant who is 6 to 12 months old
- 20 to 30 bpm for a child who is 1 to 5 years old
- 12 to 20 for a child who is 6 to 11 years old
- 12 to 18 for someone who is 12 or older
Advertisement -
3Look for signs of respiratory distress. If someone's breathing rate is higher or lower than the expected range, and she has not been exercising, this could be an indication that something is wrong. Other signs of respiratory distress include:
- Flaring the nostrils during each breath.
- The skin has a dusky color.
- The ribs and center of the chest are pulled in.
- The person makes a wheezing, grunting, or crying sound when breathing.
- The person's lips and/or eyelids are blue.
- The person is breathing with their entire shoulders/chest area. This is considered labored breathing.
-
4Check breaths per minute as needed. If you are with an individual and the breathing rate needs to be taken frequently, then try re-taking it every 15 minutes for non emergency cases. If the person is in an emergency situation, then check their breaths per minute every 5 minutes.
- Checking the person's breaths per minute can give you early warning signs of deteriorating conditions, shock, or other changes.
- If possible, try to keep a record of the person's breaths per minute in case you go to the hospital.
Getting Medical Help
-
1
-
2Get breathing assistance. If someone needs help breathing, there are several ways that a doctor can administer oxygen. This includes:
- An oxygen mask. This is a mask that fits over the person's face and delivers a higher concentration of oxygen than is present in the atmosphere. In the environment, the air is 21% oxygen. But if someone is having trouble breathing, they may need a higher concentration.
- CPAP or continuous positive airway pressure. Tubes are put into the person's nose and oxygen flows in under a small amount of air pressure. The pressure helps the airways and the lungs stay open.
- Ventilation. This involves putting a breathing tube down through the person's mouth and into the windpipe. Oxygen can then be administered directly into the lungs.
-
3Avoid hyperventilation due to anxiety. Some people breathe very quickly, called hyperventilation, when they are anxious or panicking. This can lead to the feeling of not being able to catch your breath even though you are getting too much oxygen while breathing too fast. If someone you are with experiences this you can:[7]
- Reassure the person and help her relax. Tell her that she is not having a heart attack and is not going to die. Assure her that she is doing ok.
- Have the person adopt breathing techniques that will reduce the amount of oxygen she gets. She can: breathe into a paper bag, purse her lips, or cover one nostril and her mouth while breathing. As the balance of carbon dioxide and oxygen in her system returns to normal, she should feel better.
- You can also help the person to relax by advising them to concentrate on a single object on the horizon, such as a tree or building. Or, you can also tell them to close their eyes to ease the sense of panic the person might feel.
- Encourage the person to see a doctor.
References
- ↑ http://www.hopkinsmedicine.org/healthlibrary/conditions/cardiovascular_diseases/vital_signs_body_temperature_pulse_rate_respiration_rate_blood_pressure_85,P00866/
- ↑ https://my.clevelandclinic.org/health/healthy_living/hic_Pre-participation_Evaluations/hic_Vital_Signs
- ↑ http://www.hopkinsmedicine.org/healthlibrary/conditions/cardiovascular_diseases/vital_signs_body_temperature_pulse_rate_respiration_rate_blood_pressure_85,P00866/
- ↑ https://www.health.ny.gov/professionals/ems/pdf/assmttools.pdf
- ↑ https://my.clevelandclinic.org/health/healthy_living/hic_Pre-participation_Evaluations/hic_Vital_Signs
- ↑ http://www.hopkinsmedicine.org/healthlibrary/conditions/cardiovascular_diseases/vital_signs_body_temperature_pulse_rate_respiration_rate_blood_pressure_85,P00866/
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/003071.htm
-Step-1-Version-4.webp)
-Step-2-Version-4.webp)
-Step-3-Version-4.webp)

-Step-4-Version-4.webp)
-Step-5-Version-4.webp)
-Step-6-Version-4.webp)





























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...