This article was co-authored by Carrie Noriega, MD. Dr. Noriega is a Board Certified Obstetrician & Gynecologist and medical writer in Colorado. She specializes in women’s health, rheumatology, pulmonology, infectious disease, and gastroenterology. She received her MD from the Creighton School of Medicine in Omaha, Nebraska and completed her residency at the University of Missouri - Kansas City in 2005.
There are 27 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 59,851 times.
According to the Centers for Disease Control and Prevention (CDC), breast cancer is the leading cause of death for American women. Breast cancer is easier to treat when detected early, which makes breast awareness key to ensuring breast health. There are a number of ways you can check the health of your breasts and uncover potential abnormalities.[1] You should also be aware that although it is uncommon, men can get breast cancer, so if you are a male and have seen any changes in your breast tissue, see a doctor immediately.[2]
Steps
Performing a Breast Self-Exam
-
1Increase your breast awareness. Get comfortable with your breasts and be aware of what their "normal" state is. "Normal" is unique for each woman, but get to know how your breasts generally look and feel. Establish a familiarity with them and their texture, contours, size, etc. You’ll be better able to recognize any changes and then communicate those changes to your physician. In addition, becoming more aware can help you feel empowered as you take an active role in your own health and well-being.[3]
- Increasing breast awareness is one of the best things you can do for yourself if you are concerned about breast cancer. By becoming aware of what is normal for you, you'll be better able to assess when something is abnormal.[4]
- Note that even things like breast asymmetry, where one breast is a slightly different size or in a slightly different position, are generally completely normal.[5] You generally should only have cause for concern if things change from the way they usually are (for example, one breast grows significantly larger, etc.).
- If you have a spouse or partner, make him or her part of the process of checking your breasts and becoming more aware of your breast tissue. This is especially important because your partner sees and touches your body from a different angle and may be able to see things that you cannot. Ask your partner to communicate any changes s/he may notice or feel.
-
2Understand that the issue of breast self-examination is a subject of debate. In the past, a monthly breast self-examination (BSE) was recommended for all women. However, in 2009 the US Preventative Services Task Force recommended against teaching women to do consistent and formal self-examinations after several large research studies concluded that BSE didn't reduce mortality or increase the number of cancers found. Subsequent studies have confirmed that BSE is of no importance in detecting malignant lesions in the breasts.[6] [7]
- At present, the American Cancer Society and the US Preventative Services Task Force recommend that BSE should be done at your own discretion. These organizations also emphasize that the real key is to be aware of what is normal for your own breast tissue.[8]
- Part of the pushback against BSE is because it can lead to unnecessary testing (such as a biopsy), which can cause harm to the patient as well as a financial burden on the healthcare system. The problem is that BSE may draw attention to benign lesions, whereas mammograms can identify those malignant lesions that are real cause for concern and medical treatment.[9]
- Be aware as well that a BSE should never be done in lieu of a physician's clinical examination or mammogram. At best, doing a BSE can help you become more aware of what is normal in your breasts and can help you assist your doctor in detecting changes.[10]
Advertisement -
3Know what to look for. There are a number of signs that you should be aware of when visually or manually checking your breasts for cancer, including the following:[11]
- Changes in breast size or shape - Swelling from a tumor or infection can change the shape and size of the breast tissue. This often occurs only on one breast but in some cases can occur on both. Your breasts may also change size during certain times in your menstrual cycle, so having an idea of what is "normal" for you at any particular time of the month is helpful.
- Discharge from the nipple - If you're not breastfeeding, there should be no discharge coming from the nipple. If there is discharge, especially without squeezing the nipple or breast tissue, talk to your physician.
- Swelling - There are aggressive and invasive types of breast cancer that may cause swelling in breast, collarbone or armpit. In some cases, the swelling occurs before you can feel a lump.
- Dimpling - Tumors or growths in the breast near the surface of the skin or nipple can cause a change in shape and look of the tissue, including dimpling or puckering of the skin (like the skin of an orange, also known as peau d'orange). Look as well for a newly inverted nipple, which is also a sign of a problem.[12] (Some women have naturally inverted nipples, which are not a cause for concern; a change from your normal state is.)
- Redness, warmth or itching - Inflammatory breast cancer is a rare but aggressive type of cancer that presents with symptoms similar to an infection in the breast: a warming sensation, itching or redness.
-
4Do a visual BSE. You can do this whenever you like, although it's a good idea to do it after your period, when your breasts are less tender and swollen. Try to do it every month at around the same time. You can even mark down when you do the exam each month in your planner or journal to keep track of it.[13]
- In front of a mirror, sit or stand without a shirt or bra on. Lift and lower your arms. Look for any changes to the size, shape, tenderness, and appearance of your breast tissue, using the above signs as your guide.
- Then place your palms on your hips and flex your chest muscles. Look for any dimples, puckers or other abnormalities.
-
5Do a manual BSE. Devote a set time each month to do a manual BSE. If you are still menstruating, the best time to do this is a few days after your period when your breasts are the least tender. You can do the examination lying down; in this position, the breast tissue is more spread out and thus thinner and easier to feel. Another alternative is in the shower, where the soap and water can help your fingers move more smoothly over your breast skin. You can also do both methods, in order to maximize the examination.[14] Follow these steps:
- Lie flat and place your right hand behind your head. Using the first three fingers of your left hand, palpate (feel) the breast tissue on your right breast. Be sure to use the pads of the fingers, not just the very tips. Feel for anything that feels hard and round.
- Start at your armpit area and work your way towards the center of each breast. Move across to the middle of your body until you only feel the sternum (breastbone).
- Use three different levels of pressure to feel the tissue: light pressure at the top for tissue just under the skin, medium pressure to check tissue in the middle of the breast, and deeper pressure to feel the tissue closest to the chest wall. Make sure to apply each pressure level to each area before moving on.
- Once you've done one breast, do the other. Put your left hand under your head and perform the same exam on your left breast.
- Squeeze each nipple gently to check for discharge.
- Remember that your breast tissue extends to the area near your armpit. This area can also develop lumps or cancer, so it's important to check there as there during your manual BSE.[15]
Scheduling Clinical Breast Exams
-
1Schedule annual "well woman exams". These are yearly physical or pelvic exams with your gynecologist or family practitioner. You should see the doctor every year for a checkup, even if you are feeling fine. This is especially important as you age and your risk for developing certain cancers, including breast cancer, increases.[16]
- During the beginning of the exam, give your doctor an updated medical history. Breast cancer is often hereditary, so your breast exams will be even more important if there is a history of breast cancer in your family, particularly among a mother or sister.
-
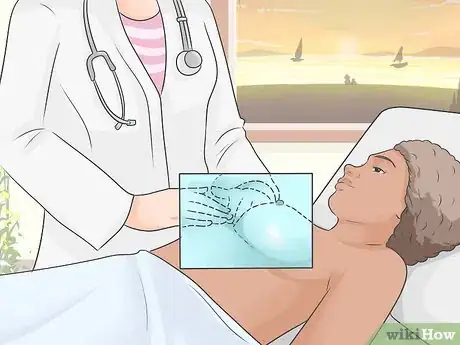
2Get a clinical breast exam. During your yearly physical or pelvic exam, your physician will do a manual check of your breasts for any suspicious lumps or other changes. If your doctor doesn't do this, ask for it. Physicians are trained in how to do a breast exam and will know what to look for and what should be cause for concern. This is why you should never try to replace this exam with your own self-examination.[17]
- If you feel uncomfortable, you can ask for a nurse or family member to be present during the exam. If you’re a female patient seeing a male doctor, this is typically standard procedure.
-
3Have the appearance of your breasts assessed. Your doctor will begin by checking the appearance of your breasts. You will be asked to raise your arms over your head and then hang them down by your sides while the doctor examines the size and shape of your breasts.[18]
- The doctor is not judging your breasts on any aesthetic qualities. She is only checking to see whether they are generally the same shape and size, or if there are any areas for concern.
-
4Undergo a physical examination. While you lie down on the examination table, your doctor will use the pads of her fingers to examine the entire breast area, including the armpits and collarbones. The exam should last for only for a few minutes.[19]
-
5Stay calm and breathe. If you feel any anxiety, take a deep breath and remind yourself that this is a necessary part of maintaining and being proactive about your health.
- Remind yourself as well that breast cancer has a higher success rate of being treated effectively when it is caught early and before it has spread to other organs, tissues, and the bones.
- Remember that you can always ask any questions about why your doctor is performing certain motions or exams. If you feel stressed out or uncomfortable, talk with your doctor.
Getting a Screening Mammogram
-
1Schedule an annual mammogram when you turn 40. The National Breast Cancer Foundation recommends a screening mammogram every one to two years for women aged 40 and older. If you have a personal or family history of breast cancer or you notice a lump during a self-exam, your doctor may want you to begin having screening mammograms before you are 40 years old.[20]
- Screen mammography for women aged 75 and older depends on the woman’s overall health. If she has a number of health problems, she is not likely not to be a candidate for treatment were cancer in fact detected. Thus, you should talk to your doctor about screening if you are 75 or older.[21]
- For women who know via genetic testing that they carry the breast cancer genetic mutation (BRCA1 and BRCA2), screening should begin at age 25 and may also involve an MRI of the breast tissue in addition to a mammogram.[22]
-
2Understand what the procedure does. A mammogram is an low-radiation x-ray that allows doctors to see your breast tissue. A mammogram can often detect lumps in your breast tissue before you can feel them.[23]
- Although the doctor may be looking for potential cancerous growth with a mammogram, the test can also detect calcifications, fibroadenomas and cysts in the breast tissue.[24]
-
3Prepare for your mammogram. Find out if there are any requirements before your mammogram. You should not wear deodorant, perfume or lotion on the day of your mammogram, as these can interfere with the test reading.[25]
- Be sure to wear a loose top that will be easy for you to take off for the mammogram.
- Read up on the procedure to help calm yourself if you feel anxious. The test may be slightly uncomfortable but is over within a matter of minutes.
-
4Discuss your breasts with your doctor and the mammogram technician. They will need to know if you have breast implants, or if you are currently menstruating.[26]
-
5Have the test. In the mammogram, your breast is placed on a platform and compressed with a paddle to even out the breast tissue, hold the tissue still during the x-ray, and allow for the use of a lower-energy x-ray.[27]
- You’ll feel pressure and may experience some discomfort during the mammogram, but this is just temporary.
- A mammogram will be done on both breasts so the radiologist can compare both sides.
-
6Wait for results. If the potential for breast cancer shows up in your results, you might need have further imaging testing, such as a breast ultrasound to look for cysts or an MRI to evaluate and differentiate a suspicious lesion from a benign one.[28]
- If the mammogram and MRI detect a tumor or growth, your doctor may recommend an ultrasound-guided needle biopsy to determine both the type of cell growth and the type of treatment needed to treat the cancer (i.e., surgery, chemotherapy, radiation, etc.). In a biopsy, tissue is removed from the suspicious area of the breast and analyzed in a laboratory. Most breast tissue biopsies are outpatient procedures, and you won’t have to stay overnight in a hospital.[29]
Knowing Your Risk Factors
-
1Be aware of the basic risk factors for breast cancer. Although being a woman is the main risk factor developing breast cancer, there are also a number of other factors that increase the likelihood that you could develop breast cancer, including:[30]
- Age: Risk increase with age. Most people who have breast cancer are over 45 years old. Once you reach the age of 50, your risk increases ten-fold for each decade beyond 50.
- Menstruation: If you started menstruating before you were 12 years old, or entered menopause when you were older than 55, your risk is slightly increased. In both cases, the risk is higher because of the increased ovulation cycles.
- Pregnancy: An early pregnancy or multiple pregnancies can both reduce your risk. Having no children or getting pregnant after the age of 40 increases your risk of developing breast cancer.
- Hormone replacement therapy (HRT): Current or previous use for more than 10 years can increase the risk for breast cancer.
-
2Be aware that your lifestyle can affect your breast cancer risk. Obesity, smoking, alcohol use, and shift work are all risk factors for breast cancer.[31]
- Whether someone is overweight or obese is determined by using the body mass index (BMI). BMI is a person's weight in kilograms (kg) divided by the square of the person's height in meters (m). A BMI of 25-29.9 is considered overweight, while a BMI greater than 30 is considered obese. A BMI greater than 30 is considered a risk factor for developing breast cancer, since fat cells secrete estrogen, which feeds many breast cancers.
- There is also some recent evidence that long-term heavy smoking correlates with a higher risk of breast cancer. The risk is especially high among certain groups of smokers, such as women who began smoking before they had their first child. Research is still being conducted to determine the exact relationship between smoking and breast cancer.
- Alcohol has also been linked to increased risk of developing breast cancer. The risk increases the more you drink alcohol. Women who consume between two and five drinks every day have a 1.5x higher risk than women who don't drink.
- Recent research has suggested that women who work night shifts (such as nurses) may have an increased risk of breast cancer due to changes in melatonin levels. Further research is needed, however, before these findings will be considered conclusive.
-
3Know your personal and family medical history. There are also risk factors related specifically to you, your family history, and your genetics, including:[32]
- Personal medical history: If you have had a previous diagnosis of breast cancer, you are three to four times as likely to develop a new cancer in the same or opposite breast.
- Family history: You are more likely to develop breast cancer if one or more close blood relatives in your family have had breast, ovarian, uterine or colon cancer. Your risk is doubled if you have a first-degree relative (sister, mother, daughter) with the disease. Having two first-degree relatives triples your risk.
- Genes: Genetic defects found on BRCA1 and BRCA 2 can dramatically increase your risk of developing breast cancer. You can opt to find out if you have these genes by contacting a genome mapping service. In general, approximately 5-10% of cases are related to heredity.
-
4Be aware that most women diagnosed with breast cancer have NO risk factors. The majority of women don't exhibit any of the above and are no more or less likely to breast cancer than anyone else.[33] As a result it is imperative that women practice the above guidelines regarding breast health and that they notify their primary care physicians if they notice any changes in their breast tissue.[34]
Warnings
- Always consult a physician for diagnosis. You cannot diagnose breast cancer at home or based on your own self-examination. So before you get too worried or concerned, get the answers you need to make the right decisions.⧼thumbs_response⧽
References
- ↑ http://www.cdc.gov/cancer/breast/index.htm
- ↑ http://www.cancer.org/cancer/breastcancerinmen/detailedguide/breast-cancer-in-men-detection
- ↑ https://www.breastcancer.org/screening-testing/breast-self-exam-bse
- ↑ https://www.nhs.uk/common-health-questions/womens-health/how-should-i-check-my-breasts/
- ↑ http://www.healthywomen.org/content/ask-expert/1293/uneven-breasts
- ↑ MARIA TRIA TIRONA, MD,Breast Cancer Screening Update American Fam Physician. 2013 Feb 15;87(4):274-2780
- ↑ http://www.cdc.gov/cancer/breast/basic_info/screening.htm
- ↑ https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html
- ↑ Tiffany L. Allen, MSN, FNP-BC, WHNP, Brittany J. Van Groningen, MSN, WHNP,Debra J. Barksdale, PhD, FNP-BC, CNE, FAANP et al The Breast Self-Examination Controversy: What Providers and Patients Should Know, Journal of Nurse Practitioners, June 2010Volume 6, Issue 6, Pages 444–451.
- ↑ https://www.cdc.gov/cancer/breast/basic_info/screening.htm
- ↑ https://medlineplus.gov/ency/article/001993.htm
- ↑ http://www.breastcancer.org/questions/bc_signs
- ↑ https://my.clevelandclinic.org/health/diagnostics/3990-breast-self-exam
- ↑ https://www.breastcancer.org/screening-testing/breast-self-exam-bse
- ↑ https://www.breastcancer.org/screening-testing/breast-self-exam-bse
- ↑ https://www.plannedparenthood.org/learn/health-and-wellness/wellness-visit
- ↑ http://www.nationalbreastcancer.org/breast-cancer-symptoms-and-signs
- ↑ https://www.plannedparenthood.org/learn/cancer/breast-cancer/what-breast-exam
- ↑ http://www.nationalbreastcancer.org/clinical-breast-exam
- ↑ http://www.nationalbreastcancer.org/mammogram
- ↑ MARIA TRIA TIRONA, MD,Breast Cancer Screening Update American Fam Physician. 2013 Feb 15;87(4):274-2780
- ↑ MARIA TRIA TIRONA, MD,Breast Cancer Screening Update American Fam Physician. 2013 Feb 15;87(4):274-2780
- ↑ http://www.nationalbreastcancer.org/mammogram
- ↑ https://www.breastcancer.org/screening-testing/mammograms/what-mammograms-show
- ↑ https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/mammograms-what-to-know-before-you-go.html
- ↑ https://www.breastscreen.nsw.gov.au/your-mammogram-appointment/screening-and-breast-implants/
- ↑ https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/mammogram-basics.html
- ↑ http://www.nationalbreastcancer.org/mammogram
- ↑ http://www.nationalbreastcancer.org/breast-cancer-biopsy
- ↑ https://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm
- ↑ https://www.cancer.org/cancer/breast-cancer/risk-and-prevention/lifestyle-related-breast-cancer-risk-factors.html
- ↑ https://www.cancer.org/cancer/breast-cancer/risk-and-prevention/breast-cancer-risk-factors-you-cannot-change.html
- ↑ https://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm
- ↑ CDC Recommendations for Breast Cancer Screening, 2015.
- ↑ http://www.cancer.org/cancer/breastcancerinmen/detailedguide/breast-cancer-in-men-detection
About This Article
To check for breast cancer, one of the best things you can do is become familiar with how your breasts normally look and feel so that you're aware if anything changes. Then, you'll be able to communicate any changes to your doctor. Some changes that you should keep an eye out for include changes in your breast size or shape, swelling, dimpling, discharge from your nipple, redness, warmth, or itching. In addition to monitoring your breasts for any changes, it's important that you get a yearly clinical breast exam since physicians are trained in what to look for. For more advice from our Medical co-author, like how to schedule breast exams and mammograms, scroll down!











































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...