This article was co-authored by Rebecca Levy-Gantt, MPT, DO. Dr. Rebecca Levy-Gantt is a board certified Obstetrician and Gynecologist running a private practice based in Napa, California. Dr. Levy-Gantt specializes in menopause, peri-menopause and hormonal management, including bio-Identical and compounded hormone treatments and alternative treatments. She is also a Nationally Certified Menopause Practitioner and is on the national listing of physicians who specialize in menopausal management. She received a Masters of Physical Therapy from Boston University and a Doctor of Osteopathic Medicine (DO) from the New York College of Osteopathic Medicine.
This article has been viewed 67,827 times.
Vaginoplasty is a surgical procedure that tightens the vaginal muscles. It may be done alone or along with labiaplasty – plastic surgery that changes the shape or size of the vaginal lips, usually for cosmetic reasons. Although vaginoplasty, labiaplasty, and related “vaginal rejuvenation” surgeries have become increasingly popular, many gynecologists believe they are often performed unnecessarily. Make sure that you give sufficient consideration to the risks involved. If you are thinking of getting vaginoplasty, there are a number of factors to consider.
Steps
Evaluating Your Symptoms
-
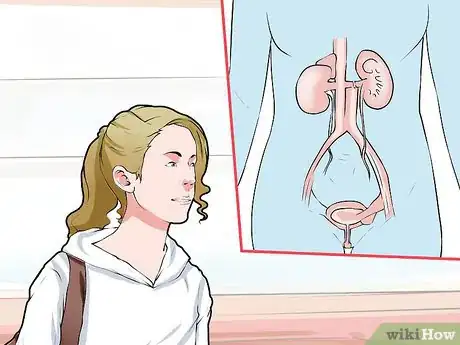
1Consider the health of your bladder. You should know that vaginoplasty can treat a prolapsed bladder. The muscles of the vagina play a crucial role in holding pelvic organs in place. When your vaginal muscles slacken, they may not do so effectively, and one of the potential consequences is a cystocele, or prolapsed bladder. This is a condition, fairly common in women, in which the bladder sinks into the vagina. If you have a prolapsed bladder, your doctor may recommend vaginoplasty as a solution.[1]
- Cystoceles are divided into categories based on severity. In Grade 1, or “mild” cases, only a small part of the bladder descends into the vagina. These cases may not need any treatment at all, unless they cause troubling symptoms.
- In Grade 2, or “moderate” cases, the bladder descends far enough into the vagina to touch the vaginal opening. In Grade 3, or “severe” cases, the bladder descends so far that it actually begins to protrude through the vaginal opening.
- If you are considering vaginoplasty for a prolapsed bladder, understand that less invasive treatments may work for you, especially if your case is not severe.
-
2Find a solution for slackened vaginal muscles. Some women who don’t have bladder pursue vaginoplasty as a solution for vaginal muscles that have become extremely weak. If your vaginal muscles have slackened to the point at which medical problems might result, your doctor may suggest vaginoplasty. Depending on the severity of your condition, this surgery might seem like a good option for you.[2]
- There are many reasons that vaginal muscles can weaken over time. Childbirth is a common factor, as is going through menopause.
- Women can also experience weakened vaginal muscles as a complication from a previous surgery. Weak vaginal muscles can also be hereditary.
- Talk to your doctor if you are experiencing problems such as vaginal pain or incontinence. Make sure to discuss your options outside of surgery.
- Non-invasive options include using a pessary to hold the pelvic organs in place, taking estrogen replacement therapy, and doing Kegel exercises to strengthen the muscles of the pelvic floor
Advertisement -
3Think about surgery to enhance sexual satisfaction. Sex is an important part of a healthy lifestyle for many women. If your vaginal muscles become very weak, you may struggle to achieve orgasm or feel that your orgasms are less satisfying. Vaginoplasty tightens the muscles of the vagina, allowing them to contract more effectively.[3]
- Vaginoplasty can improve your sex life. However, this is not the main reason to seek surgery.
- Typically, enhanced pleasure from vaginoplasty is a side-effect from having the surgery for another medical issue. It is an important benefit of this surgery.
- Increased sexual pleasure can lead to greater self-confidence and reduced levels of stress. Talk to your doctor about your individual issues.
-
4Reflect on your motivations. Many women worry that their vaginas are too slack or “stretched out” as they age or after they have children. This is normal. It’s true that both age and childbirth can weaken the muscles of the vagina and make you feel a little “looser,”, but in most cases, this is not a severe medical issue.[4]
- The rise of “vaginal rejuvenation” as a cosmetic procedure has made many women feel that their vaginas need to be improved with surgery, but for most women, this is simply not the case.
- Many times, the problem effects your self-esteem more than anything else. Work with your partner to revive your sex life.
- Don't worry about what other people think. Having surgery because someone else says that you should is not a great reason.
- Unless you're experiencing discomfort when you do normal activities, there's usually no reason to undergo vaginoplasty.[5]
-
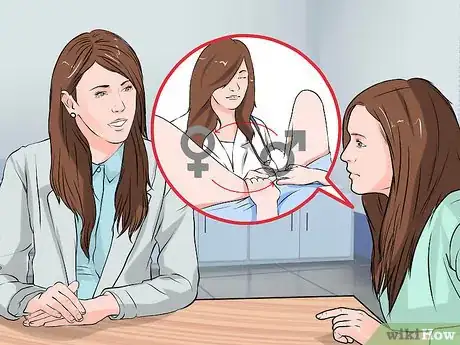
5Consider Gender Confirmation Surgery. If you are in the process of transitioning from male to female, you might want to consider surgery. To finalize the physical transition, many people choose to have a penile inversion vaginoplasty. Talk to your doctor about the process.[6]
- Make sure that you discuss the physical preparation for this surgery. You will need to be on hormone therapy for a period of time before having the surgery.
- Many doctors will recommend an extended course of counseling. This ensures that you understand the emotional connotations of having this surgery.
Weighing the Risks
-
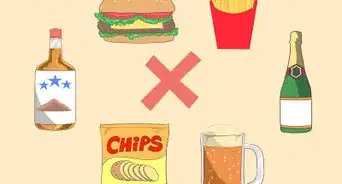
1Understand the risks of undergoing surgery. As with any surgical procedure, vaginoplasty has certain risks. For example, general anesthesia is something to discuss with your doctor. "Going under" during surgery carries its own risks.[7]
- Depending on your specific situation, you may need general anesthesia for your surgery. As with all surgeries done with general anesthesia, there are major risks. In rare cases, people undergoing surgery experience mental confusion, lung infections, strokes, heart attacks, and death.
- There are certain factors that increase your risk of complications. These include smoking, obesity, heavy alcohol use, and certain medications.
- Make sure to discuss your options with your doctor. In some cases, local anesthesia may be an option.
-
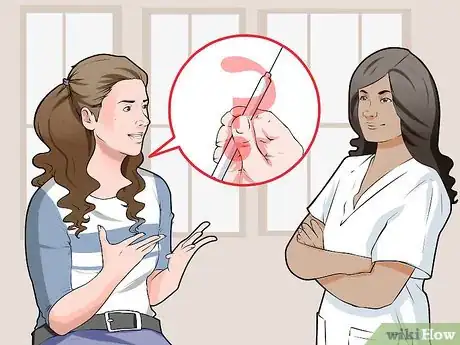
2Recognize the possibility of long-term side effects. In some cases, vaginal surgery creates more problems than it solves. Some women experience persistent pain and discomfort, either all the time or during sexual intercourse. Ask your doctor specific questions about your specific condition.
- Ask about your prospects for a successful surgery. Make sure you clearly explain your ideal outcome, and ask your doctor if this is possible.
- Talk to your doctor about how the surgery will affect your sex life. Specifically ask if orgasm will still be a possibility.
- Beware that infection is a possibility. If you undergo vaginoplasty, your surgeon will prescribe antibiotics to minimize the chance of developing an infection, but in a small number of women, infection can still occur.
-
3Be prepared for permanent changes in sensation. Ideally, vaginoplasty improves sensation and sexual function, but sometimes this does not occur. Some women report a decrease in sexual sensation. This is usually due to the normal scarring that occurs as a consequence of the surgery.[8]
- Ask your doctor if there are ways to reduce scarring. Don't be afraid to meet with more than one doctor.
- Think about how a change in sensation might effect your sex life. Is this something you are prepared for?
- Talk to your partner about possible changes. Weigh the pros and cons of surgery.
-
4Think about the recovery process. For most, the recovery process is fairly straightforward. However, it does take some planning. Know that it will be several weeks before you are back to full strength.[9]
- You will need to remain at the surgical center for at least several hours after the vaginoplasty. Most doctors will keep you overnight.
- You might experience severe pain and discomfort for several days. Ask your doctor about medications and other methods of managing pain.
- You will not be able to use tampons or have sexual intercourse for 4-6 weeks after your surgery. Your doctor will examine you before you are cleared to resume those activities.
- If you are undergoing gender confirmation surgery, the recovery process may be more intense. Talk to your doctor about how long you will need to plan to take off work and whether you will need help at home.
Pursuing Treatment
-
1Discuss your options with a gynecologist. No matter what your reasons are for pursuing surgery, you should discuss all of your options with a gynecologist. Your gynecologist can judge whether less invasive treatments might work (either as short-term fixes or long-term solutions) and make a final recommendation about vaginoplasty. He or she can also make sure you understand the risks and have realistic expectations about the results.
- Get a second opinion. If your gynecologist recommends vaginoplasty, consider seeing a second specialist. Don’t worry about offending your gynecologist; a good physician should understand – and even encourage – the desire to get a second opinion.
- Ask for recommendations. Friends, family, and even coworkers can point you in the direction of a trustworthy physician.
- Don't be afraid to ask questions about alternative treatments. It is unlikely that a doctor will pressure you to have surgery unless it is medically necessary, but be prepared to be your own advocate.
-
2Consider your future reproductive plans. If you plan to have children, it’s usually advisable to hold off on vaginoplasty. Unless you have a major medical complication, like a severe prolapse, ask your doctor for other treatment options. Additional vaginal births will stretch your muscles again, and undo some of the surgical results.
- Talk to your partner about your family plans. Have you discussed whether or not you will have children? Now is a good time to have that talk.
- If your doctor deems surgery a medical necessity, consider alternatives. You could later pursue surrogacy or adoption.
- Make sure that you discuss your reproductive plans with your doctor. That information could influence his recommendation.
-
3Discuss your plans with a therapist. If you are having trouble deciding, speak with a therapist. This is a good idea especially if you are considering vaginoplasty for sexual reasons or because you think it will increase your confidence or self esteem. A therapist can help you sort out your reasons and decide whether vaginoplasty is worth the risk.
- Some experts recommend that you consult a therapist even before you talk to a doctor. A good counselor can help you find your true motivations.
- Many women pursue vaginoplasty for cosmetic reasons. Your therapist can help you figure out the root cause of your desire for surgery.
- A therapist can also help you manage your expectations. You can also use this resource post-surgery, if you decide to have a vaginoplasty.
-
4Gather financial information. Many insurance companies consider vaginoplasty a cosmetic procedure. For this reason, many plans will not cover the cost of a vaginoplasty. Talk to your insurance provider about your specific coverage.
- If your surgery is a medical necessity, ask your doctor for advice. The hospital might have experience in these sorts of matters.
- Decide if you can pay out of pocket for the surgery. The cost is generally between $4500-8500.
- Talk to your doctor's office about payment plans and estimated costs. Then look at your budget to determine if the cost will work for you.
-
5Make the choice that feels right to you. Take your doctor’s advice into account, but know that unless there is a serious medical condition related to your vaginal muscles, you are really the only individual who can decide whether the benefits outweigh the risks. Make the decision that feels best to you. Once you have made your choice, move forward with confidence.
- Think about what is best for your body. If you think the surgery is worth it, go for it.
- Don't rush the decision. This is not a choice to be made on impulse.
Expert Q&A
-
QuestionWhen should you get a vaginoplasty?
 Rebecca Levy-Gantt, MPT, DODr. Rebecca Levy-Gantt is a board certified Obstetrician and Gynecologist running a private practice based in Napa, California. Dr. Levy-Gantt specializes in menopause, peri-menopause and hormonal management, including bio-Identical and compounded hormone treatments and alternative treatments. She is also a Nationally Certified Menopause Practitioner and is on the national listing of physicians who specialize in menopausal management. She received a Masters of Physical Therapy from Boston University and a Doctor of Osteopathic Medicine (DO) from the New York College of Osteopathic Medicine.
Rebecca Levy-Gantt, MPT, DODr. Rebecca Levy-Gantt is a board certified Obstetrician and Gynecologist running a private practice based in Napa, California. Dr. Levy-Gantt specializes in menopause, peri-menopause and hormonal management, including bio-Identical and compounded hormone treatments and alternative treatments. She is also a Nationally Certified Menopause Practitioner and is on the national listing of physicians who specialize in menopausal management. She received a Masters of Physical Therapy from Boston University and a Doctor of Osteopathic Medicine (DO) from the New York College of Osteopathic Medicine.
Board Certified Obstetrician & Gynecologist I tend to believe that you should never get a vaginoplasty purely for cosmetic reasons. There are a lot of self-conscious women out there that think there's something wrong with the way their vagina looks, but the truth is that there's a ton of variation out there. Even if you don't think you're normal, you probably are. Between photos women see online, porn, and media, there's a lot of incentive out there to feel bad about your body. You can't give into that feeling; the odds are extremely high that you're normal. That said, there are a few instances where it's a good idea to consider a vaginoplasty. In a very small number of women, there may be excess tissue down there that makes it hard to complete daily activities. If this is the case for you, talk to your doctor about a vaginoplasty!
I tend to believe that you should never get a vaginoplasty purely for cosmetic reasons. There are a lot of self-conscious women out there that think there's something wrong with the way their vagina looks, but the truth is that there's a ton of variation out there. Even if you don't think you're normal, you probably are. Between photos women see online, porn, and media, there's a lot of incentive out there to feel bad about your body. You can't give into that feeling; the odds are extremely high that you're normal. That said, there are a few instances where it's a good idea to consider a vaginoplasty. In a very small number of women, there may be excess tissue down there that makes it hard to complete daily activities. If this is the case for you, talk to your doctor about a vaginoplasty!
References
- ↑ https://my.clevelandclinic.org/health/diseases/15468-cystocele-fallen-bladder
- ↑ http://www.healthcentre.org.uk/cosmetic-surgery/vaginoplasty-reasons.html
- ↑ http://www.healthcentre.org.uk/cosmetic-surgery/vaginoplasty-reasons.html
- ↑ http://www.healthcentre.org.uk/cosmetic-surgery/vaginoplasty-reasons.html
- ↑ Rebecca Levy-Gantt, MPT, DO. Board Certified Obstetrician & Gynecologist. Expert Interview. 3 April 2020.
- ↑ https://my.clevelandclinic.org/health/treatments/21526-gender-affirmation-confirmation-or-sex-reassignment-surgery
- ↑ https://transcare.ucsf.edu/guidelines/vaginoplasty
- ↑ https://www.hopkinsmedicine.org/center-transgender-health/services-appointments/faq/vaginoplasty
- ↑ https://www.hopkinsmedicine.org/center-transgender-health/services-appointments/faq/vaginoplasty
About This Article
Before having vaginoplasty done, take time to evaluate your reasons for wanting the procedure. For example, you may need it to treat a medical condition, such as a prolapsed bladder, or you might be looking for ways to improve your sexual sensation. If you think that vaginoplasty is a good option for you, ask your doctor about the benefits and risks of the procedure. Keep in mind that you may experience some long-term side effects, such as chronic pain or permanent changes in sensation. Once you’re ready to take the next steps, talk to your doctor about the best treatment approach for you. Keep reading for more tips on how to make an informed decision about vaginoplasty!






























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...